Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
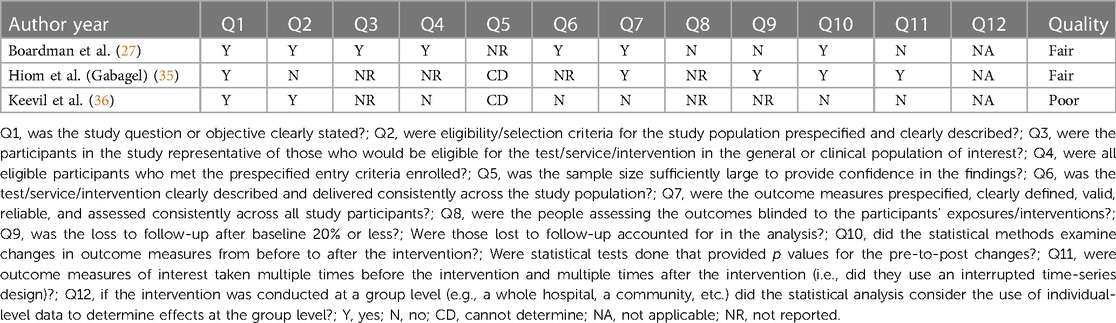
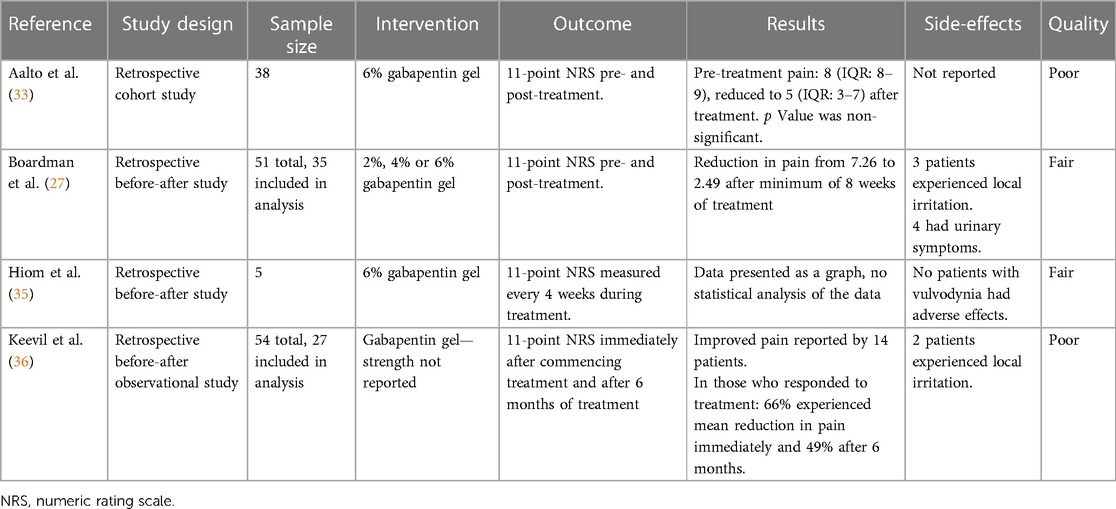
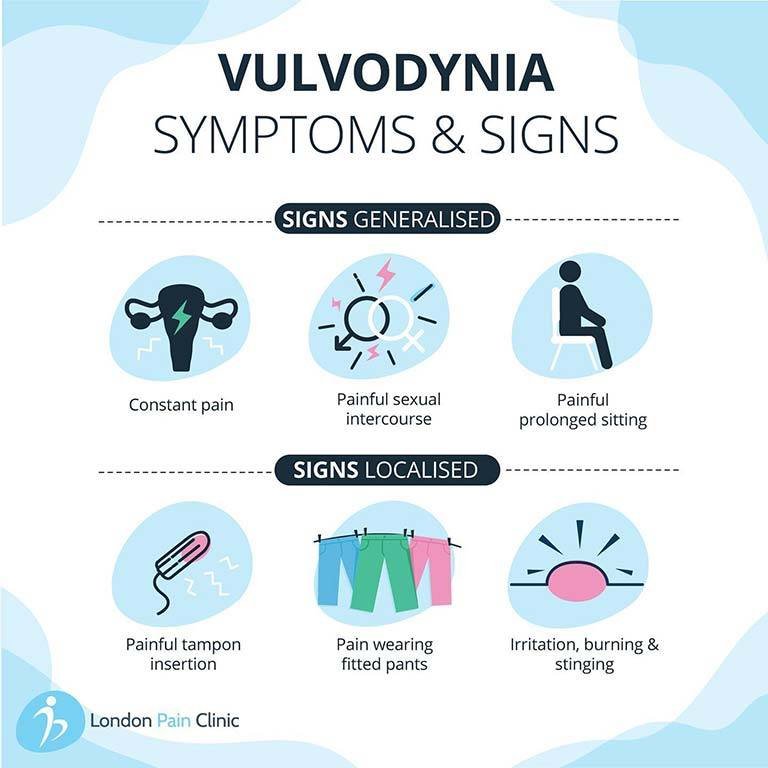
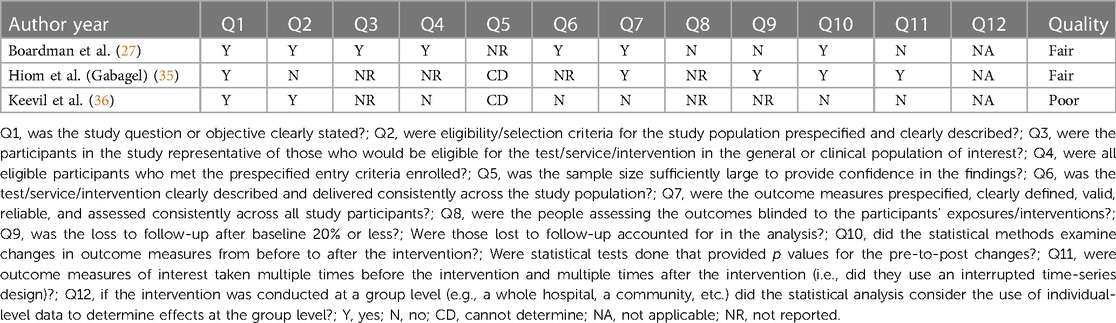
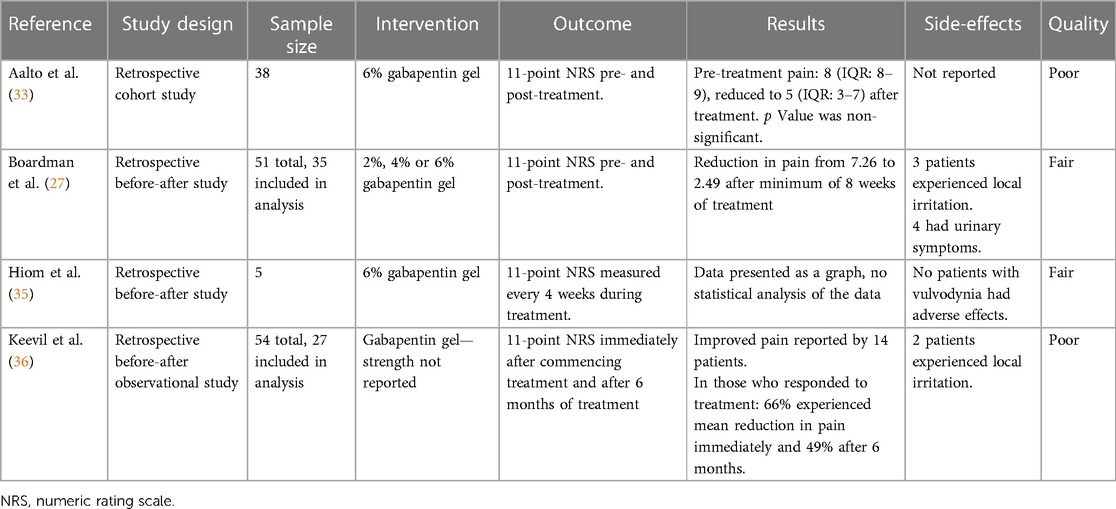
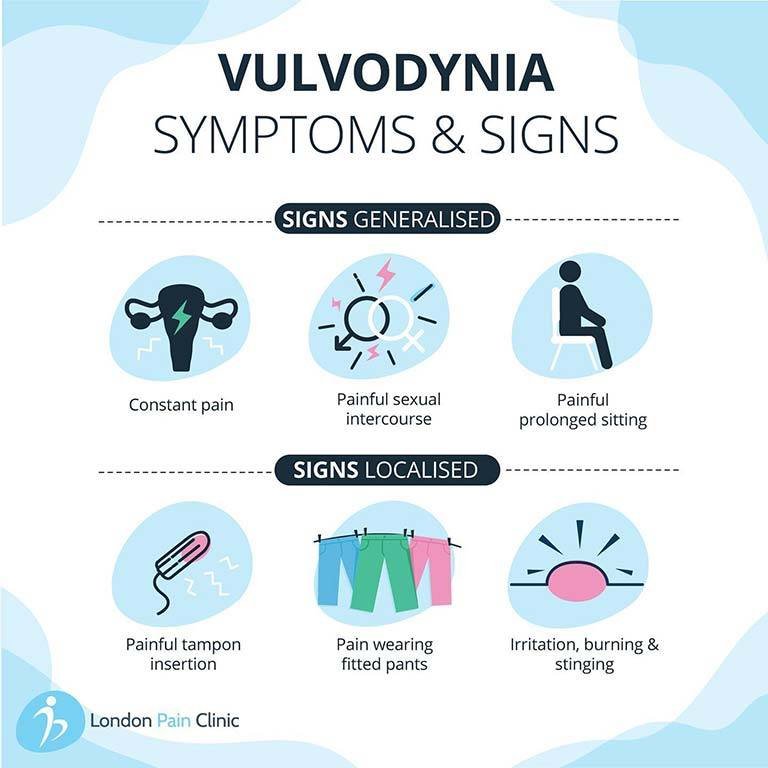
Alongside psychosocial interventions and physiotherapy, pharmacological treatment such as oral gabapentin are used in the treatment of vulvodynia. Topical formulations of gabapentin have shown promise in animal models and case reports investigating its use in other pain conditions. Gabapentin: Highest tolerable oral dose between 1200 and 3000 mg per day for 8 weeks: Oral gabapentin, 1200–3000 mg per day for 8 weeks: Anti-inflammatory agents: Submucosal methylprednisolone (1, 0.5, 0.3 mL) once per week for 3 weeks: Corticosteroids: 0.05% Clobetasol propionate or 0.5% topical hydrocortisone ointment for 28 nights Results: Between January 2001 and December 2006, 51 women with vulvodynia (19 or 37% with generalized vulvodynia, 32 or 63% with localized) were treated with 2% to 6% gabapentin. After a minimum of 8 weeks of therapy, the mean pain score among the 35 evaluable women was significantly reduced from 7.26 to 2.49 (mean change -4.77, 95% confidence We evaluated the efficacy of gabapentin, in an extended release formulation, in women diagnosed with localized provoked vulvodynia, defined as superficial vulvar vestibular pain that is provoked by touch, in a demographically diverse sample. The diagnosis of vulvodynia is clinical A team approach may be necessary to address the different com-ponents of vulvodynia. A