Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
/GettyImages-642110159-5a690e66875db900368b599e.jpg) |  |
 |  |
 | |
 |  |
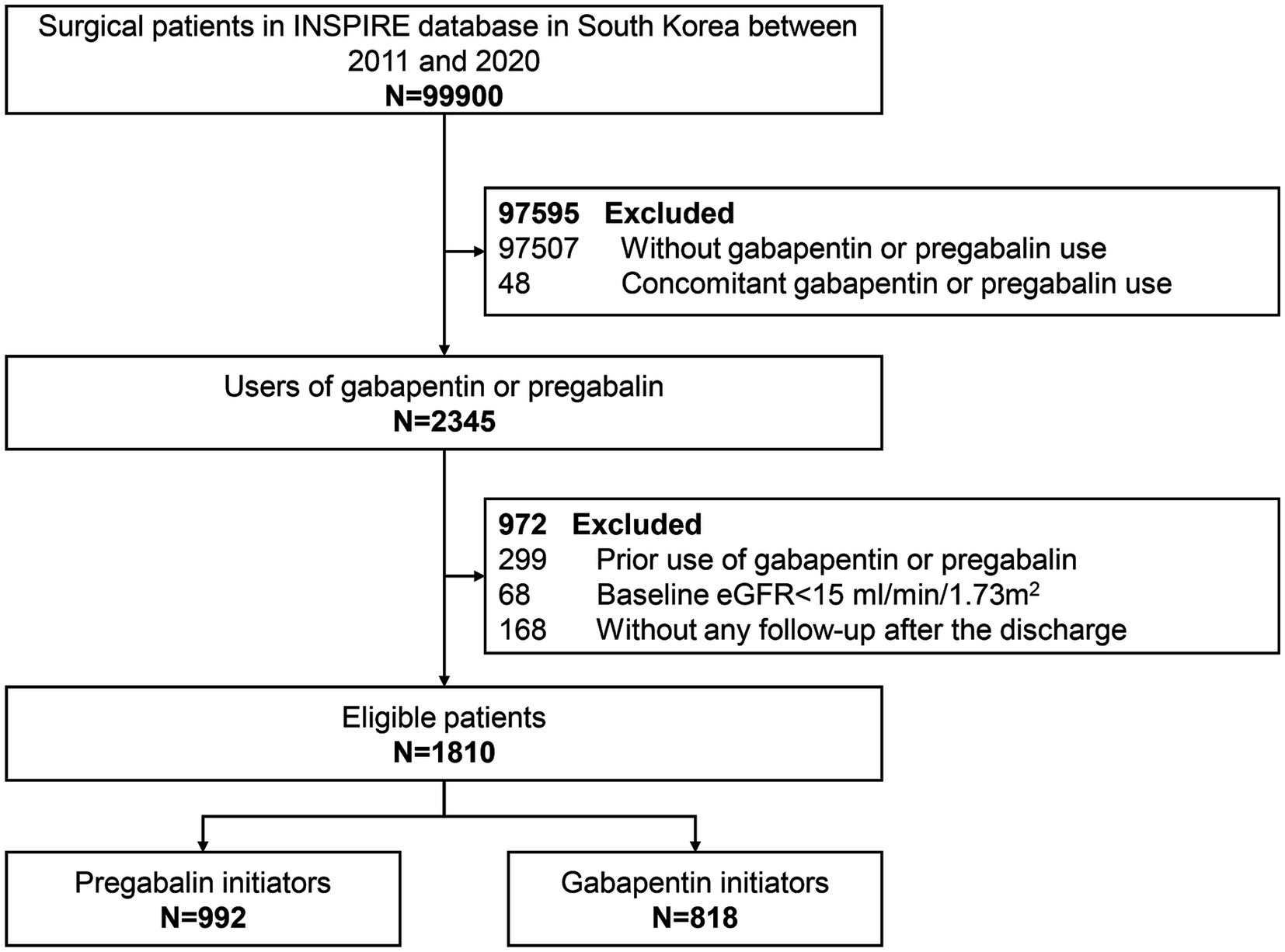 |  |
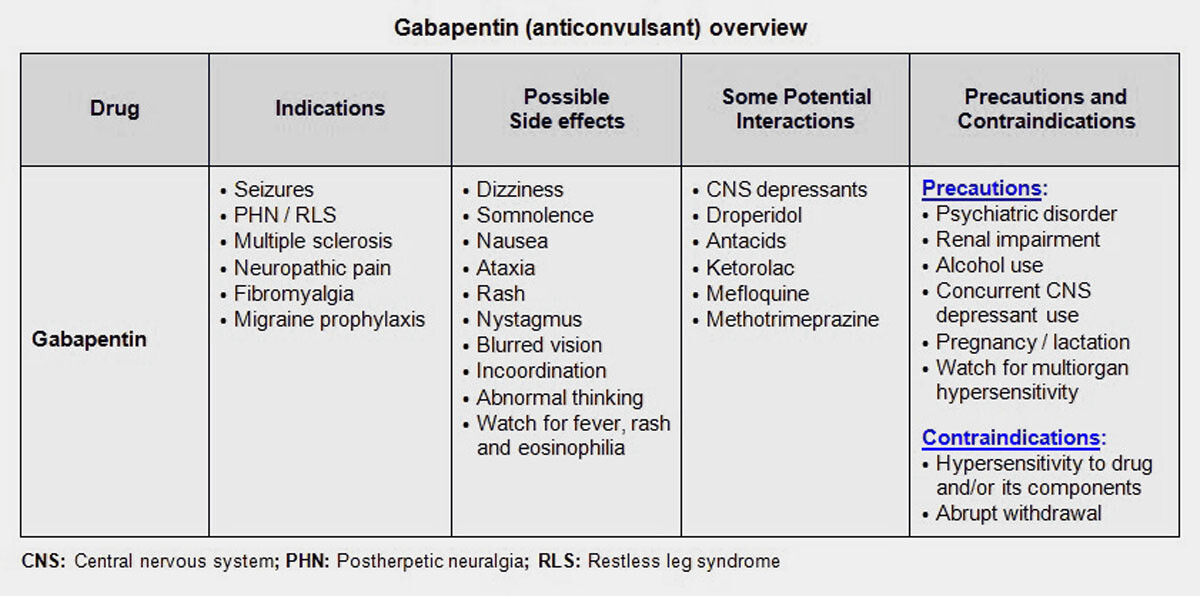
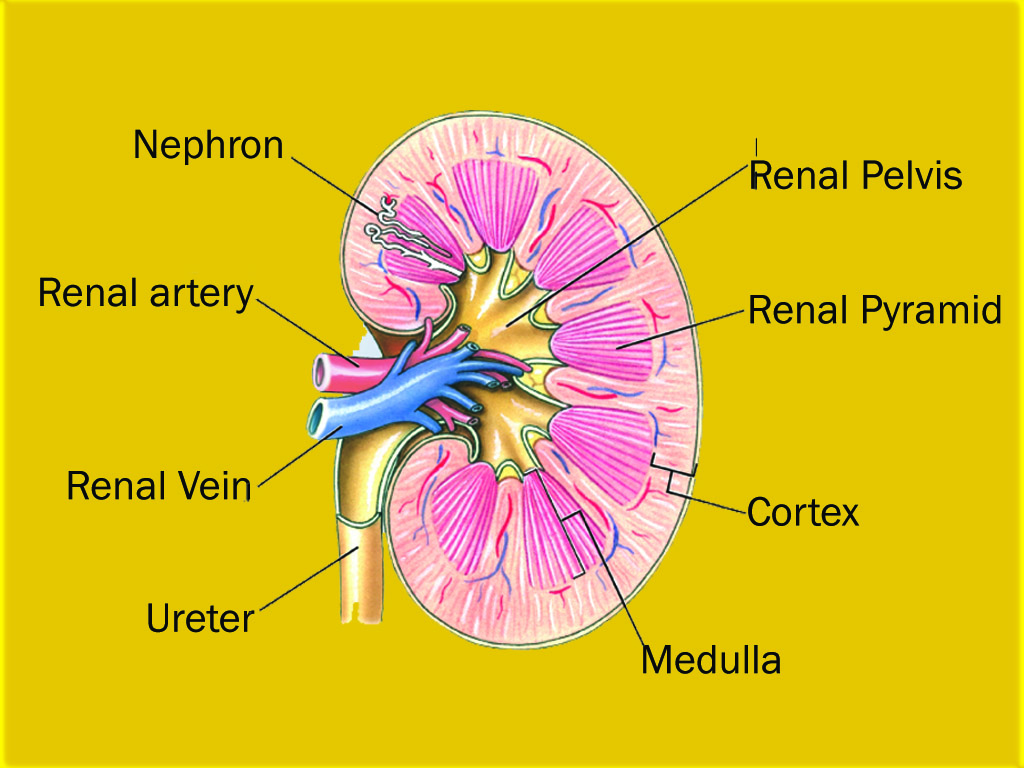
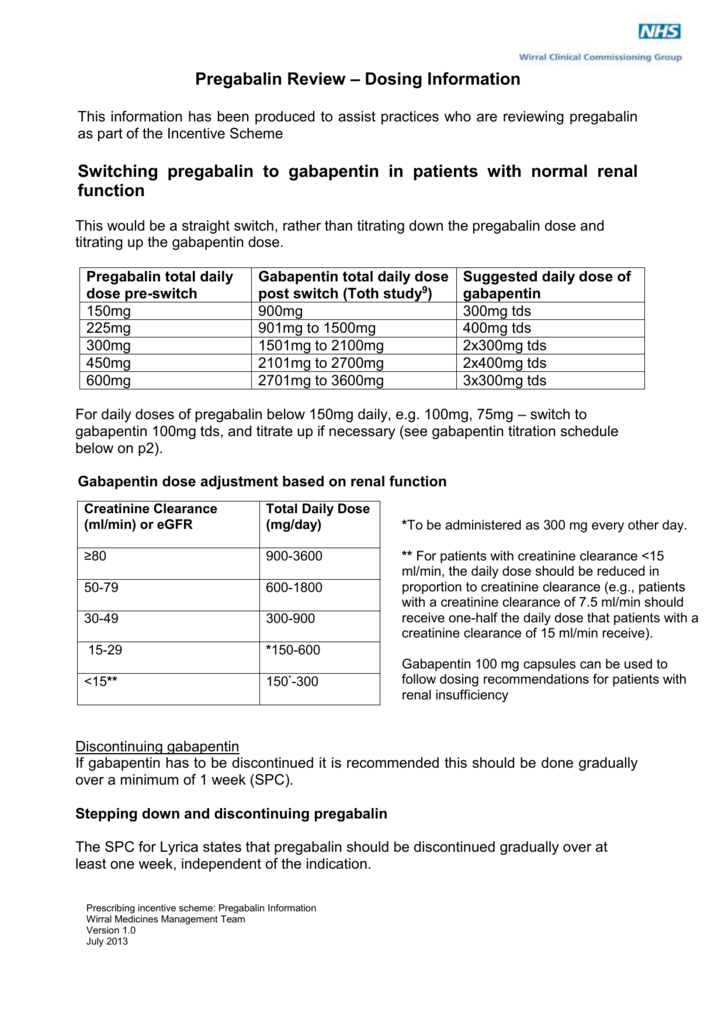
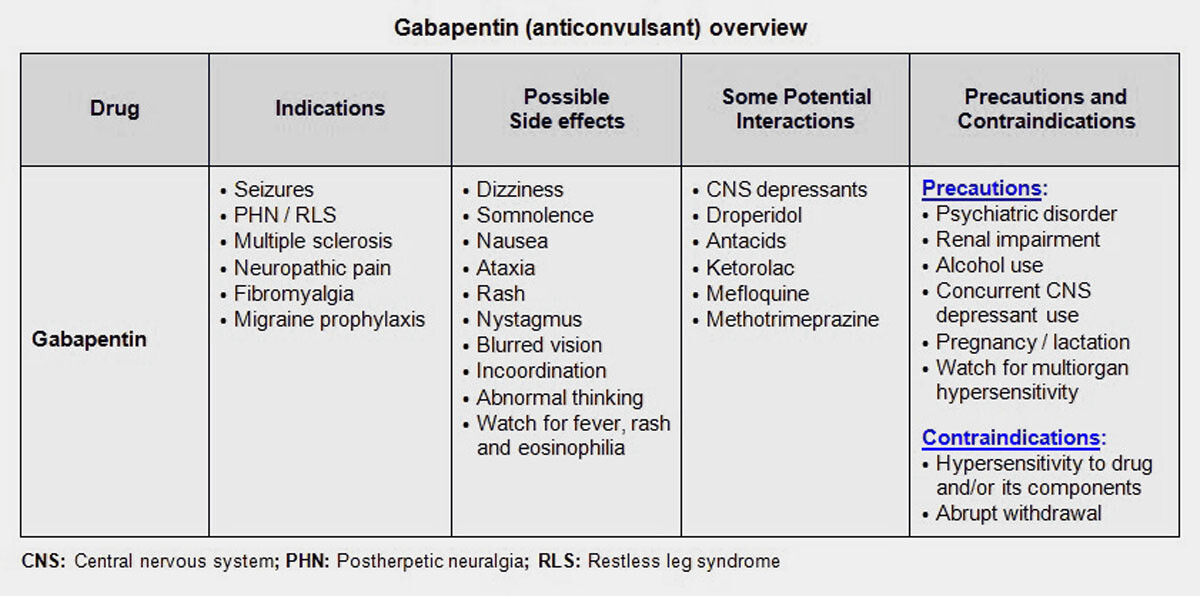
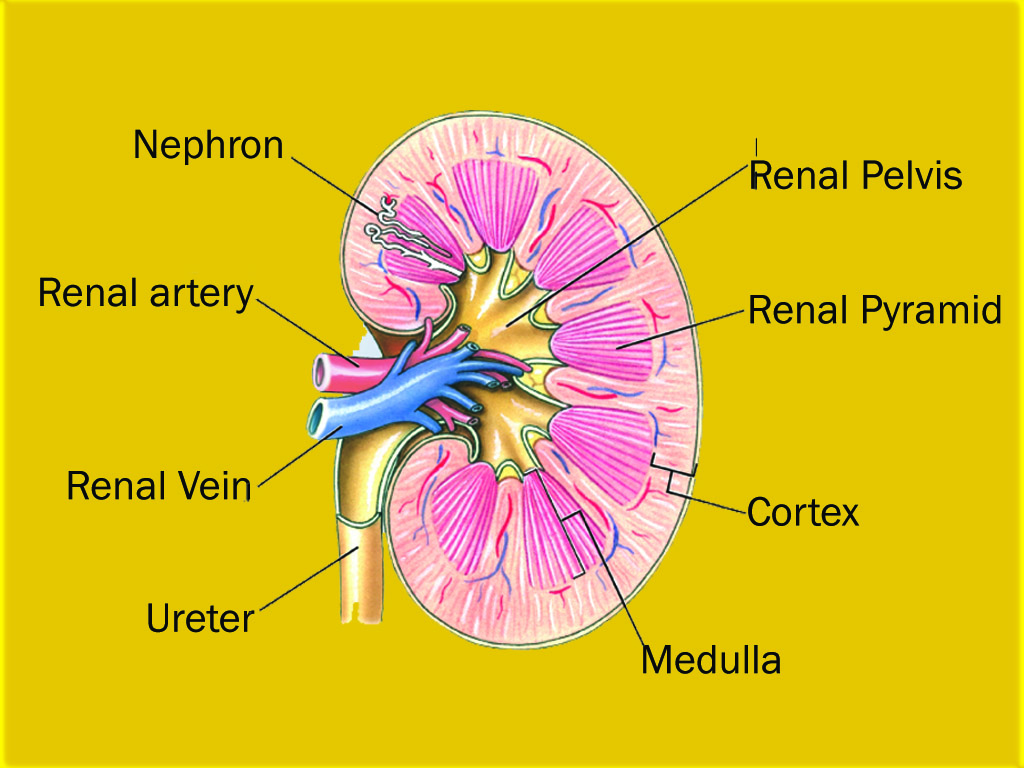
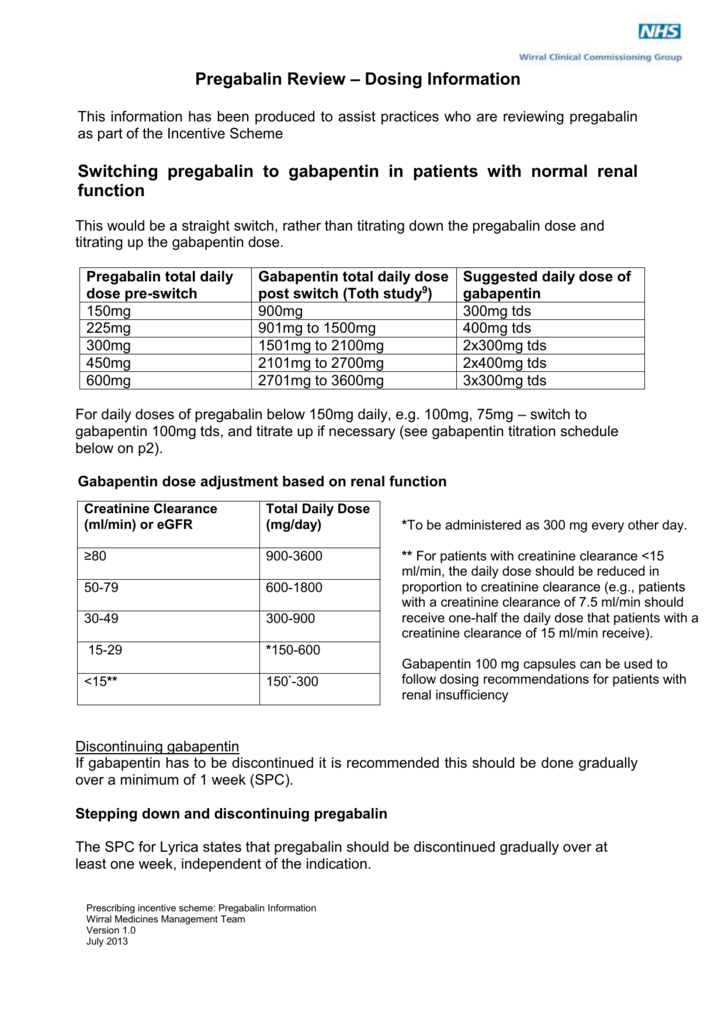
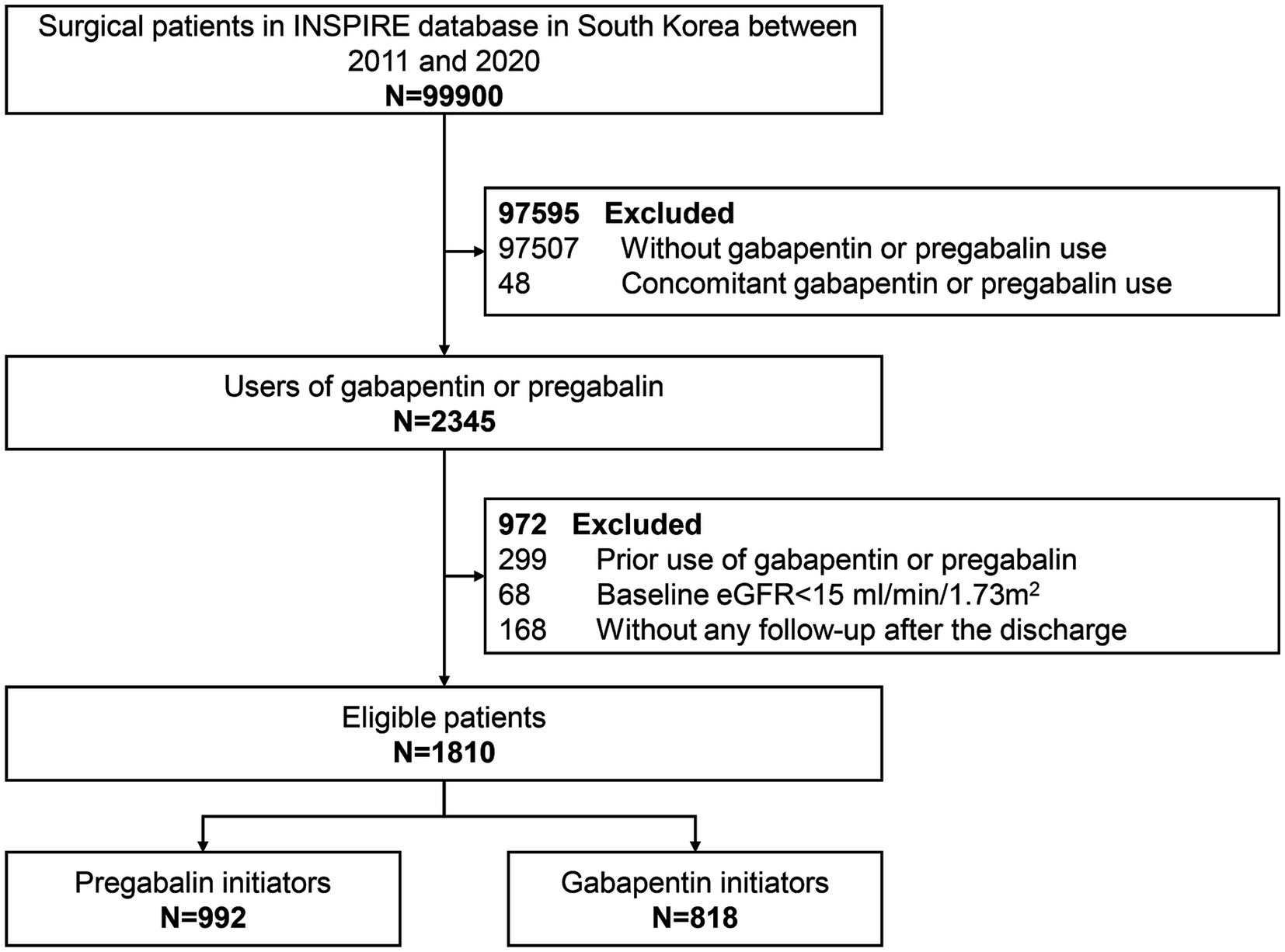
Gabapentin toxicity in patients with chronic kidney disease is underrecognized. Patients with chronic kidney disease often receive inappropriately high gabapentin dosage for their kidney function, occasioning overt toxicity; advanced age and comorbidity predispose these patients for toxicity. I currently take gabapentin for trigeminal neuralgia and have CKD stage 3. Take 900-1200 gabapentin daily over past 20 years. Experiencing severe side effects of gabapentin that Im beginning to think correlate with decreased kidney function. It’s becoming cyclic. Take normal dose of gabapentin until start to become confused and lethargic. Patients with chronic kidney disease often receive inappropriately high gabapentin dosage for their kidney function, occasioning overt toxicity; advanced age and comorbidity predispose these patients for toxicity. Notably, gabapentin is exclusively excreted through the kidneys, making its dose reduction essential when given to patients with impaired renal function. The appropriate dosing based on the patient’s actual creatinine clearance is imperative to prevent severe adverse side effects and drug-related toxicity. Rationale & Objective: Gabapentinoids are opioid substitutes whose elimination by the kid-neys is reduced as kidney function declines. To inform their safe prescribing in older adults with chronic kidney disease (CKD), we examined the 30-day risk of serious adverse events according to the prescribed starting dose. Gabapentin is a prescription drug for seizures and nerve pain. It usually doesn't affect kidney function, but it may cause DRESS syndrome, a rare allergic reaction that can damage the kidneys. Learn more about gabapentin dosing, side effects, and interactions. Gabapentin is widely used in the management of pain. It is entirely excreted through the renal system so this needs to be considered in any patient becoming acutely ill and developing renal failure. We describe a patient who developed significant deterioration in her conscious level due to iatrogenic gabapentin overdose. Gabapentinoids are opioid substitutes whose elimination by the kidneys is reduced as kidney function declines. To inform their safe prescribing in older adults with chronic kidney disease (CKD), we examined the 30-day risk of serious adverse events according to the prescribed starting dose. For patients with chronic kidney dys-function, gabapentin dosage should be adequately adjusted for kidney clear-ance. Gabapentin dosage should be examined on an ongoing basis. Gabapentin toxicity in patients with kidney dysfunction, especially those with advanced age and multiple comor-bidities, should be suspected in appro- Gabapentinoids are opioid substitutes whose elimination by the kidneys is reduced as kidney function declines. To inform their safe prescribing in older adults with chronic kidney disease (CKD), we examined the 30-day risk of serious adverse events according to the prescribed starting dose. Patients with chronic kidney disease often receive dangerously high gabapentin dosage for their kidney function, which can lead to all sorts of problems. An alternative we recommend instead of Gabapentin is Alpha Lipoic Acid. In patients with normal renal function, the maximum dose of gabapentin is 3600mg daily in divided doses. However, gabapentin is renally cleared and so the dose needs to be adjusted according to the GFR. For patients on dialysis, the recommended dose is 100-300mg post dialysis on dialysis days only. the kidney, and pharmacokinetic studies show a stepwise prolongation in the elimination half-life of gabapentin and pregabalin as kidney function declines.9,10 Gabapentinoids should therefore be started at lower doses in patients with chronic kidney disease (CKD; guidelines are summarized in Table S1).1-3,11 Although the risk of gabapentinoid The half-life of gabapentin immediate-release formulation is 5–7 hours in patients with normal renal function and is prolonged up to 52 hours in patients with CrCl<30 mL/min. 26 The half-life of pregabalin is 16.7 hours in patients with CrCl 30–59 mL/min, 25 hours in patients with CrCl 15–29 mL/min, and 48.7 hours in patients with CrCl<15 The standard doses of gabapentin prescribed for people with normal kidney function are not suitable for those with CKD. Typically, healthcare providers will significantly reduce the dose of gabapentin based on a patient’s estimated glomerular filtration rate (eGFR) , a measure of kidney function. Patients with compromised respiratory function, respiratory or neurological disease, renal impairment, concomitant use of central nervous system (CNS) depressants, and elderly people might be at higher risk of experiencing severe respiratory depression and dose adjustments may be necessary in these patients. While gabapentin itself does not directly cause kidney damage, its accumulation due to impaired renal function can lead to increased side effects and potential toxicity. This makes it crucial for healthcare professionals to monitor patients on gabapentin closely, especially if they already have kidney disease. The straightforward answer is yes, you can potentially take gabapentin if you have stage 3 kidney disease, but with significant caveats. It’s crucial to understand that gabapentin is primarily eliminated by the kidneys, meaning that impaired kidney function can lead to a buildup of the drug in your system. In patients with normal renal function, the maximum dose of gabapentin is 3600mg daily in divided doses. However, gabapentin is renally cleared and so the dose needs to be adjusted according to the GFR. For patients on dialysis, the recommended dose is 100-300mg post dialysis on dialysis days only. The clearance of both gabapentin and pregabalin decreases and half-life (t ½) increases proportionately with worsening renal function, requiring renal dose adjustment (Tables 1 and Supplementary Table 1) [106-108]. Both medications should be dosed post-HD.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
/GettyImages-642110159-5a690e66875db900368b599e.jpg) |  |
 |  |
 | |
 |  |
 |  |