Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
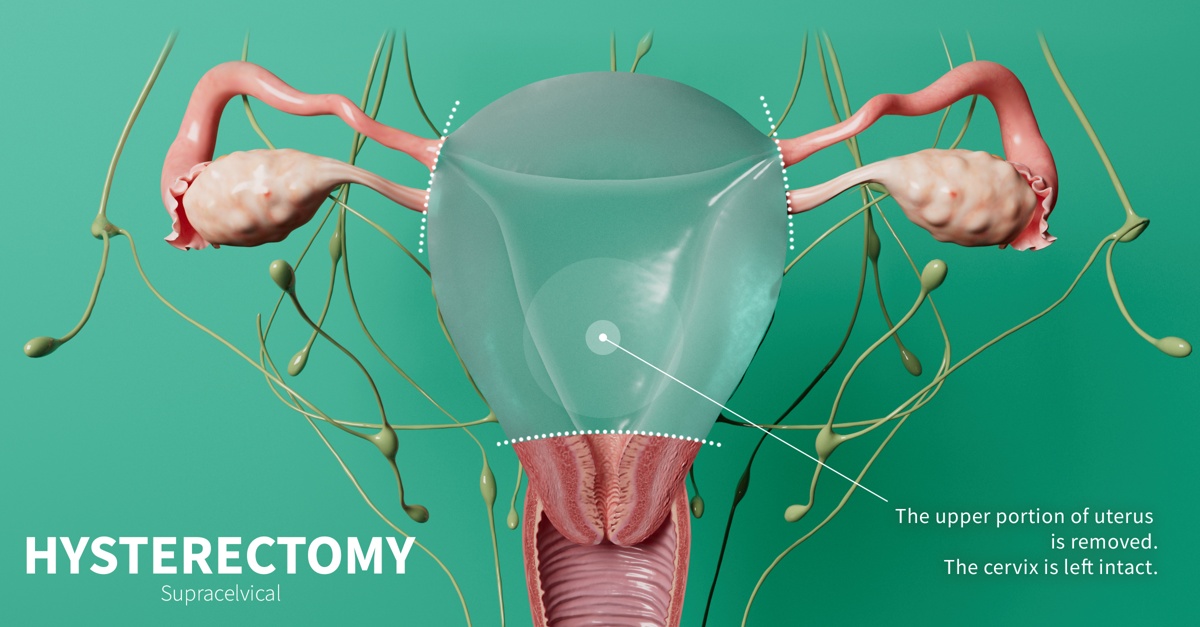
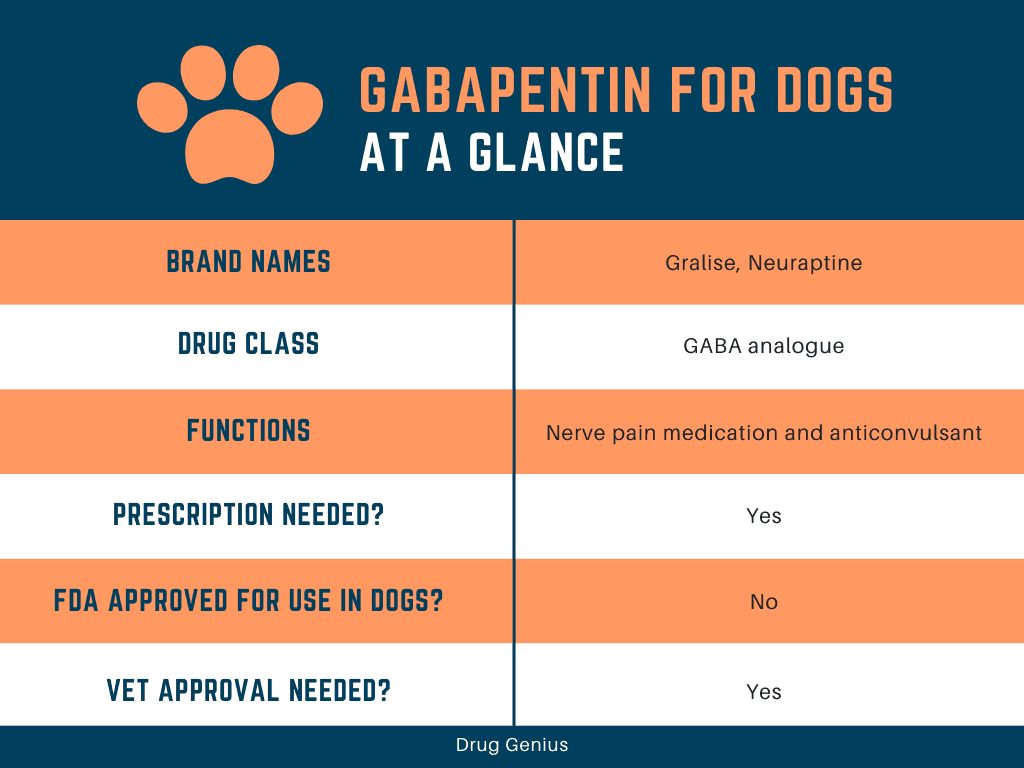
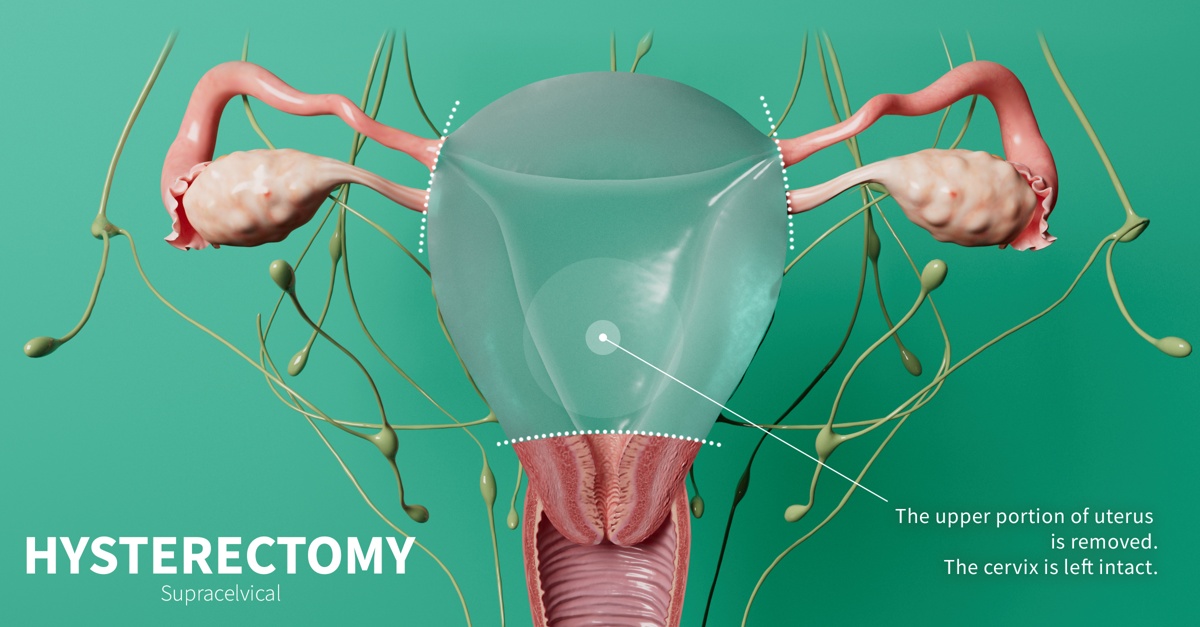
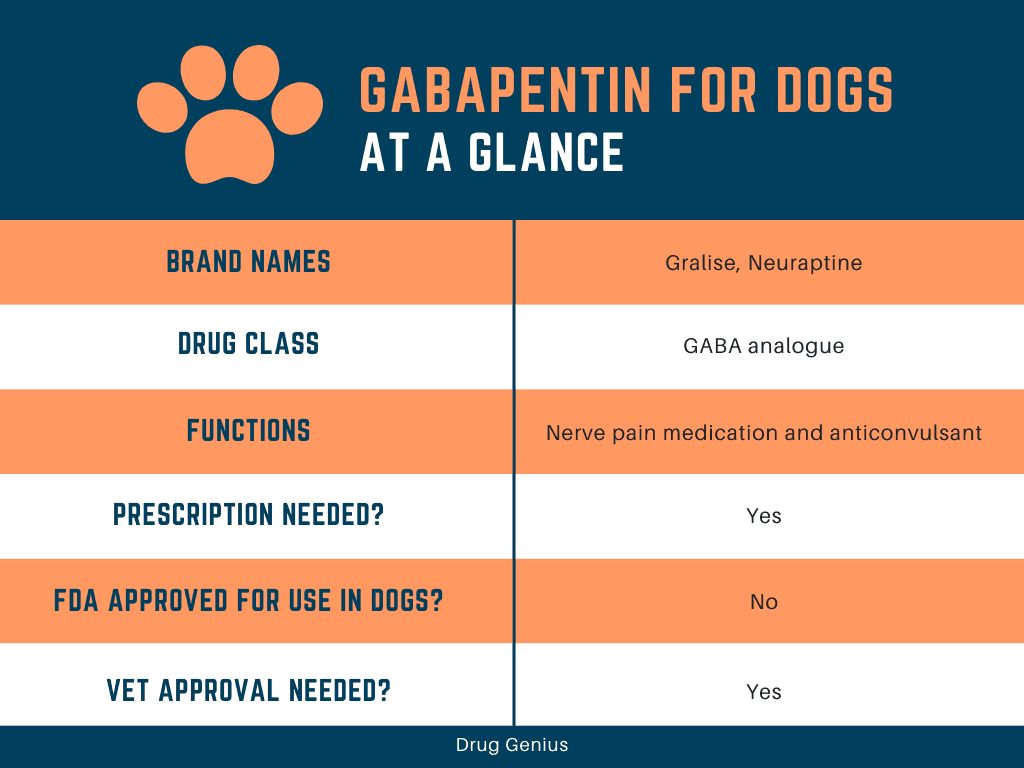
Gabapentin was associated with increased dizziness, but it significantly reduced the use of antiemetic at any time in thefirst 24 postoperative hours. Patient satisfaction in the two groups was good and not found to differ. Conclusion: Preemptive administration of gabapentin before laparoscopic hysterectomy does not decrease postoperative pain To evaluate whether a single dose of gabapentin given preoperatively reduces narcotic use 24 hours after minimally invasive hysterectomy (MIH). tic drug. Several randomized studies have evaluated the effectiveness of preemptive gabapentin before surgical incision for hysterectomy as well as combined use of preemptive and postoperative gabapentin. This meta-analysis and systematic review examined the evidence for preemptive use of gabapentin in abdominal hysterectomy. A search for articles published between 2004 and 2013 was conducted Conclusion: Gabapentin 600 mg administered 1 hr before laparoscopic abdominal surgery is as effective as gabapentin 900 mg for PONV control and VAS reduction of 24-hour postoperative pain scores with fewer side effects. On the other hand, gabapentin 300 mg did not demonstrate good control of PONV, or pain control compared to higher doses. In a triple-blind trial, the study investigators randomly assigned women undergoing laparoscopic hysterectomy to receive 600 mg gabapentin (n = 43) or placebo (n = 45) orally 1 hour before the procedure. Patient-controlled opioid analgesia was provided postoperatively. The authors, accordingly, suggested using a single dose of gabapentin before hysterectomy, in order to reduce postoperative pain. Dierking et al. studied the effect of 1200 mg gabapentin 1 hour before the surgery, in respect to placebo, in hysterectomy patients, showing considerable decrease in pain, nausea and vomiting in the gabapentin group Gabapentin, an anticonvulsant, has recently been suggested as an effective postoperative ‘analgesic’ agent. The objective of the present study was to examine the analgesic effectiveness, opioid-sparing effects and side effects associated with the use of gabapentin in a perioperative setting. Objective: This study sought to examine the efficacy of preemptive use of gabapentin in laparoscopic hysterectomy for benign gynaecologic conditions. Methods: In a triple-blind trial, the study investigators randomly assigned women undergoing laparoscopic hysterectomy to receive 600 mg gabapentin (n = 43) or placebo (n = 45) orally 1 hour before the procedure. Preemptive medication strategies (eg, medications given to the patient before surgery), including paracetamol and acetaminophen, gabapentin, nonsteroidal antiinflammatory drugs, and COX-2 inhibitors, have been shown to decrease total narcotic requirements and improve postoperative pain and satisfaction scores in women undergoing total abdominal In all the trials, gabapentin was administered preoperatively as a single oral dose or two divided doses 2–24 hours before surgery at a dose ranging from 300 mg to 1,200 mg. This study also identified an association between cumulative gabapentin dose and reduction in morphine consumption. Metaregression analysis showed that the effect of gabapentin in reducing morphine consumption (compared with placebo) at 24 hours was stronger in the preoperative only group than in the preoperative and postoperative groups. hysterectomy were reduced more with gabapentin alone (pre-operative dosing) than when gabapentin was given both pre-operatively and postoperatively. The benefits of gabapentin for minimally invasive hysterectomy (MIH) are not as well defined. The randomization code was kept by the hospital's pharmacy and revealed to the investigators only after completion of all statistical analysis. To the best of our knowledge, this was the first randomized trial evaluating the effects of preemptive gabapentin before hysterectomy by laparoscopy. Dierking et al found no difference in pain after hysterectomy between patients treated with 3000 mg gabapentin and placebo, although they showed that gabapentin decreased morphine consumption by 32%. These results are likely due to either differences in the time of morphine administration, or the fact that each patient in the test group was On the other hand, the study by Dierking et al. showed that a total dose of 3000 mg gabapentin before and within 24 hours of surgery had no significant effect on postoperative pain score, but reduced postoperative morphine consumption after hysterectomy surgery . In our study, postoperative opioid consumption was lower in the group receiving Thirty patients were excluded for different reasons; and 140 included patients were randomly assigned to one of two groups according to the method of treatment, gabapentin or placebo, in a double-blind manner before hysterectomy. Postoperatively, the pain was assessed on a visual analogue scale (VAS) at 1, 4, 8, 12 and 24 h at rest. The patients in the gabapentin group received gabapentin 600 mg every 6 hours, starting from 18 hours before surgery, until the 5th postoperative day. The pain score and morphine request rate were assessed for 2‒3 days and 1 month after the surgery. Prior to instructing the patient on preoperative medication management, completion of a thorough medication history is recommended – including all information on prescription medications, over-the-counter medications, “as needed” medications, vitamins, supplements, and herbal medications. Allergies should also be verified and documented. We investigated, in a randomized, placebo-controlled, double-blind study, the efficacy and safety of gabapentin on pain after abdominal hysterectomy and on tramadol consumption in patients. The 50 patients were randomized to receive either oral placebo or gabapentin 1200 mg 1 h before surgery. Metaregression analysis showed that the effect of gabapentin in reducing morphine consumption (compared with placebo) at 24 hours was stronger in the preoperative only group than in the preoperative and postoperative groups.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |