Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
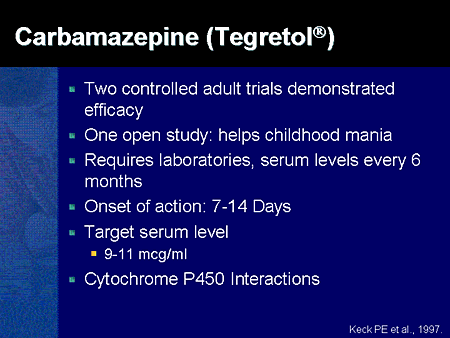
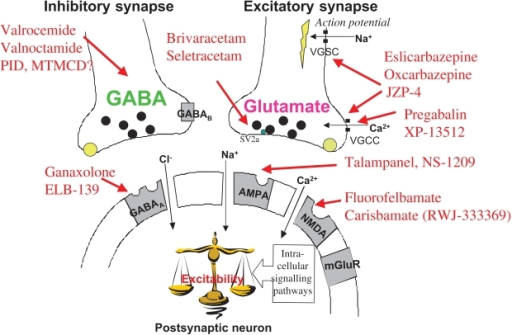
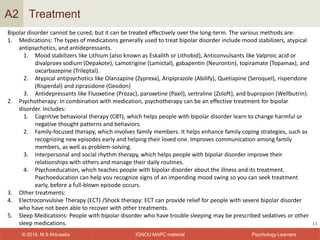
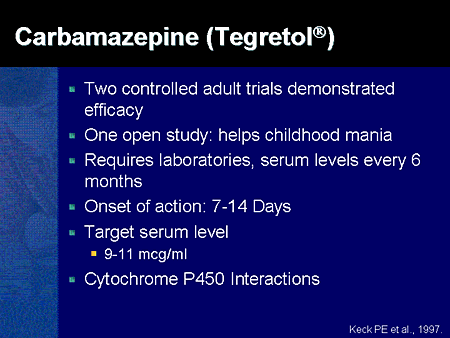
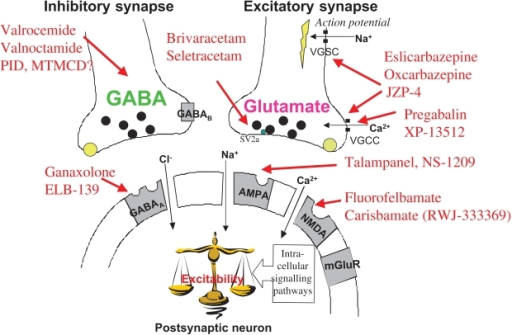
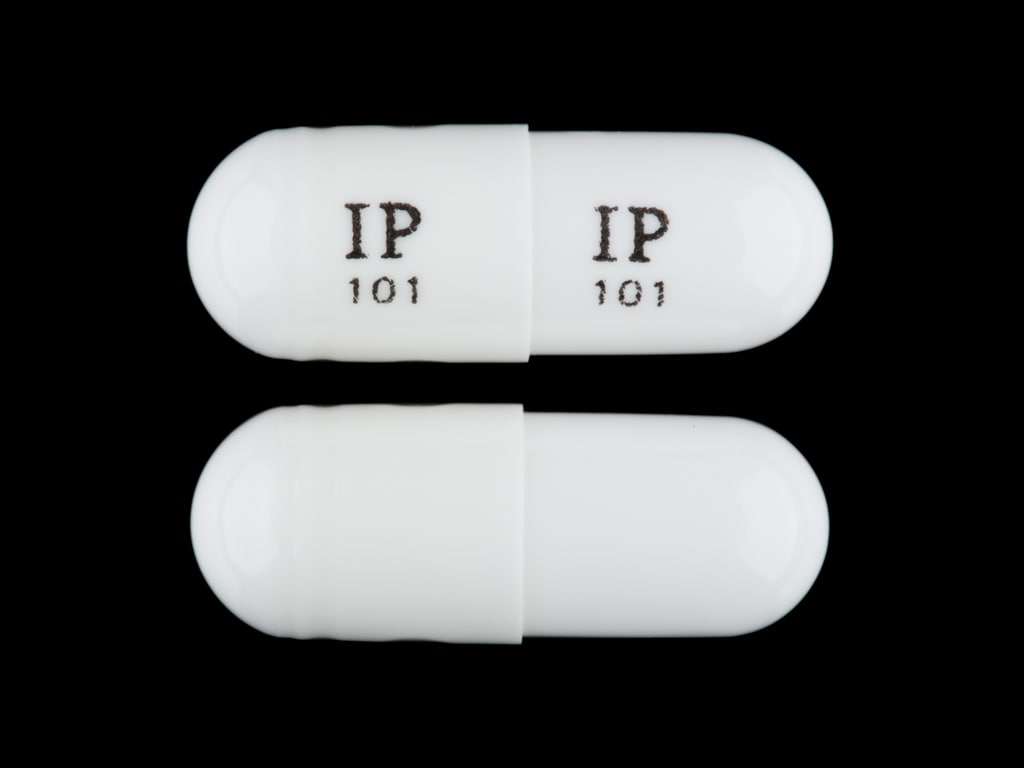
The use of gabapentin in bipolar disorder (BPD) treatment provides an informative case of off-label uptake and abandonment of a new medication. Gabapentin was patented by Warner-Lambert in 1977 and FDA-approved in December1993 for the adjunctive treatment of epilepsy and in 2002 for postherpetic neuralgia (see Appendix 1 for timeline). Researchers found that gabapentin does not help people with bipolar disorder. Learn more about the history of why some doctors prescribe gabapentin for bipolar as an adjunct therapy, even though there’s no evidence that it works for bipolar treatment or maintenance. Gabapentin was developed to create a γ-aminobutyric acid (GABA) neurotransmitter analog. 2 However, it exerts no GABA agonist effects and does not inhibit GABA uptake or degradation. 10 – 13 The most accepted molecular mechanism of gabapentin is binding at the α 2 δ 1 subunit of Ca 2+ channels affecting Ca 2+ currents. 14 – 16 The Medically Reviewed Gabapentin for Anxiety, Depression, and Bipolar Disorder. The prescription drug is being used off-label to treat common mental illnesses and even alcohol use disorder. Lithium and gabapentin. Gabapentin is currently being studied as a treatment for bipolar disorder, and there have been favorable reports regarding its potential as a mood stabilizer (82, 83). The advantages of gabapentin include the lack of interactions with other drugs in the cytochrome P450 system and the lack of protein binding . Since there Evidence does not support the use of gabapentin for bipolar disorder, major depressive disorder (MDD), posttraumatic stress disorder (PTSD), obsessive compulsive disorder (OCD), stimulant use disorder, or opioid withdrawal. Issue: Most patients with a bipolar spectrum disorder are treated with 2 or more drugs in combinations that are sometimes rational and evidence-based and sometimes not. a hot topic, with many new agents now available and many new combinations being touted. Prescribers wish that gabapentin had utility in bipolar disorder because gabapentin isn’t a P450 substrate, is renally excreted, and is generic and thus relatively affordable. Unfortunately, gabapentin does not demonstrate efficacy in randomized trials for bipolar disorder and current treatment guidelines do not emphasize its use. gabapentin (SMD -0.92, 95% CI -1.32 to -0.52) were more effective than placebo in reducing preoperative anxiety. In insomnia, results were inconclusive. Gabapentin and pregabalin have often been prescribed off-label in spite of a paucity of evidence and clinical practice guidelines to support its use. This systematic review aimed to synthesize Gabapentin may be a useful drug for the add-on treatment of bipolar patients with poor response to other