lead clinician should triage patients and consider referral to other health professionals who have a role in vulvodynia management, e.g. psychosexual medicine, physiotherapy, pain management teams Although gabapentin is recommended and commonly prescribed for vulvodynia, its value in such cases is usually associated with complaints that have neuropathic components, such as dynamic allodynia. Results from a multicenter US trial do not support a recommendation for use of extended-release gabapentin alone as a treatment for vulvodynia. Between January 2001 and December 2006, 51 women with vulvodynia (19 or 37% with generalized vulvodynia, 32 or 63% with localized) were treated with 2% to 6% gabapentin. After a minimum of 8 weeks of therapy, the mean pain score among the 35 evaluable women was significantly reduced from 7.26 to 2.49 (mean change -4.77, 95% confidence interval Antiepileptics treat vulvodynia by calming the central nervous system and are used to treat neuropathic pain conditions. 89, 90 In a multicenter double‐blind crossover RCT, oral gabapentin did not reduce dyspareunia. 90 There is no evidence to support the use of oral gabapentin for vulvodynia. Future of Vulvodynia Treatments Gabapentin has been employed in vulvodynia therapy for its properties in treating neuropathic pain. Gabapentin inhibits voltage-gated calcium influx in neurons thereby preventing release of the nociceptive neurotransmitter glutamate. 38 Two nonrandomized studies and 1 case report investigated the use of topical gabapentin ( Table 6 ). Tricyclic antidepressants should be considered for the treatment of vulvodynia. Selective serotonin reuptake inhibitors and gabapentin (Neurontin) should be considered for symptomatic relief The purpose of this study was (1) to evaluate whether extended-release gabapentin is more effective than placebo in improving sexual function in women with provoked vulvodynia and whether there is a relationship between treatment outcome and pelvic pain muscle severity that is evaluated by palpation with standardized applied pressure and (2) to evaluate whether sexual function in women with Gabapentin, used to manage neuropathic pain disorders, is the most studied and used anticonvulsant for vulvodynia 4. Dosage can be increased over time from 300 mg total daily to a maximum dose of 3,600 mg daily (1,200 mg by mouth three times a day), and may need adjustment to avoid adverse effects. Gabapentin and botulinum toxin A are both safe and effective treatments for vulvodynia that lead to significant reductions in pain. The improvements in patient outcomes that we found suggest that vulvodynia has physiological, and possibly neuropathic, bases. Gabapentin improved sexual function in this group of women with provoked vulvodynia, although overall sexual function remained lower than women without the disorder. The highly significant increase in the arousal domain of the FSFI suggests a central mechanism of response. Objective: To evaluate whether extended-release gabapentin is more effective than placebo among women with vulvodynia. Methods: In a multicenter double-blind, placebo-controlled randomized crossover trial, gabapentin (1,200-3,000 mg/d) was compared with a placebo. to benefit vulvodynia include topical corticoste roids, topical testosterone, and topical antifungal medications. Table 1. Topical Medications Used to Treat Vulvodynia Topical medication Dosage Side effectsa 5% lidocaine ointment Apply to skin as needed; dispense 30-g tube. Do not use .20-g of ointment in a 24-h period. Erythema or edema. Rare Gabapentin (Neurontin) and Lyrica have been used to treat chronic pain conditions, including vulvodynia Gabapentin tends to have fewer side effects than the tricyclic antidepressants. Physical therapy of the pelvic floor muscles is commonly employed in the treatment of vulvodynia, for both local and generalized pain. Since oral gabapentin is frequently used for neuropathic pain, Boardman et al 23 hypothesized that topical gabapentin could be effective in treating vulvodynia. Records were gathered of pre- and postmenopausal women diagnosed with localized or generalized vulvodynia over a 6-year period and were narrowed to those treated with topical gabapentin. For treating vulvodynia, gabapentin works by inhibiting pain signals that are sent from damaged neurons. The retrospective study that was published in Obstetrics and Gynecology showed that gabapentin cream was well tolerated and effective for women experiencing vulvodynia. About 80% of the women using the cream showed at least a 50% improvement Gabapentin appears to be very effective in the treatment of generalized vulvodynia, unprovoked. It has a very low side effect profile. Certain patients may be less likely to benefit from gabapentin, including those with the comorbidity of sleep disturbance.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |