Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
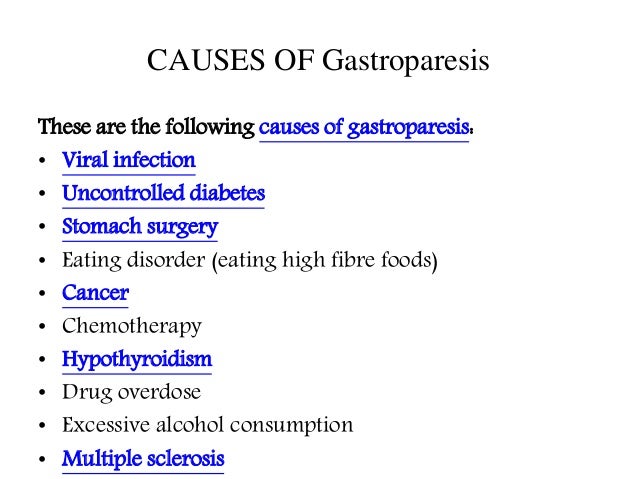 |  |
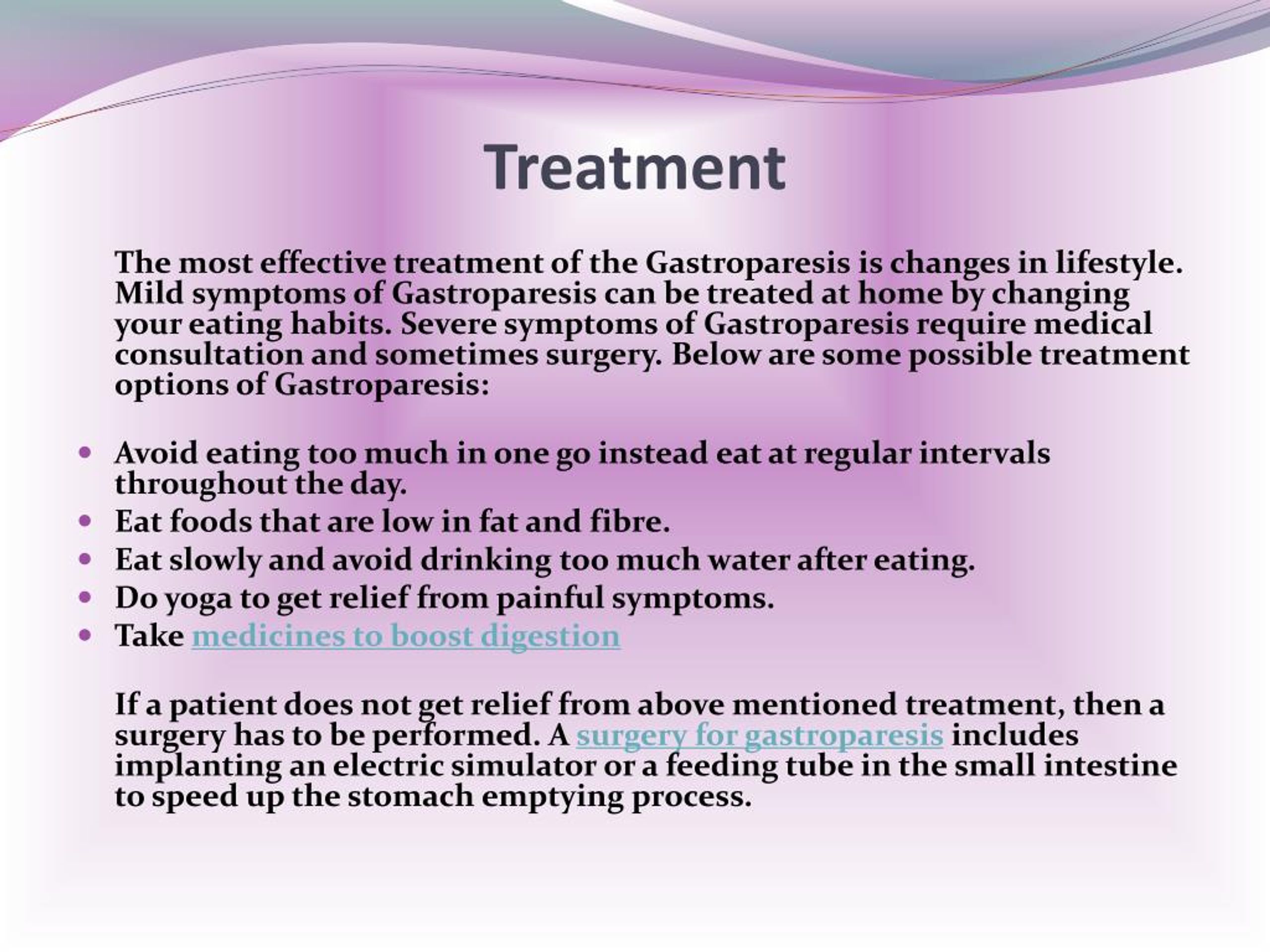
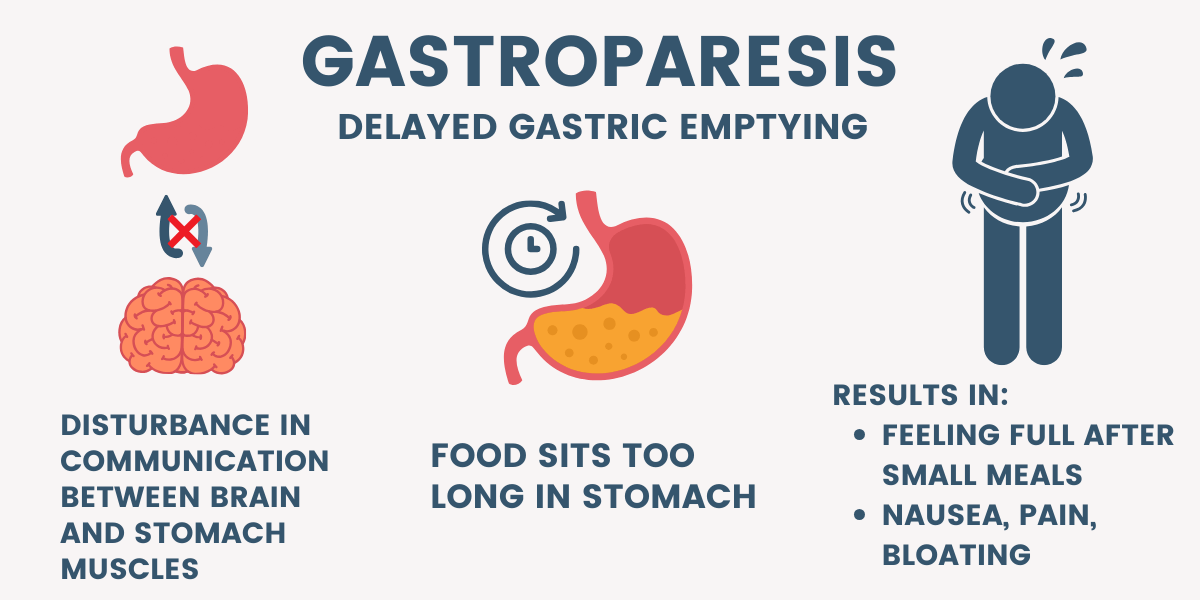
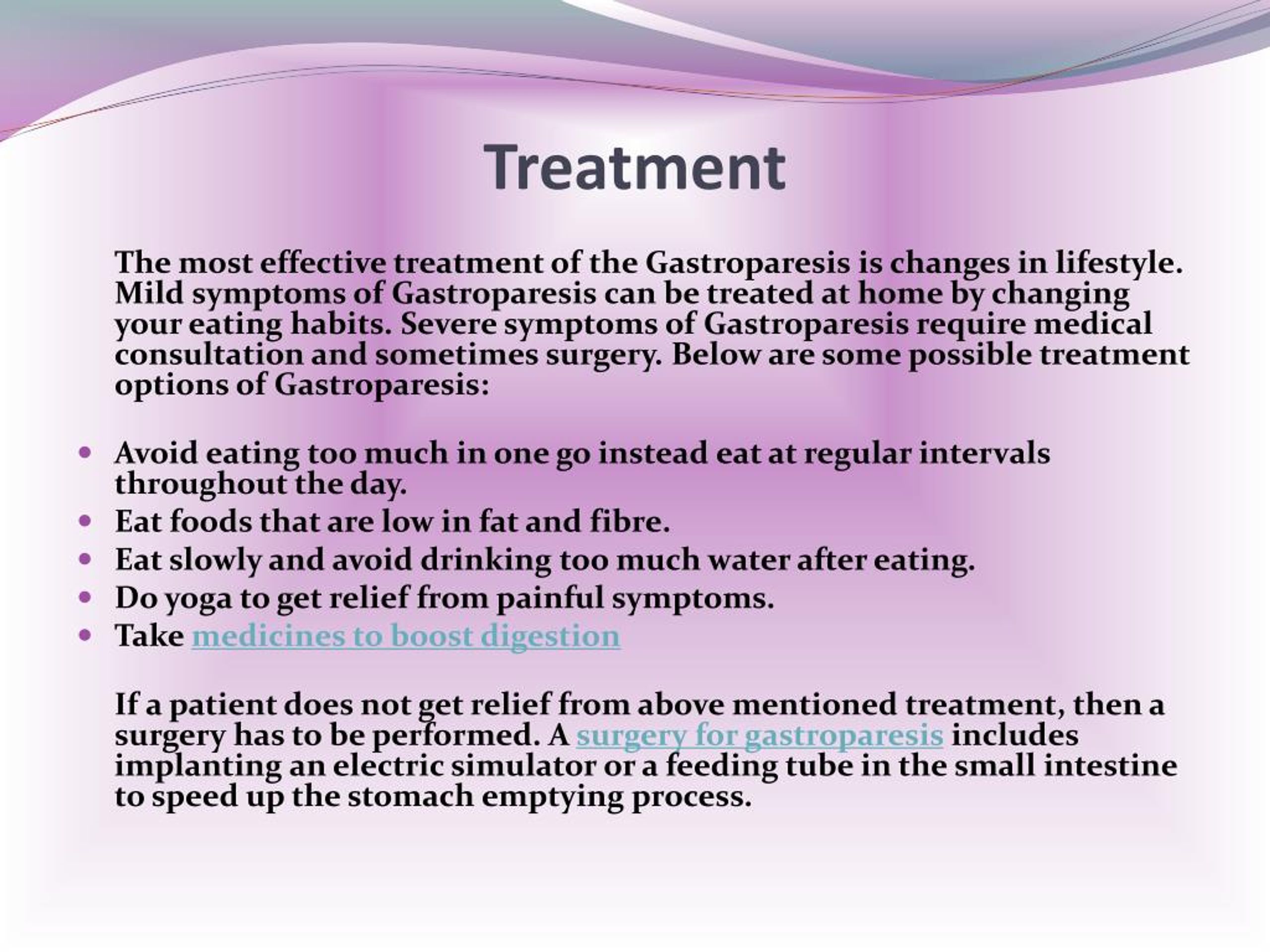
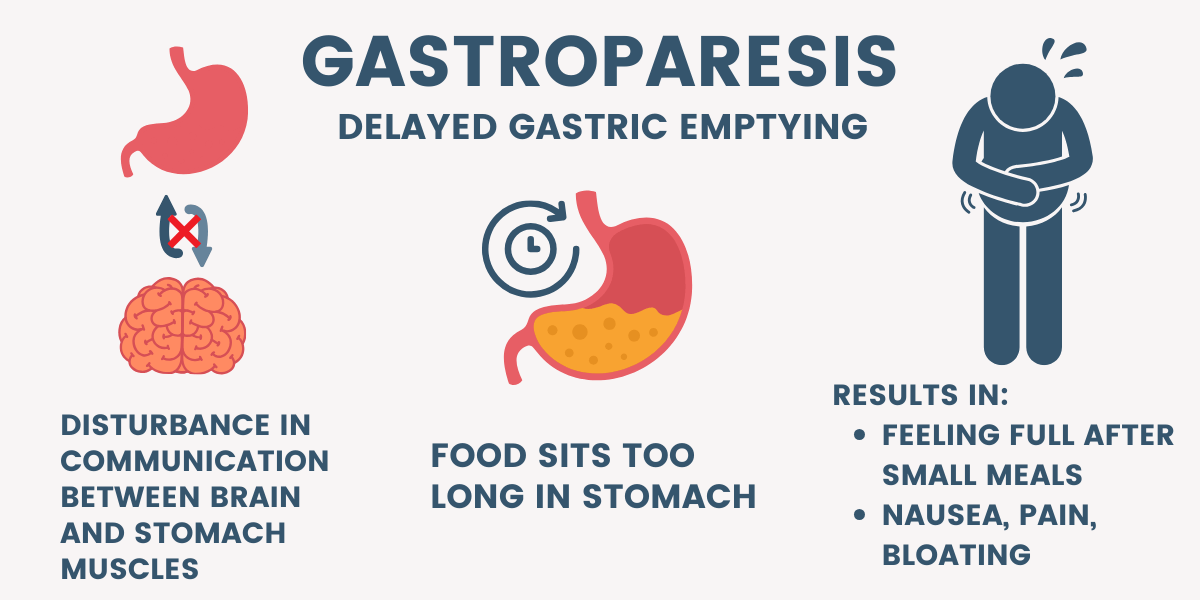
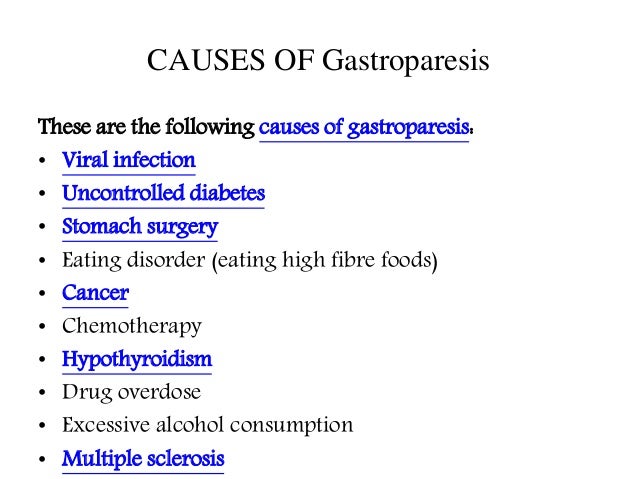
Several medications can delay gastric emptying and should be avoided with gastroparesis. However, most of the below-listed medications are vital to treat or prevent serious diseases. Don’t stop or change your medications without consulting your health care provider. Gabapentin as an adjunctive drug could be more effective in reducing the severity of GI symptoms in patients with dyspepsia, especially neurological symptoms (such as pain, reflux, and indigestion). Keywords: Functional dyspepsia, gabapentin, gastrointestinal disorders. Abstract. Gastroparesis (GP), a historically vexing disorder characterized by symptoms of nausea, vomiting, abdominal pain, early satiety, and/or bloating, in the setting of an objective delay in gastric emptying, is often difficult to treat and carries a tremendous burden on the quality of patients’ lives, as well as the healthcare system in general. These actually may worsen gastroparesis by impairing GI motility and are not recommended. Tramadol may be used in low doses and is a narcotic antagonist, which may be effective. If possible, however, try to use Gabapentin, Pregablin or tricyclics such as Nortriptyline for the abdominal pain in gastroparesis. Anticholinergics are one of the most common medication classes that “slow down” the GI tract which could obviously be a problem in this case. Looking into alternatives (depending upon the indication and benefit of amitriptyline) like SSRI’s (if depression), SNRI’s, or possibly increasing the gabapentin would all be potential options. Some side effects of gabapentin may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects. Gastroparesis is a syndrome defined by symptomatic delay in gastric emptying in the absence of mechanical obstruction. 1 Typical gastroparesis symptoms of nausea, vomiting, early satiety, bloating, postprandial fullness, abdominal pain, and/or weight loss overlap to a significant degree with functional dyspepsia (FD). 1–5 With an estimated prevalence per 100,000 persons of 37.8 for women and I'm on gabapentin (ostensibly) for my gastroparesis and have been for a number of years. I started at 25 mg three times a day, and gradually bumped up. My current dose is 800 mg once a day. The sleepiness was awful for the first week or so, and then again after each dose bump. Diabetic gastroparesis is reported as a side effect among people who take Gabapentin (gabapentin), especially for people who are female, 60+ old, also take Lantus, and have Gastroesophageal reflux disease. Other causes of gastroparesis include imbalances of minerals in the blood such as potassium, calcium, or magnesium, medications (such as narcotic pain-relievers), and thyroid disease. For a substantial number of patients, no cause can be found for gastroparesis, a condition termed idiopathic gastroparesis. DEFINITION OF GASTROPARESIS SYNDROME AND GASTROPARESIS SYMPTOMS Summary of Evidence. Gastroparesis is defined as a syndrome of objectively delayed gastric emptying in the absence of mechanical obstruction and cardinal symptoms including early satiety, postprandial fullness, nausea, vomiting, bloating, and upper abdominal pain (); the same constellation of complaints may be seen with other Gastroparesis is a syndrome characterized by delayed gastric emptying in the absence of any mechanical cause. It is estimated that gastroparesis affects up to 4% of the US population and inpatient care for patients with severe gastroparesis costs $7,000 per month [1]. In other words, gastroparesis is a relatively common disorder and comes with In a retrospective study of an FD cohort treated with gabapentin, there were significant improvements in dyspeptic symptoms evident as a significant reduction of mean patient assessment of GI disorder symptom severity index score by 0.44 (p<0.0001). 87 Likewise in a randomised clinical trial, 75 mg of pregabalin was associated with a reduction This page includes the following topics and synonyms: Medications that Delay Gastric Emptying, Drug-Induced Gastroparesis, Delayed Gastric Emptying due to Medications. Abstract. Gastroparesis (GP), a historically vexing disorder characterized by symptoms of nausea, vomiting, abdominal pain, early satiety, and/or bloating, in the setting of an objective delay in gastric emptying, is often difficult to treat and carries a tremendous burden on the quality of patients’ lives, as well as the healthcare system in general. Gastroparesis is a commonly diagnosed gastrointestinal disorder with a high prevalence globally and high disease burden to those afflicted with it. Etiologies are variable with idiopathic and diabetes being the most common causes of gastroparesis. Management of gastroparesis depends on the etiology, This case report discusses 2 cases of medication-induced gastroparesis which were initially diagnosed as diabetic gastroparesis, and thorough history taking revealed the cause to be medication induced. More rarely, gabapentin can cause fluid buildup (edema), weight gain, and vision problems. It can also cause diarrhea. More serious (but rare) side effects include suicidal thoughts or behavior, and mood changes in children. This could be exceeded in cases where gabapentin is well tolerated but there has not been complete improvement. 52 % of patients with functional dyspepsia responded to gabapentin based on change in total PAGI-SYM score. 61 % of patients with functional dyspepsia responded to gabapentin based on change in PAGI-SYM postprandial fullness subscore For example, while nausea is a predominant symptom in all patients with gastroparesis, vomiting is typically more prevalent and severe in patients with diabetic gastroparesis in comparison to other causes [2-4]. Less common symptoms such as postprandial fullness, upper abdominal pain, or abdominal distention may present as well.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |