Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
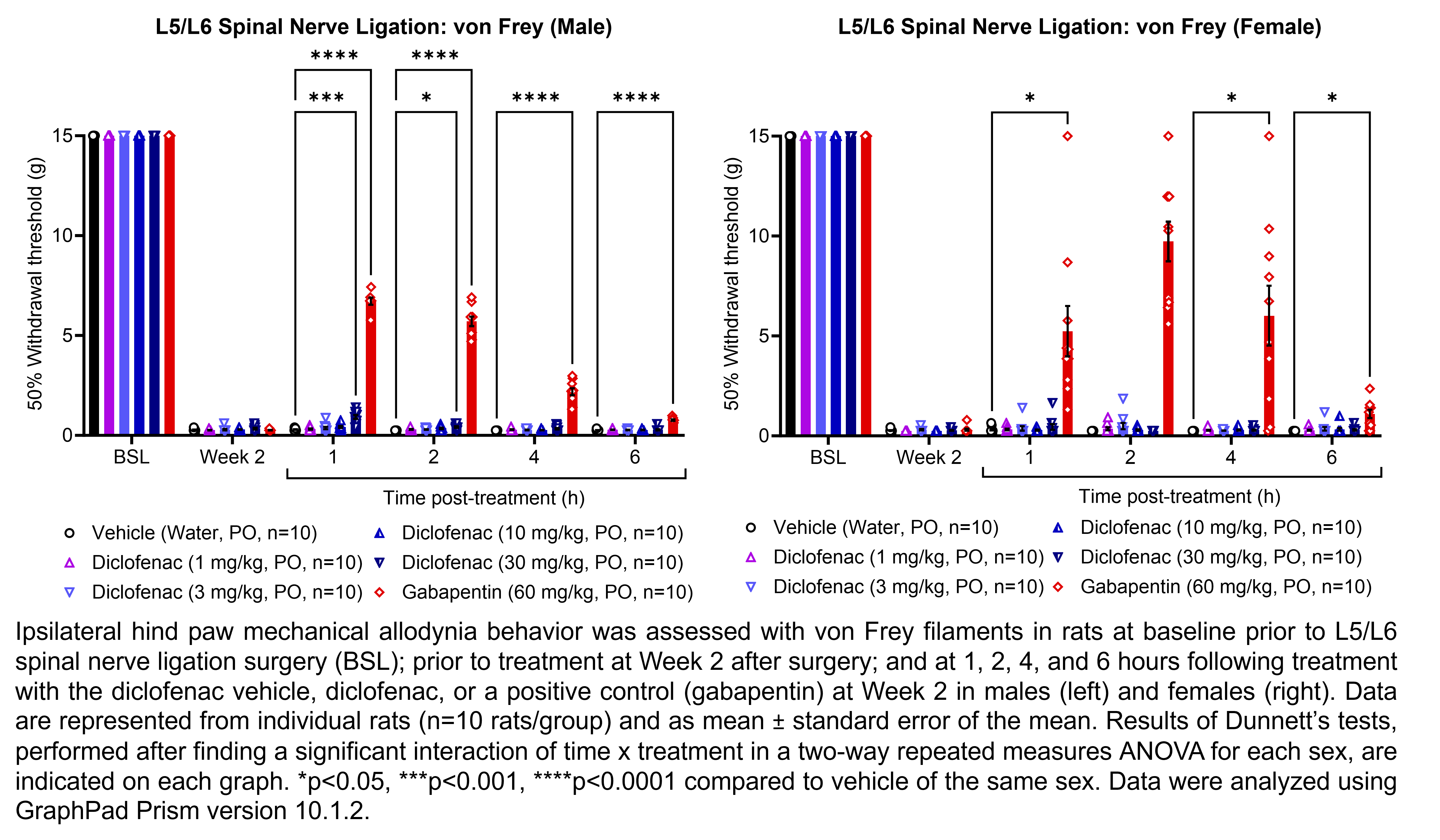
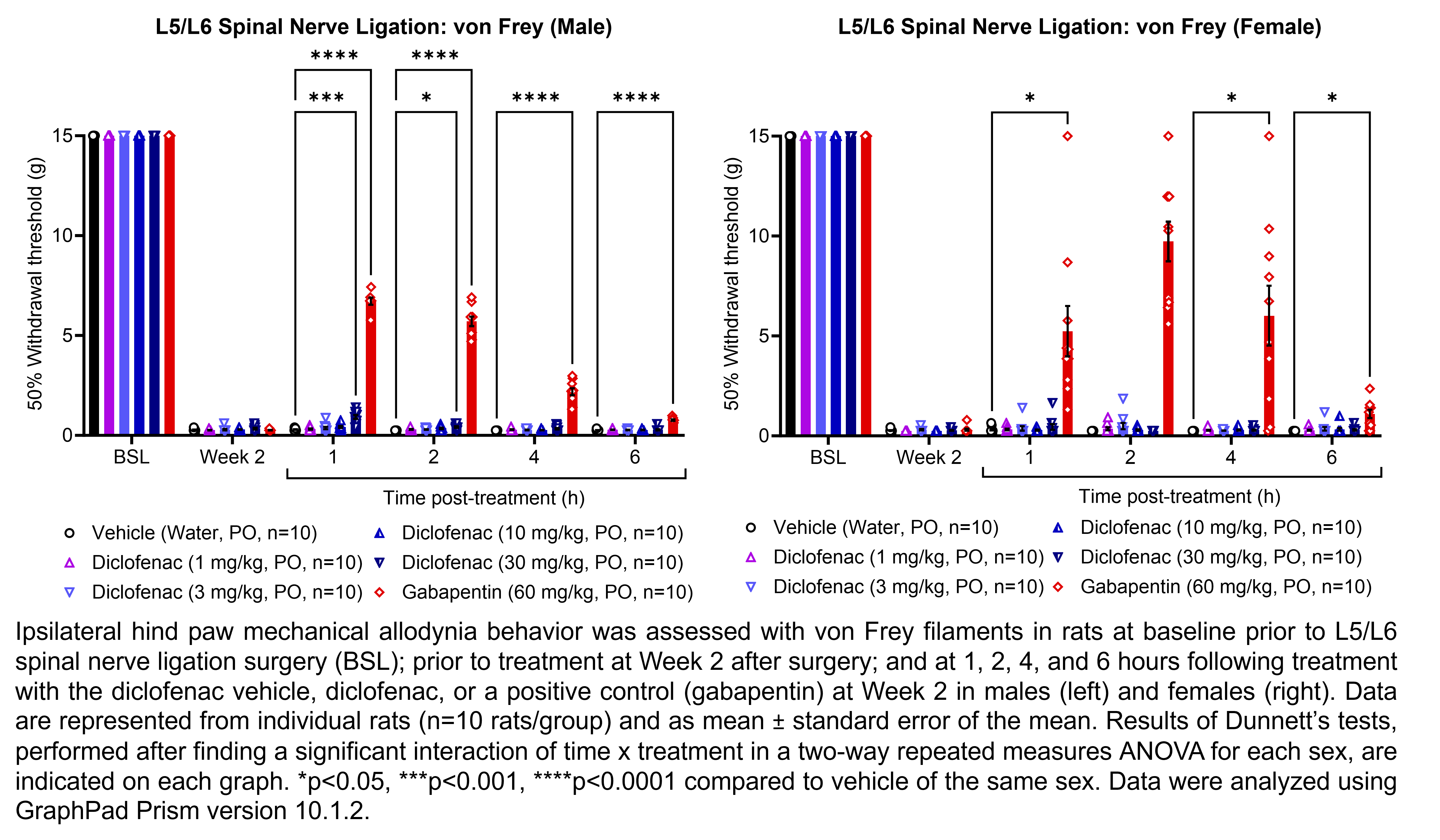
To identify patients eligible to newly receive gabapentin for perioperative pain management, we excluded those who received gabapentin before surgery, had other indications or contraindications for gabapentin, or received critical care, mechanical ventilation, or a feeding tube in the immediate perioperative period. In this cohort study, perioperative gabapentin use was associated with increased risk of delirium, new antipsychotic use, and pneumonia among older patients after major surgery. These results suggest careful risk-benefit assessment before prescribing gabapentin for perioperative pain management. Gabapentin (1200 mg) administered orally 2 h before surgery decreased the intraoperative fentanyl and isoflurane consumption, postoperative analgesic requirements, postoperative pain, and the incidence of postoperative nausea and vomiting, but increased dizziness. 1. Introduction. The findings contradict guidelines published by the American Pain Society (APS) in 2016, which advocate “around the clock” use of gabapentin, pregabalin and other nonopioid drugs both before and after surgery. Conclusion: Gabapentin 600 mg administered 1 hr before laparoscopic abdominal surgery is as effective as gabapentin 900 mg for PONV control and VAS reduction of 24-hour postoperative pain scores with fewer side effects. On the other hand, gabapentin 300 mg did not demonstrate good control of PONV, or pain control compared to higher doses. 1. 2. A typical dose range for perioperative gabapentin is 200-300 mg and 25-50 mg for pregabalin. 3. Given the opioid-sparing effect of gabapentinoids, lower doses of perioperative narcotics may be used. 4. While the benefits of perioperative gabapentinoids are well-documented, their use may First, we repeated the analysis by defining gabapentin exposure on the day of surgery without requiring a 2-day minimum length of stay after surgery. Then, we explored a dose-response relationship using a 4-dose category of gabapentin (no use, 1 mg to <600 mg, 600 mg to <1200 mg, or ≥1200 mg). Similarly, aside from 24 h after surgery, gabapentin significantly reduced pain with movement (25–27,31,34,35,37,38) by 18% to 28% (VAS 8.2 mm to 10.2 mm) after surgery . The pooled effects on VAS pain scores displayed significant heterogeneity, which was not explained by subgroup analyses based on surgical procedure, gabapentin dose or study day trial, patients in the gabapentin group showed improved VAS pain scores and improved Leeds Assessment of Neuropathic Symptoms and Signs (LANSS) scores compared to patients in the naproxen group. In 2006, Sihoe et al. evaluated gabapentin in the treatment of chronic pain after chest surgery (6). This was a heterogeneous group of patients. Turan et al. investigated the effects of gabapentin on acute postoperative pain and on morphine consumption in patients undergoing spinal surgery where 1,200 mg gabapentin was given 1 hour before surgery. The Cleveland Clinic study had patients take a preemptive dose of three drugs: acetaminophen, the nerve pain medication gabapentin and the NSAID celecoxib (Celebrex). “Giving non-opioid pain medications before may help prevent the cascade of pain-causing chemicals that comes from your central nervous system after surgery,” explains Memtsoudis. Purpose of review: This review summarizes the risks and benefits of gabapentinoids (gabapentin and pregabalin) for perioperative pain control and the controversies surrounding their use in a variety of settings. We review current literature with the goal of providing patient-centric and procedure-specific recommendations for the use of these According to this review, pre-operative 1200 mg or less gabapentin as a single dose was associated with lesser post-operative pain and opioid demand during first 24 h after surgery, but multiple dosage of gabapentin before and after surgery did not cause a reduction in VAS score for pain, in this regard it suggests single pre-operative dose of Postoperative opioid consumption was reduced when using gabapentin within the initial 24 hours following surgery (standard mean difference −1.35, 95% confidence interval [CI]: −1.96 to −0.73; P <0.001). There was a significant reduction in morphine, fentanyl, and tramadol consumption (P <0.05). undergoing elective or emergent surgery under any type of anesthesia were considered. Included trials had to evaluate gabapentinoids (pregabalin or gabapentin) initiated between 1 week before and 12h after surgery. At least one outcome measure had to be assessed to be considered for inclusion. In the absence of either criteria, discontinue prior to surgery. Irreversible MAO antagonists may require 2 weeks after discontinuation of drug for normal MAO function to return. Therefore these medications should be tapered and discontinued two weeks before elective surgery. We defined new postoperative gabapentin as fills for 7 days before surgery until 7 days after discharge. We excluded patients whose discharge disposition was hospice or death. The primary outcome was prolonged use of gabapentin, defined as a fill>90 days after discharge. However, perioperative gabapentin had a significant effect on promoting opioid cessation after surgery. MeaningSeventy-two hours of perioperative gabapentin use may promote opioid cessation after surgery and decrease the duration of postoperative opioid use. Gabapentin (n= 208) 1200 mg before surgery and 1800 mg for 72 hours after: Patients treated with gabapentin had a 24% increase in the rate of opioid cessation after surgery (p=0.05). However, there were no significant differences in the number of adverse events. Gordh et al., 2008 26 Sweden: Randomized controlled trial: 98 patients MEDICATIONS TO STOP PRIOR TO YOUR SURGERY . You will need to temporarily stop taking the following medications before your surgery. These medications can thin your blood, change its clotting, and slow the healing process after surgery. Be aware: Many over-the-counter products may have some of these ingredients and must also be stopped.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |