Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 | :max_bytes(150000):strip_icc():format(webp)/GettyImages-1369889825-309a0c942f2c4ad0a5595047104135fb.jpg) |
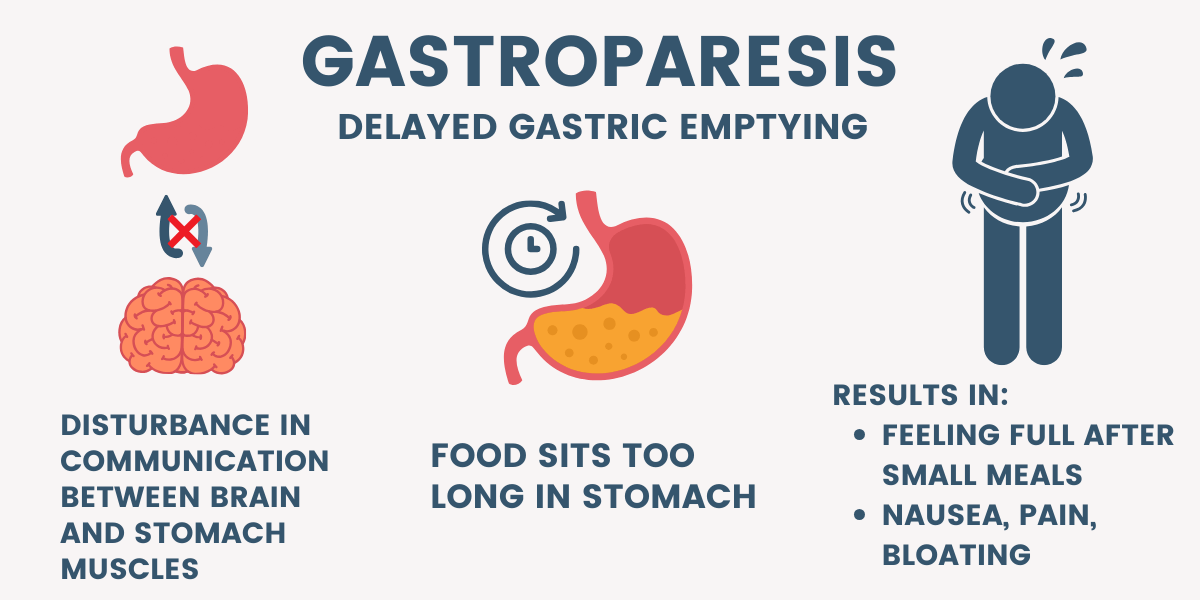 |  |
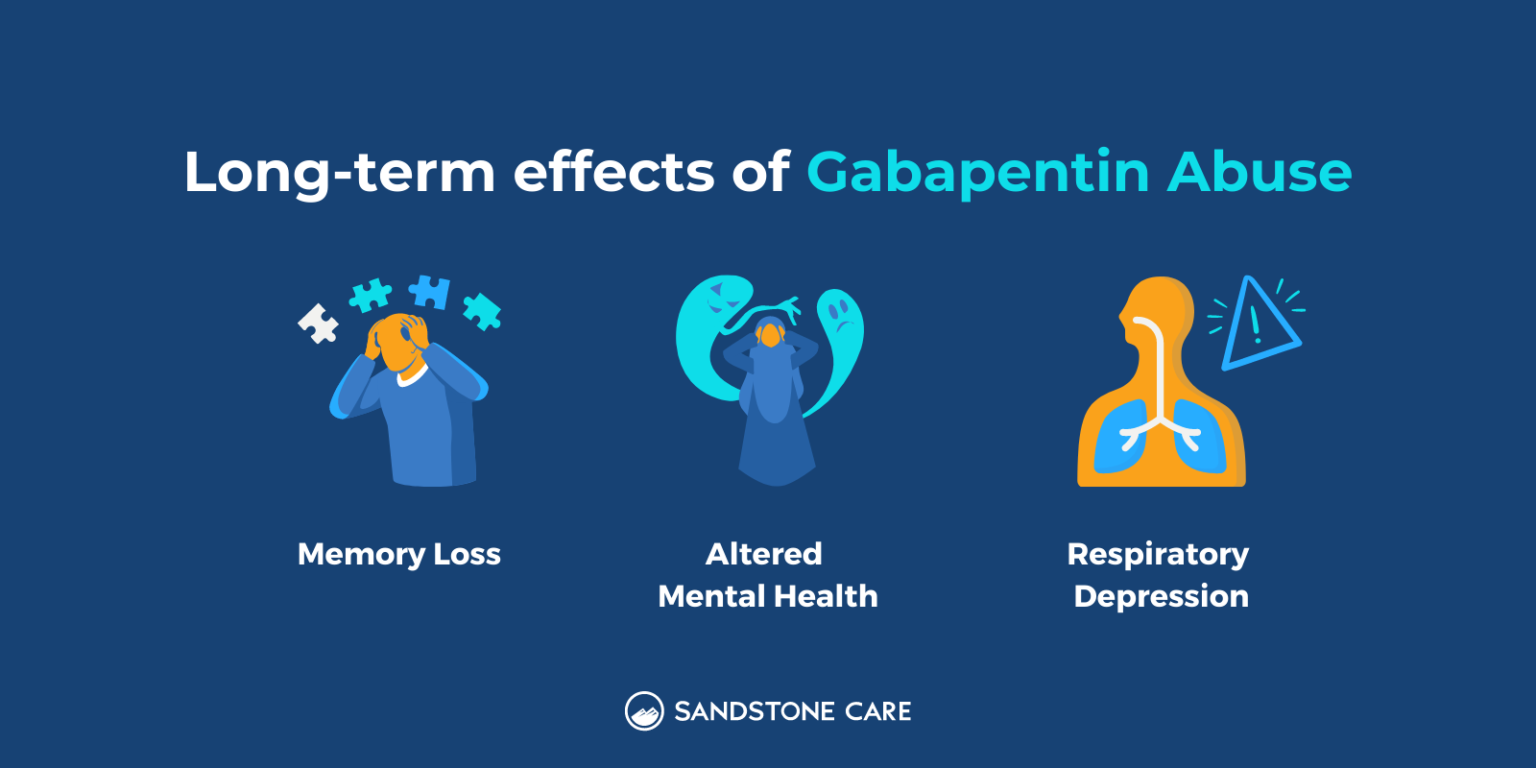
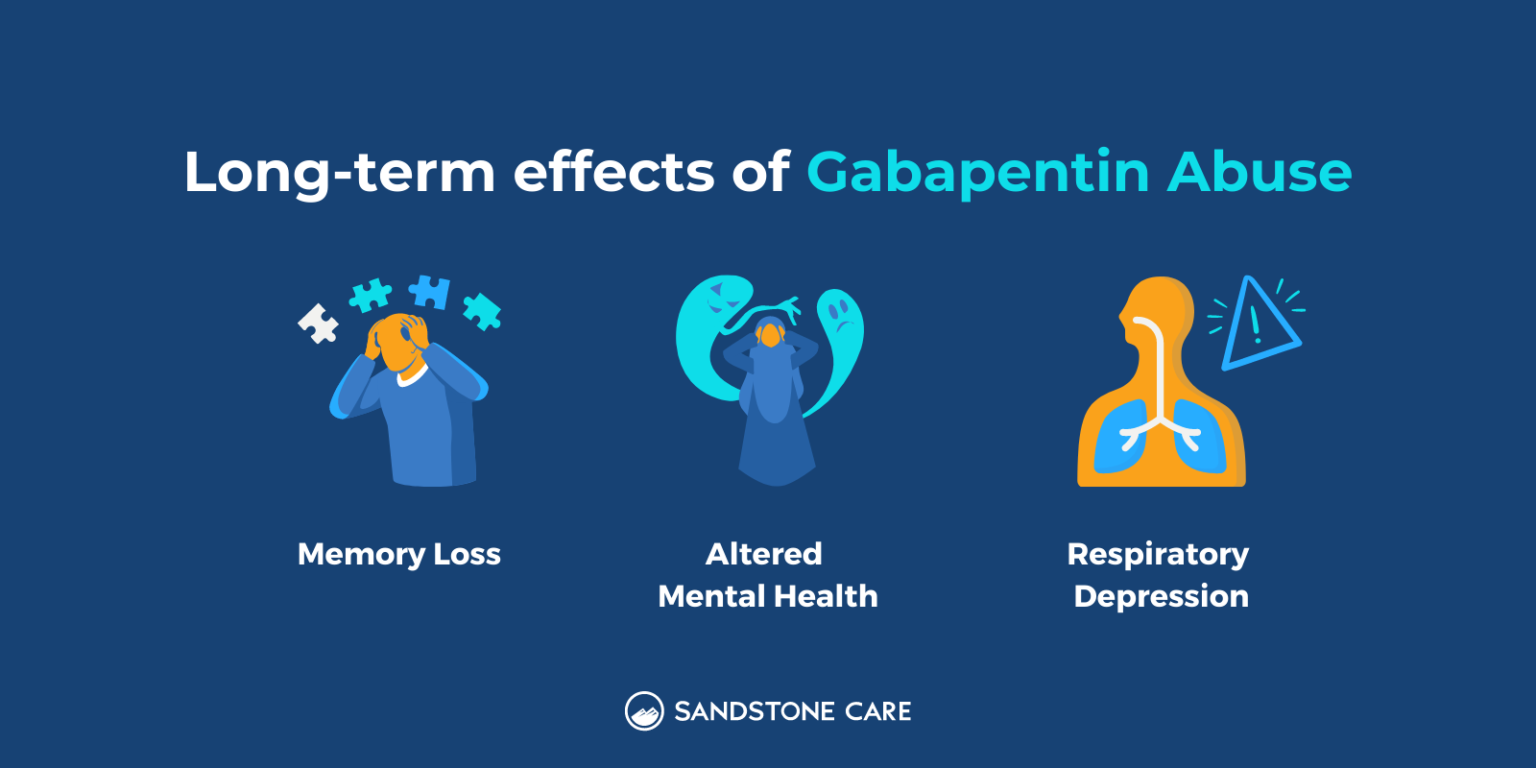
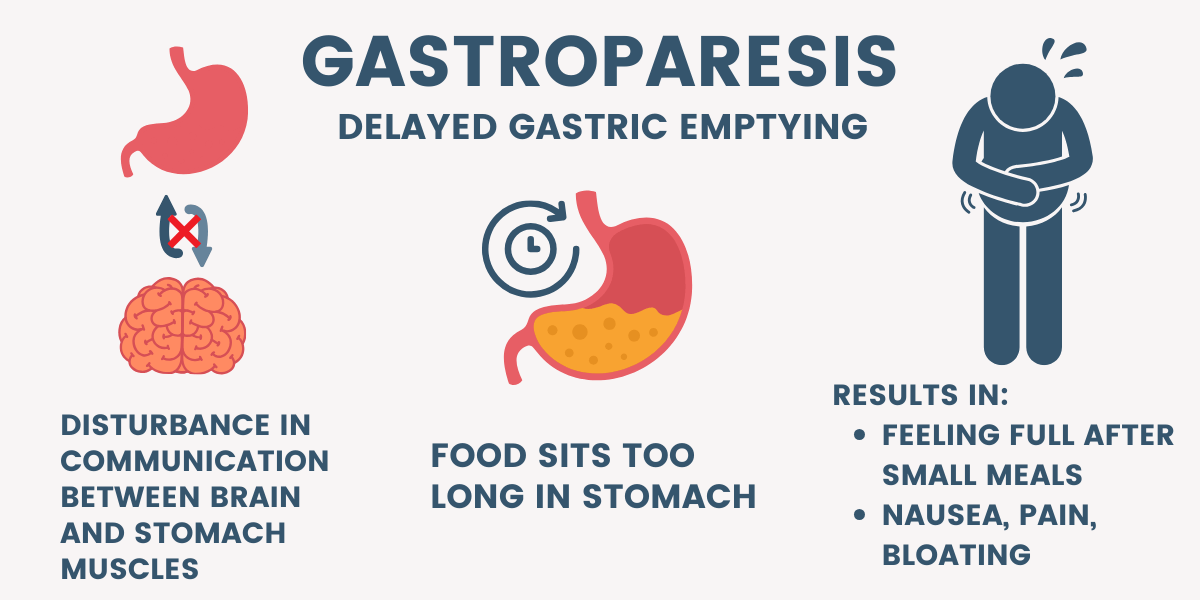
It is structurally related to gabapentin but has no activity at GABA or benzodiazepine receptors, though both pregabalin and gabapentin are frequently used to treat neuropathic pain. It can help improve spasms in the stomach muscles. Some studies show that the medicine decreases resistance in the muscles and improves gastric emptying and symptoms. Other studies showed that this treatment did not routinely benefit patients with gastroparesis. This page includes the following topics and synonyms: Medications that Delay Gastric Emptying, Drug-Induced Gastroparesis, Delayed Gastric Emptying due to Medications. If diabetes is causing your gastroparesis, your healthcare professional can work with you to help you control your blood sugar levels. Changes to your diet. Getting enough calories and nutrition while improving symptoms is the main goal in the treatment of gastroparesis. Many people can manage gastroparesis with dietary changes. Several medications can delay gastric emptying and should be avoided with gastroparesis. However, most of the below-listed medications are vital to treat or prevent serious diseases. Don’t stop or change your medications without consulting your health care provider. Delayed gastric emptying on objective testing defines gastroparesis, but symptoms overlap with functional dyspepsia and do not correlate well with gastric emptying delay. This review outlines a strategy for defining, diagnosing, and managing refractory gastroparesis. Additionally, the role of duodenal and distal gut mechanisms in gastroparesis warrants further investigation. It is possible that a combination of symptoms, molecular and physiological testing may help us identify subsets of gastroparesis patients which can be then targeted using specific treatments. Gastroparesis can be a serious problem where the GI tract literally “slows down”. This issue is common in patients with diabetes. Bloating, abdomnial pain, nausea, vomiting, and a feeling of fullness are all possible symptoms of gastroparesis. There are also medications that can worsen gastroparesis. The case: KD is a 62 year old female who [] I'm on gabapentin (ostensibly) for my gastroparesis and have been for a number of years. I started at 25 mg three times a day, and gradually bumped up. My current dose is 800 mg once a day. The sleepiness was awful for the first week or so, and then again after each dose bump. If possible, however, try to use Gabapentin, Pregablin or tricyclics such as Nortriptyline for the abdominal pain in gastroparesis. There are patients who are refractory to all types of treatment and cannot even take in sufficient calories and fluids. The pathophysiology behind gastroparesis is varied and depends on disease etiology. Vagal and/or autonomic neuropathy play an important role in the development of diabetic gastroparesis, and it is estimated to occur in up to 20% to 40% of patients with diabetes. Gastroparesis can cause problems with blood sugar levels and nutrition. Gabapentin can help alleviate the discomfort and frequent episodes of nausea and vomiting associated with gastroparesis. Improved digestion: By targeting the nervous system, Gabapentin can improve the function of the digestive system, allowing for better digestion and a decrease in bloating and abdominal pain. Pain relief DEFINITION OF GASTROPARESIS SYNDROME AND GASTROPARESIS SYMPTOMS Summary of Evidence. Gastroparesis is defined as a syndrome of objectively delayed gastric emptying in the absence of mechanical obstruction and cardinal symptoms including early satiety, postprandial fullness, nausea, vomiting, bloating, and upper abdominal pain (); the same constellation of complaints may be seen with other Gastroparesis is a syndrome characterized by delayed gastric emptying in the absence of any mechanical cause. While often associated with diabetes mellitus, most cases of gastroparesis are idiopathic. The purpose of the present paper is to review In a retrospective study of an FD cohort treated with gabapentin, there were significant improvements in dyspeptic symptoms evident as a significant reduction of mean patient assessment of GI disorder symptom severity index score by 0.44 (p<0.0001). 87 Likewise in a randomised clinical trial, 75 mg of pregabalin was associated with a reduction Discussion. Gastroparesis is a disease with variable presentations ranging from mild nausea and abdominal fullness to recurrent vomiting and abdominal pain symptoms. 4 The diagnosis requires evidence of delayed GE based on a radionuclide study using an isotope-labeled solid meal for 4-hour duration in addition to the absence of mechanical obstruction. Gabapentin as an adjunctive drug could be more effective in reducing the severity of GI symptoms in patients with dyspepsia, especially neurological symptoms (such as pain, reflux, and indigestion). Keywords: Functional dyspepsia, gabapentin, gastrointestinal disorders. Introduction Metoclopramide works for gastroparesis by helping the stomach muscles have better contractions. It also relaxes the area where food leaves the stomach. This helps food to pass into the intestines quicker. The usual dose of metoclopramide for gastroparesis is 10 mg by mouth 4 times daily. Idiopathic gastroparesis is the most common form, whereas diabetes accounts for approximately one-third of all cases of gastroparesis. 2 Other causes of nausea, vomiting, and postprandial distress symptoms (eg, early satiety, postprandial fullness, and epigastric pain) are excluded by standard endoscopy, routine laboratory studies, and computed Gastroenterologists at Massachusetts General Hospital have begun prescribing low-dose gabapentin for patients with functional dyspepsia because it is thought to be capable of relieving visceral pain.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 | :max_bytes(150000):strip_icc():format(webp)/GettyImages-1369889825-309a0c942f2c4ad0a5595047104135fb.jpg) |
 |  |