mood stabilizers. Gabapentin may improve depressive residual symptoms such as irritability, social withdrawal or anxiety. These results should be confirmed in randomized clinical trials. A recent survey using the US-based TriNetX electronic health records network showed that gabapentin had been prescribed at least once in 13.6% of patients with bipolar disorder (BD), 11.5% with anxiety disorders, and 12.7% with insomnia disorder; for pregabalin, the figures were 2.9%, 2.6%, 3.0% respectively (PJH, unpublished observations). For bipolar disorder, four double-blind RCTs investigating gabapentin, and no double-blind RCTs investigating pregabalin, were identified. A quantitative synthesis could not be performed due to heterogeneity in the study population, design and outcome measures. Background: with increasing awareness of lithium's limitations, several new anticonvulsants had been tested for their mood stabilisation during recent years. Among the innovative third generation mood stabilizing anticonvulsants, gabapentin (GBP) seems to have a broad spectrum of efficacy, although no certain data are available as to its efficacy and use in clinical practice. "In my opinion, gabapentin has been a lifesaver. Conventional drugs for bipolar never have worked well for me. I have bipolar 1, OCD, GAD, PTSD, and a picking disorder. With my bipolar, I have mixed mania and rapid cycling. Since taking gabapentin, my family has noticed a 100% improvement. Introduction Gabapentin has been extensively prescribed off-label for psychiatric indications, with little established evidence of efficacy. Gabapentin and pregabalin, a very similar drug with the same mechanism of action, bind to a subunit of voltage-dependent calcium channels which are implicated in the aetiopathogenesis of bipolar disorder, anxiety and insomnia. This systematic review and Gabapentin and pregabalin have often been prescribed off-label in spite of a paucity of evidence and clinical practice guidelines to support its use. This systematic review aimed to synthesize the available human clinical trials and inform evidence-based pharmacological approaches to BD management. Results: Twenty-two patients (88%) com-pleted the 16 weeks of treatment with gabapentin; 19 (76%) had a positive response as measured by changes in CGI and BPRS scores. The mean dose was 1440 mg/day. The only side effect observed was oversedation, which decreased with continu-ing treatment. Twenty-two RDC bipolar 1 and II patients were assessed by means of the SADS and entered if they gave their consent to participate. All them had suffered from frequent relapses, subsyndromal features (mostly depressive) and incomplete response to other drugs. They all received open-label increasing doses of gabapentin until clinical response. A recent survey using the US-based TriNetX electronic health records network showed that gabapentin had been prescribed at least once in 13.6% of patients with bipolar disorder (BD), 11.5% with
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |