Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
/human-internal-digestive-organ-liver-anatomy-1269115008-d736a0e2fa9b4266a2c01506e15352e3.jpg) | /GettyImages-1080011718-b7f22fa56b934a6b96c23e17458086c9.jpg) |
 |  |
 | |
 |  |
 |  |
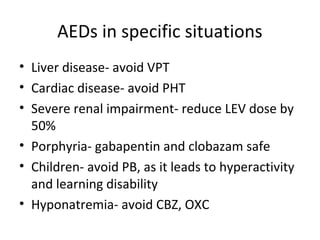
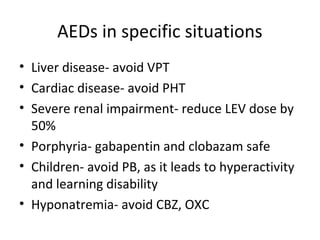
Herein, we report a gabapentin-induced hepatocellular injury in a patient without another identifiable cause for acute liver injury. Discontinuing gabapentin resulted in rapid reversal improvement in hepatocellular injury. Keywords: gabapentin, hepatotoxicity, drug-induced liver injury. Carbamazepine has been reported to cause hepatotoxicity in the general population; it may precipitate a rapid deterioration in cirrhotic patients and thus should be avoided. 46 Gabapentin is unique among many anticonvulsants because it is not metabolized by the liver or bound to plasma proteins, making it a preferred anticonvulsant in patients Adjuvant analgesics such as tricyclic antidepressants and anti-convulsants may be used cautiously for cirrhotic patients with neuropathic pain. Gabapentin or pregabalin may be better tolerated in cirrhosis because of non-hepatic metabolism and a lack of anti-cholinergic side effects. The physicians found that a statistically significant 15.8% of patients on Acamprosate advanced to severe liver disease, including scarring, cirrhosis, alcohol hepatitis or liver cancer, compared with 13.4% of the veterans taking gabapentin. Antiepileptics such as gabapentin and pregabalin are sometimes used to treat neuropathic pain. The LiverTox, an authoritative resource for drug-induced liver injury, classifies these 2 agents as class C, indicating that clinically apparent liver injury is uncommon. 55, 56 Mechanistically, both agents are likely safe to use in hepatic impairment, as they are primarily renally eliminated in an What does gabapentin have to do with any of that? The itching is from the cirrhosis What you need for that is an antihistamine. Herein, we report a gabapentin-induced hepatocellular injury in a patient without another identifiable cause for acute liver injury. Discontinuing gabapentin resulted in rapid reversal improvement in hepatocellular injury. Keywords: drug-induced liver injury; gabapentin; hepatotoxicity. Gabapentin/pregabalin: not metabolized by the liver or bound by proteins, but consider renal dysfunction in cirrhosis patients, as well as other relevant side effects (e.g. sedation, dizziness); minimal data on safety of these agents. A large cohort study of patients with alcohol use disorder found that patients with cirrhosis who were prescribed gabapentin for AUD were less likely to experience cirrhosis decompensation. Figure 9: The percent of patients with no drinking days (or maintained abstinence) who received gabapentin vs placebo for the treatment of alcohol use disorder. INTRODUCTION. Chronic pain in cirrhosis is common, poorly characterized, and uniquely morbid. Reported by 40%–79% of patients with cirrhosis, 1,2 it is a key driver of poor functional status and quality of life. 3–6 Patients with cirrhosis and chronic pain also have significantly greater health care use. 7 Pain management in cirrhosis can be complex because of challenges in diagnosis and We would like to show you a description here but the site won’t allow us. In an effort to facilitate safe pain control, this article will summarize the existing literature regarding impaired pharmacokinetics due to liver dysfunction and dosing recommendations for analgesic treatment in patients with cirrhosis. Other more long-term issues can result from liver failure, scarring or cirrhosis, and liver cancer. Sometimes, even other conditions outside the liver itself like heart failure can lead to liver congestion and enzyme changes. Rare individual case reports of liver injury from gabapentin have been published, although the causal relationship of gabapentin with the liver injury was not always clear. The latency to onset in these reports was 1 to 8 weeks and associated with cholestatic pattern of enzyme elevations. Carbamazepine is associated with hepatotoxicity and should be avoided in patients with liver dysfunction. Gabapentin is the preferred agent, as it is not metabolized hepatically nor protein bound, but should be adjusted according to renal function. 4. Summary and Recommendations Gabapentin and pregabalin are safe; use cautiously in patients with hepatic encephalopathy. Topical lidocaine and diclofenac are safe. Pain is common and affects 30%-79% 1 of patients with cirrhosis. Cirrhosis is severe liver damage, and while there are few treatments for the condition, some pain medications can help. gabapentin for neuropathic pain, starting at 300 milligrams (mg) daily While there are no cures for the late-stage liver disease there are various treatment options including gabapentin and cirrhosis of the liver. One of the main goals of cirrhosis treatment is to ease the symptoms. Some options include avoiding alcohol, a low-salt diet, and weight loss. Pain is prevalent in patients with cirrhosis. Due to potential alterations in drug metabolism, risk for adverse effects, and complications from cirrhosis, physicians are often faced with difficult choices when choosing appropriate analgesics in these patients. Overall, acetaminophen remains the preferred analgesic. Despite its potential for intrinsic liver toxicity, acetaminophen is safe when Pain management in patients with cirrhosis is a difficult clinical challenge for health care professionals, and few prospective studies have offered an evidence-based approach. In patients with end-stage liver disease, adverse events from analgesics are frequent, potentially fatal, and often avoidable. Severe complications from analgesia in these patients include hepatic encephalopathy
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
/human-internal-digestive-organ-liver-anatomy-1269115008-d736a0e2fa9b4266a2c01506e15352e3.jpg) | /GettyImages-1080011718-b7f22fa56b934a6b96c23e17458086c9.jpg) |
 |  |
 | |
 |  |
 |  |