Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 | 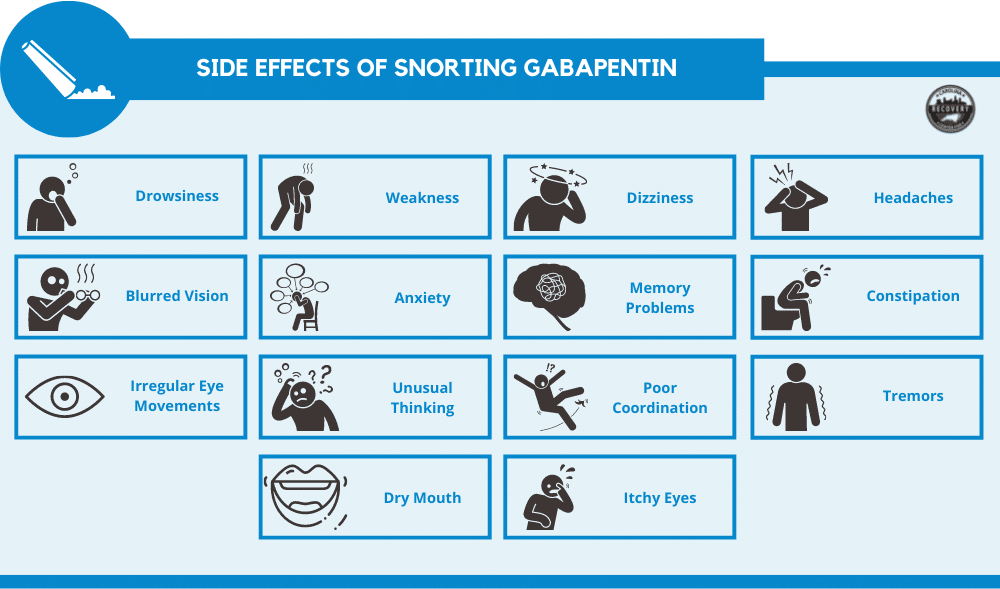 |
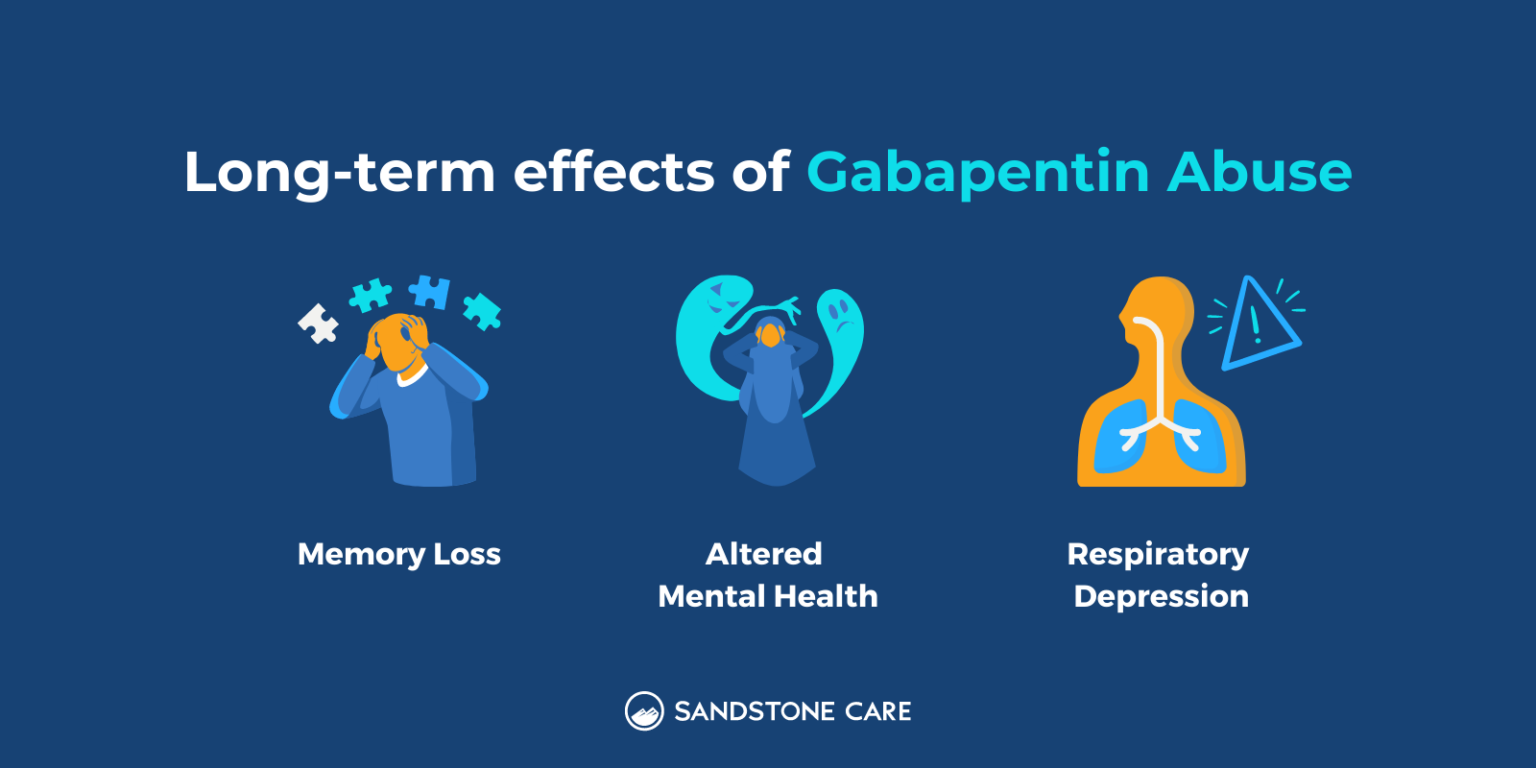
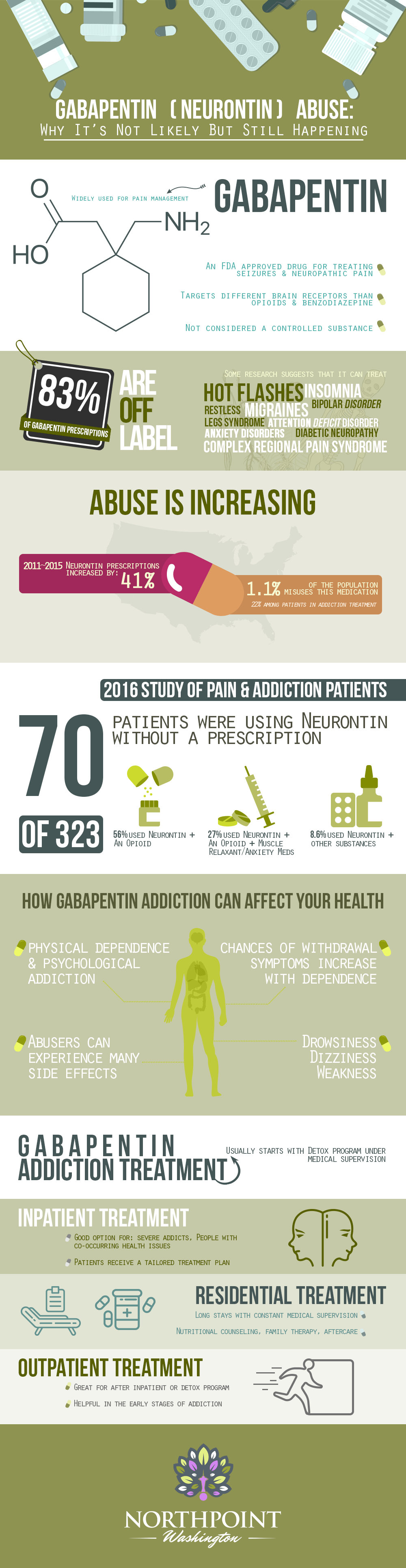
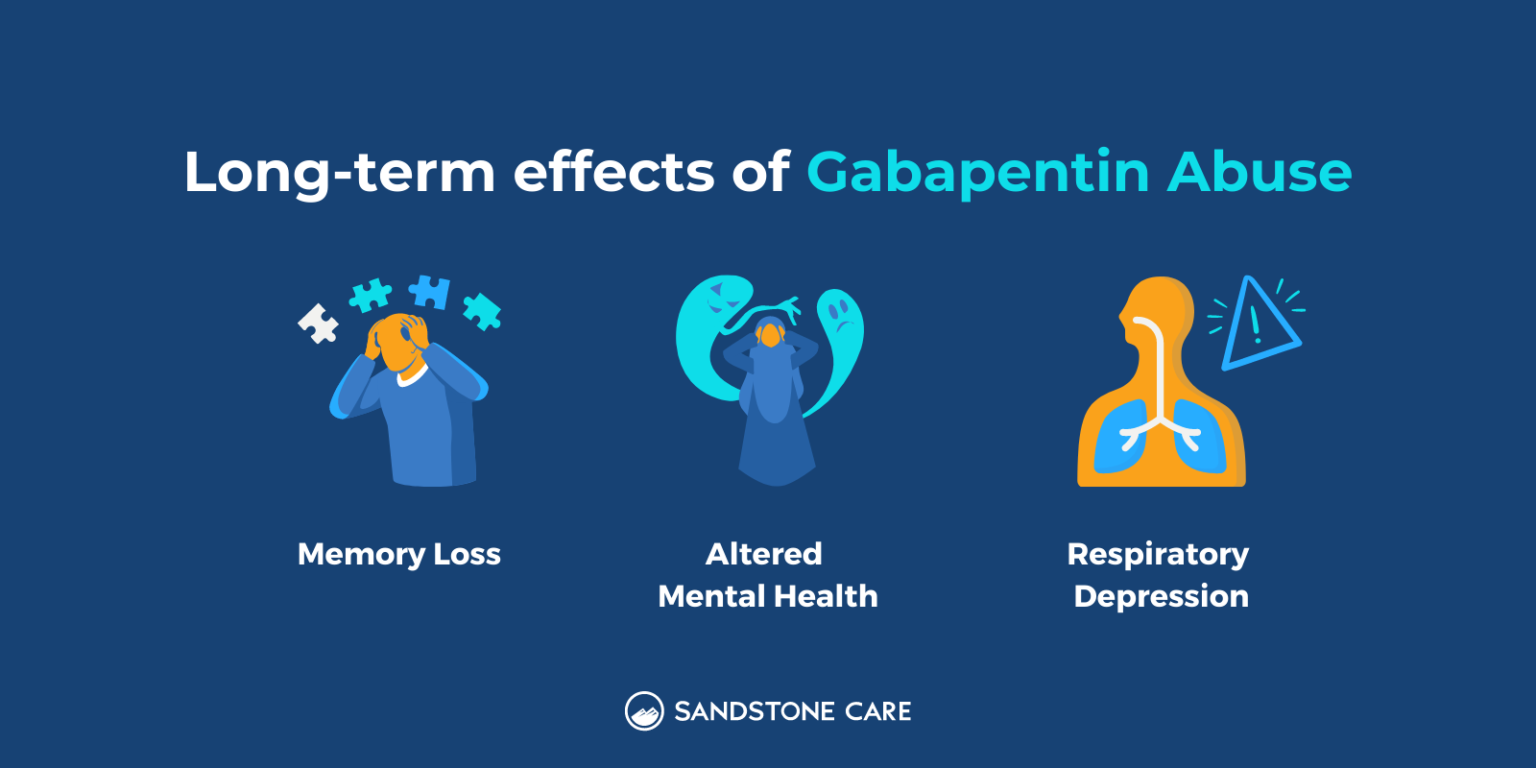
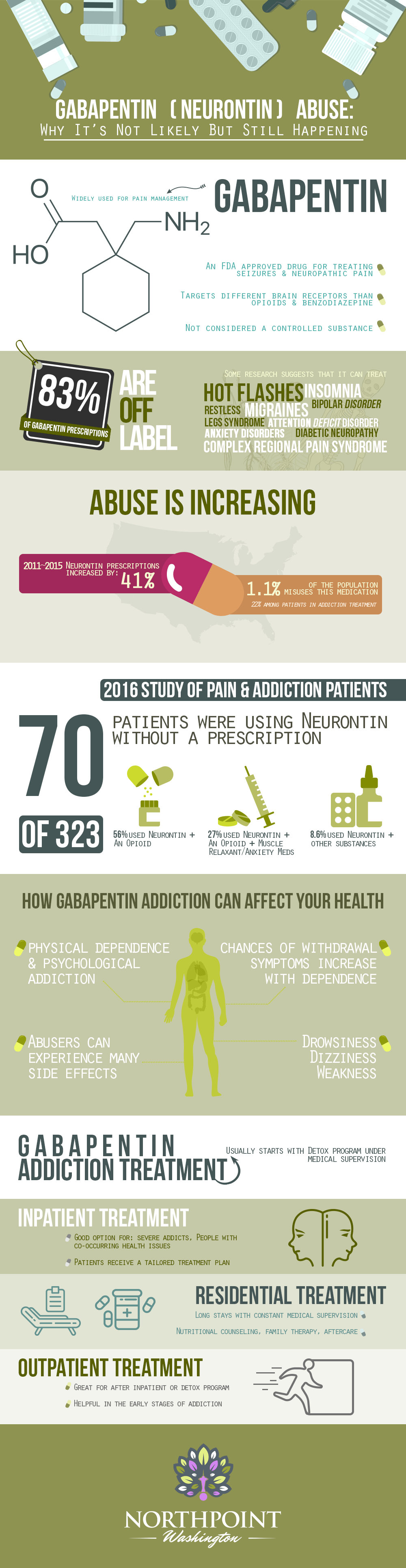
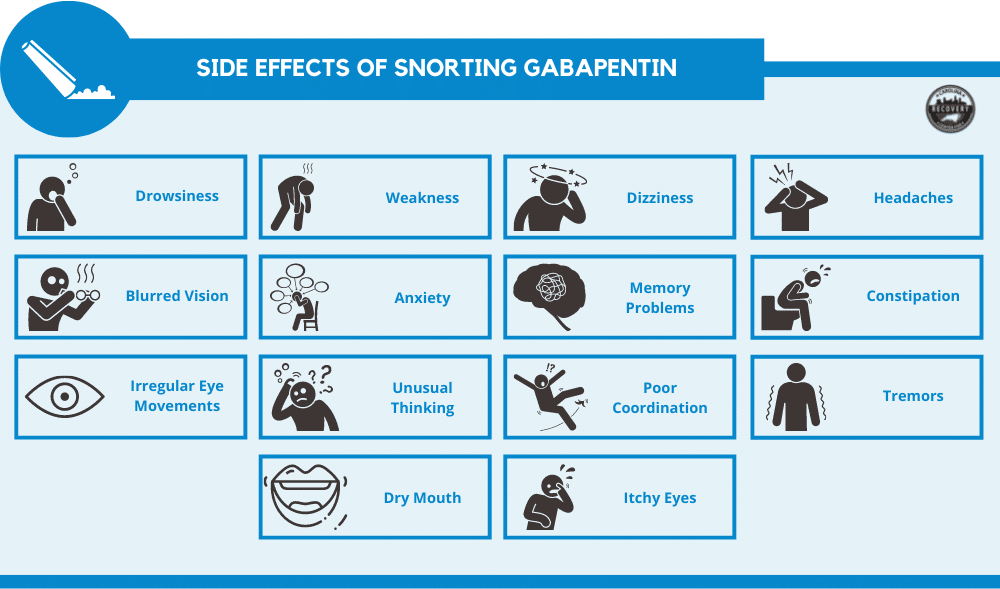
 |  |
The gabapentinoid group consists of gabapentin and pregabalin. Structurally similar to the inhibitory neurotransmitter GABA (gamma-aminobutyric acid), gabapentinoids bind to a subunit (protein α2-δ) of a voltage-dependent calcium channel in the central nervous system, decreasing the intracellular calcium influx induced by cell depolarization, and the release of exciting neurotransmitters. Gabapentin misuse occurred concomitantly with any opioid (44.9%), benzodiazepines (38.8%), alcohol (24.5%), and powder cocaine (24.5), among others. Gabapentin (Neurontin) carries a risk for abuse, can get you high if mixed with drugs, causes adverse side effects, and can lead to overdose. Many gabapentin users in early recovery abuse gabapentin because, at high doses (800mg or more), they may experience a euphoric-like high that does not show up on drug screens. Gabapentin abusers typically take the drug in addition to opioids to produce their desired high, a dangerous and potentially deadly combination. Gabapentin is one of the recommended mainstays of evidence-based treatment. 3. Unfortunately, our clinical experience suggests that gabapentin is now prevalent as a drug of abuse. The drug’s effects vary with the user, dosage, past experience, psychiatric history, and expectations. Epidemiological and case report evidence suggests that the anti-epileptic and analgesic medication gabapentin is being misused internationally, with substance abuse populations at special risk for misuse/abuse. Gabapentinoids have undergone extensive study as therapy for neuropathic pain due to promising molecular and clinical efficacy. However, the abuse potential of gabapentinoids requires further study, especially since these drugs are in widespread use. Background A 2017 systematic review (SR) identified 59 studies examining gabapentinoid (pregabalin and gabapentin) misuse/abuse. Evidence of gabapentinoid misuse/abuse has since grown substantially. Objective Update previous SR and describe new insights regarding gabapentinoid abuse. Methods A SR of PubMed was conducted to identify studies published from 7/29/2016–8/31/2020. Four searches Moreover, another investigation on former inmates (n=250) found a 16% lifetime prevalence of gabapentin misuse. 43 Furthermore, a strong relationship between opioid use disorder and gabapentin abuse was found; specifically, 26% of patients with opioid use disorder reported gabapentin abuse, but only 4% of patients without the opioid use Though gabapentin was initially marketed as a medication with low potential for abuse and is commonly thought to be safe and effective, a growing body of evidence highlights the potential risks of overprescribing the medication. The abuse potential of gabapentin is well documented; with gabapentin having been noted as an agent highly sought after for use in potentiating opioids. When combined with opioids, the risk of respiratory depression and opioid-related mortality Prescription drug misuse was reported in 62% of the patients and 16% reported misuse of gabapentin in the past. A significantly higher proportion of patients with an opioid use disorder (26%) endorsed gabapentin abuse compared with 4% of those without an opioid use disorder. Gabapentin has been shown to lead to dependence, addiction and withdrawal in some people, although when it was first approved in 1993 this risk was thought to be minimal. . Gabapentin has been increasingly associated with drug abuse, particularly in people who mix it with opioids, alcohol or other substanc This page will discuss what gabapentin is, side effects of the drug, its misuse liability, symptoms of gabapentin addiction, gabapentin withdrawal, and how a gabapentin rehab program can help with addiction recovery. Gabapentinoid abuse appears to be far more prevalent among current or past opioid abusers (one study identified a 1.1 and 0.5% rate of gabapentin and pregabalin abuse, respectively, among the general population aged 16–59 years in the UK, whereas studies of patients with opioid use disorders demonstrated much higher gabapentin (15–22%) and Gabapentin misuse was not observed in AUD studies, 2,4,5,16 but evidence indicates that patients with opioid use disorder, prisoners, and polydrug users are at high risk for gabapentin misuse. 39–41 In all cases, clinicians should monitor for red flags that may indicate abuse, such as missed appointments, early refill requests, demands for Abuse and misuse of pregabalin and gabapentin. Drugs. 2017;77(4):403-426. Peckham AM, Fairman KA, Sclar DA. All-cause and drug-related medical events associated with overuse of gabapentin and/or Two surveys reported that the misuse of gabapentin was 1.1% in the general population and 22% in drug abuse treatment centers. Withdrawal, when reported, occurred within 12 hours to 7 days of discontinuation of the medication. Conclusion: There have been numerous documented cases of gabapentin abuse, dependence, and withdrawal. Available evidence also suggests that abuse and misuse are more frequent in users of pregabalin compared with users of gabapentin. Health professionals and prescribers should be aware of the risk for misuse of pregabalin and gabapentin, which eventually could lead to abuse, substance dependence, and intoxications. Gabapentin was primarily misused for recreational purposes, self-medication, or intentional self-harm and was misused alone or in combination with other substances, especially opioids, benzodiazepines, and/or alcohol. Individuals with histories of drug abuse were most often involved in its misuse.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |