Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 | |
 |  |
 |  |
 |  |
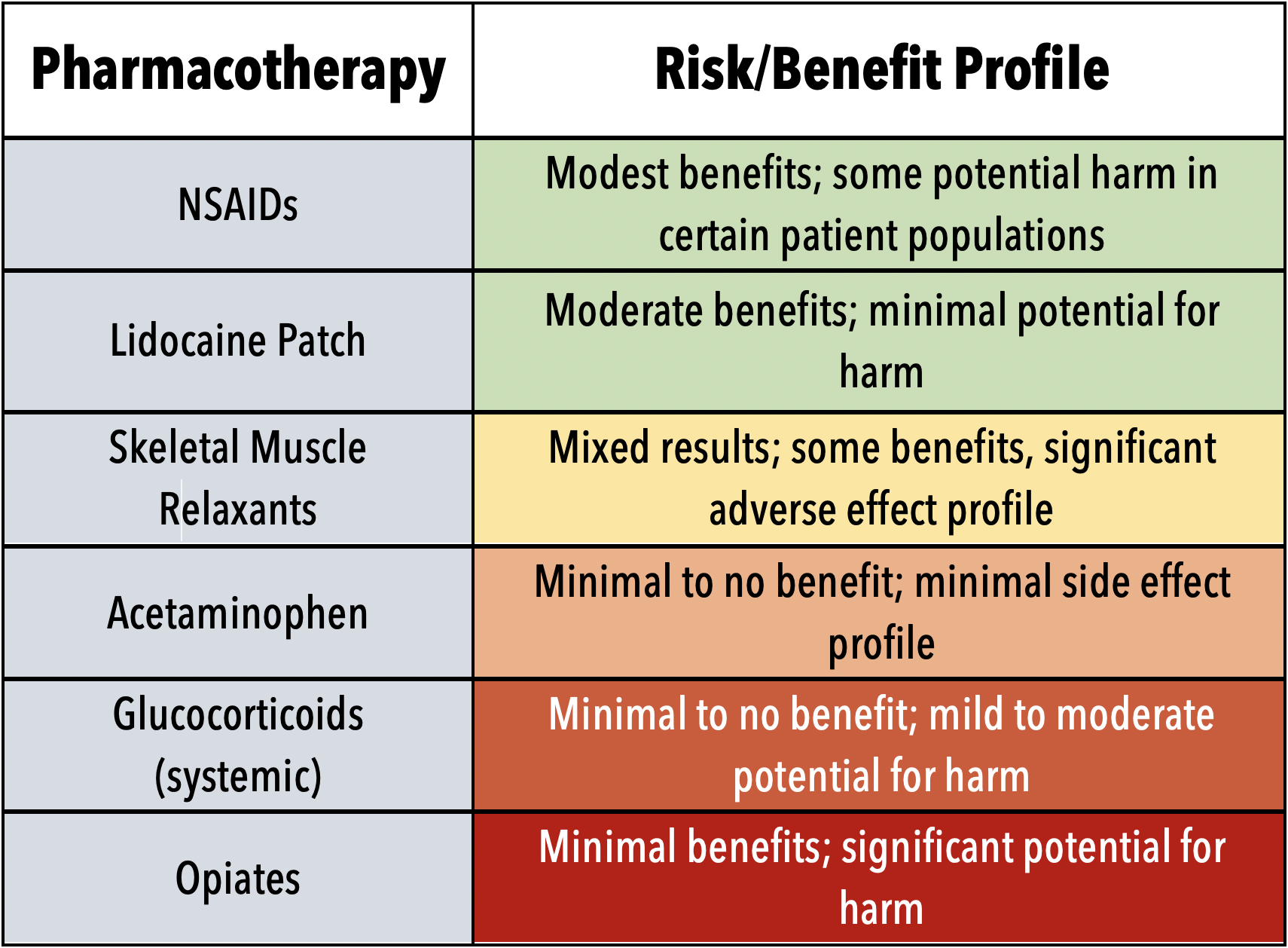
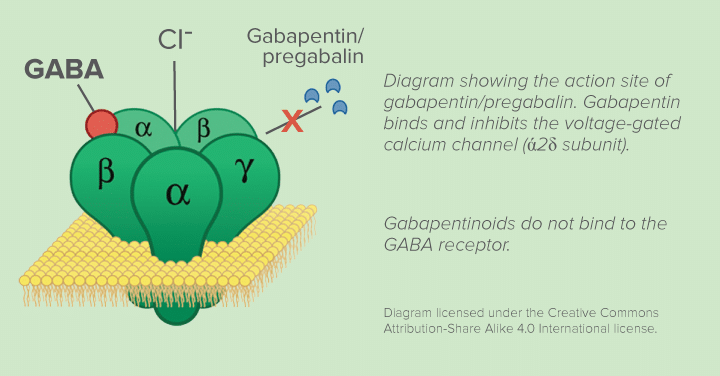
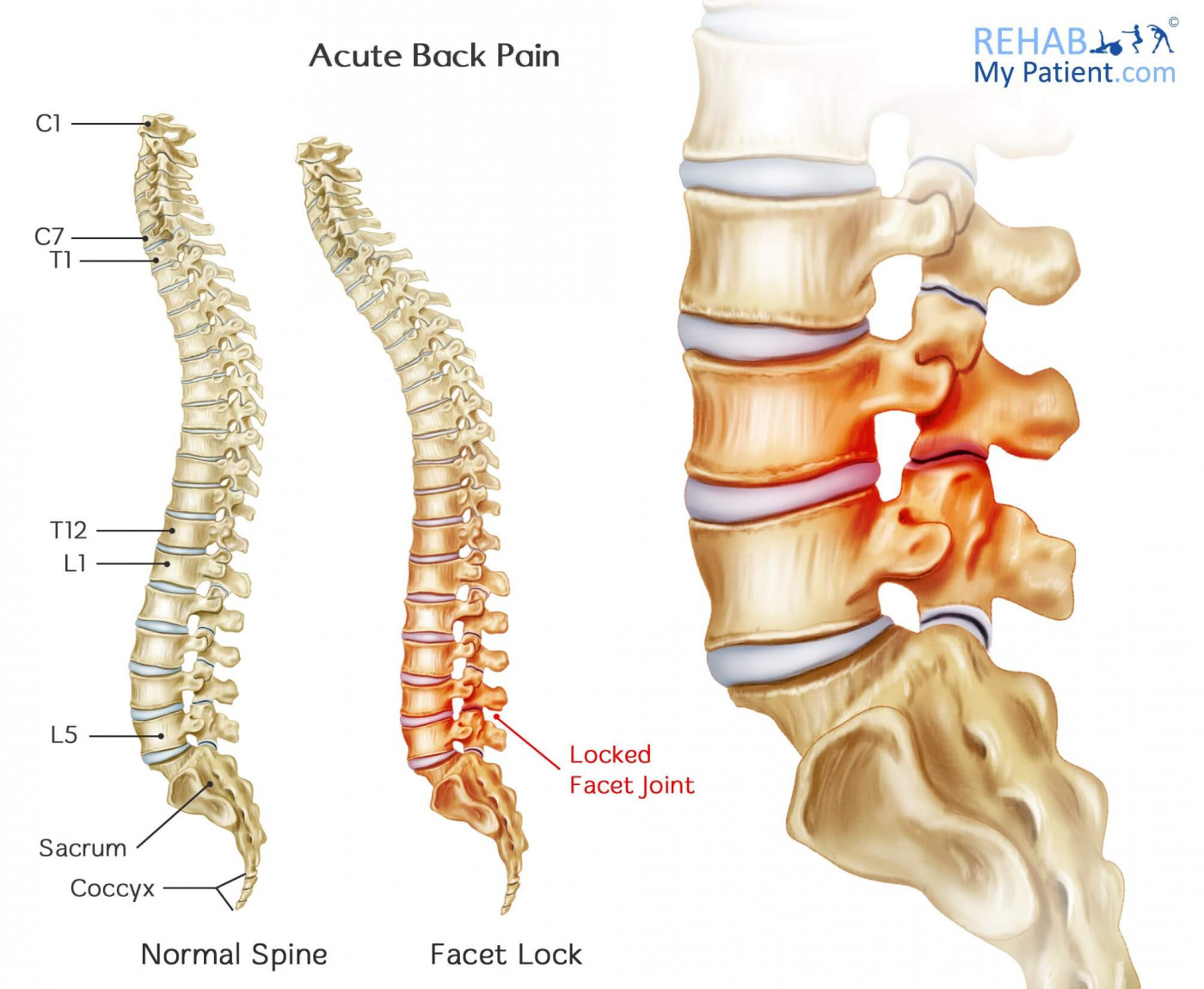
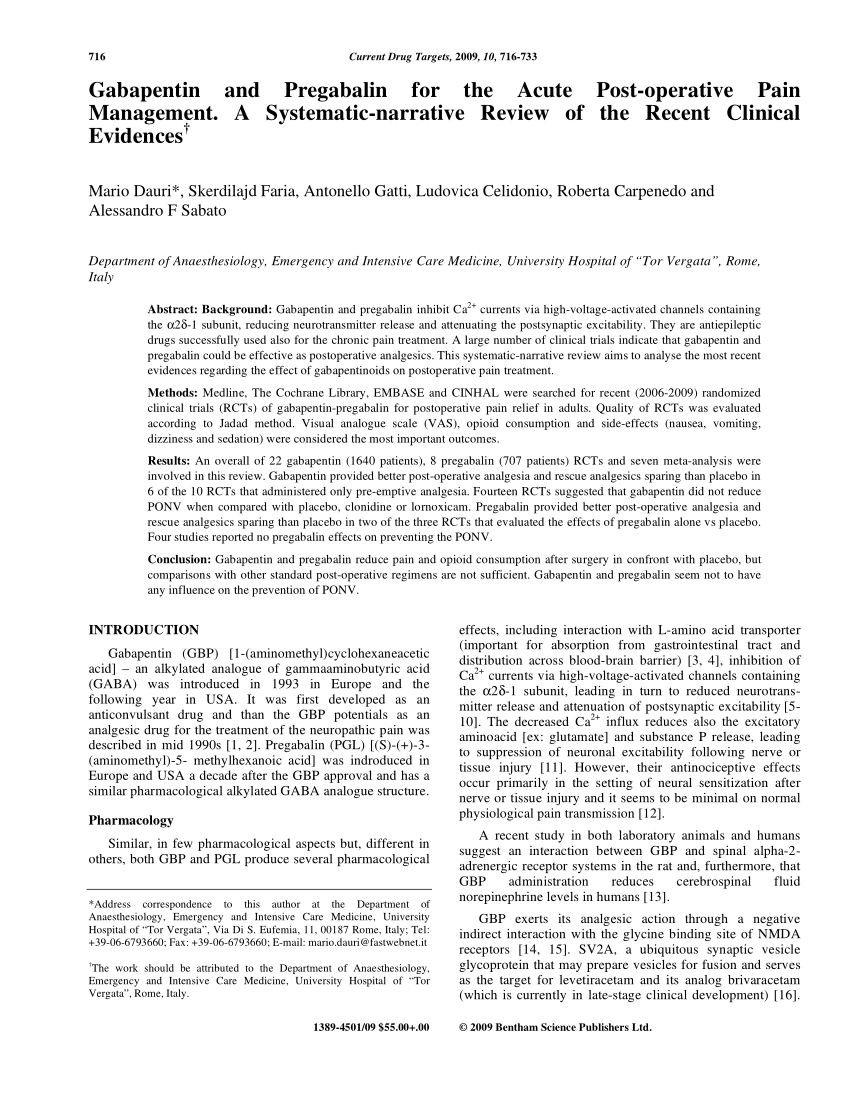
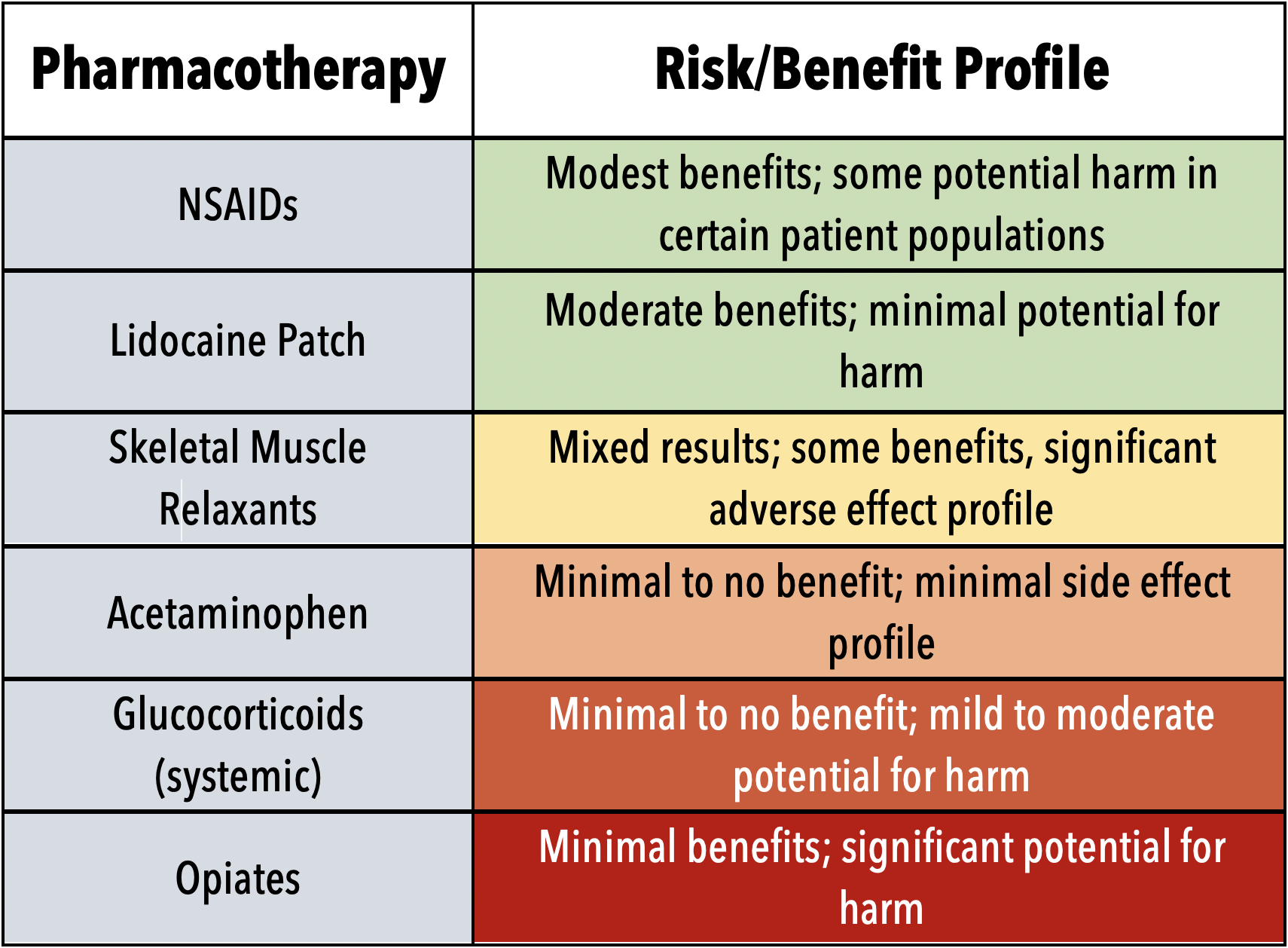
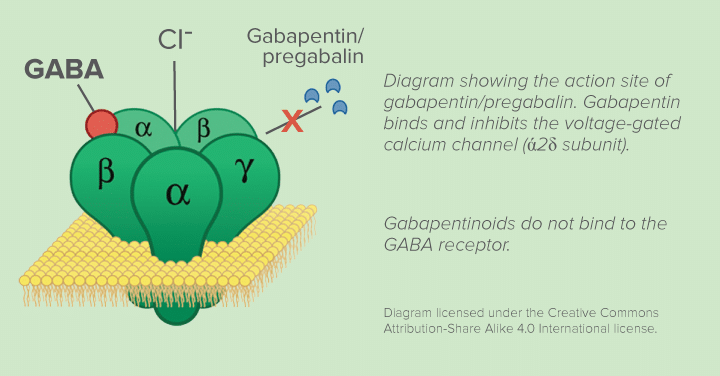
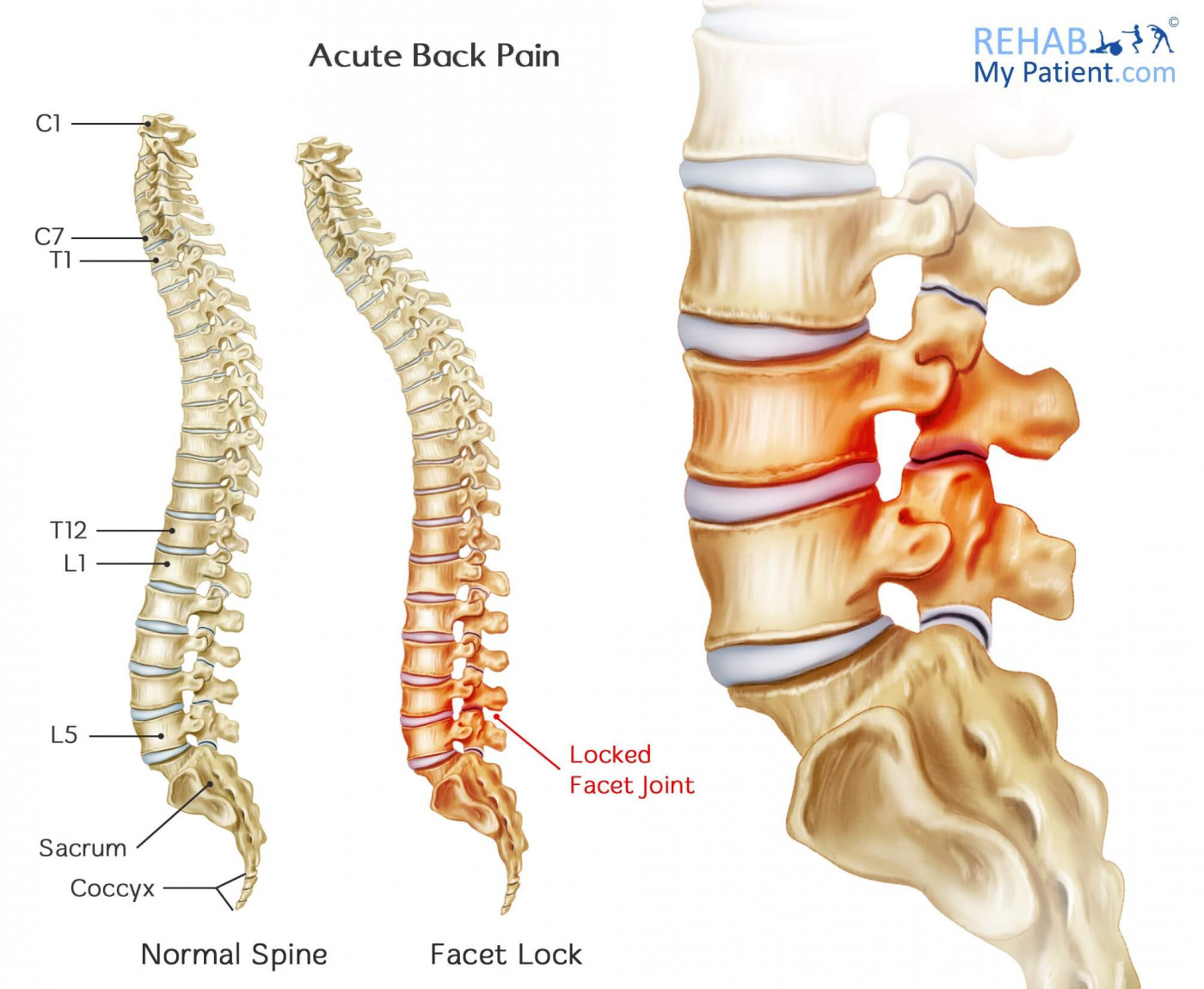
Gabapentin for treatment of radicular low back pain. American Family Physician. Mathieson, S., et al. (2017). Trial of Pregabalin for Acute and Chronic Sciatica. The New England Journal of Medicine. Medicine Optimisation. (2020). Back pain & sciatica – NICE warn against benzos, gabapentinoids & opioids. MedlinePlus. (2020). Capsaicin topical Acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs) are first-line treatment options for most patients with acute mild to moderate pain. Topical NSAIDs are recommended for non–low If your back pain is nerve-related, then the anticonvulsant drug gabapentin may be a good choice for you. This article will explain how gabapentin works, detail its uses, and go over potential side effects, so that you can assess with your doctor whether this drug may be right for you. Gabapentin is a remedy for nerve pain that’s also prescribed for back pain. See how it works and if it can help back pain from sciatica, shingles, and more. Gabapentin reduces neuropathic pain by < 1 point on a 0-10 point scale and benefits about 15% of carefully selected patients (NNT=6-8). A similar proportion of people suffer harm (NNH=8). A test of benefit/harm can be made after 1-2 days at a low dose (100-900 mg/day). Benefit is unlikely to increase with higher doses or longer treatment. A 2016 double-blind RCT (N = 108) investigated gabapentin as a treatment for chronic low back pain with and without a radicular component. 2 This RCT was included in the 2017 meta-analysis but is An oral NSAID (see Non-steroidal anti-inflammatory drugs) should be considered for managing acute low back pain, taking into consideration the risks associated with NSAIDs, the need for continued monitoring, and the possible need for gastroprotective treatment (for further information, see Peptic ulcer disease). If you’re seeking relief from back pain, understanding how gabapentin works in managing nerve pain is crucial. Gabapentin, an anti-seizure medication, is often prescribed for neuropathic pain, including nerve pain radiating from the back. The purpose of this review is to critically appraise the evidence for the use of gabapentinoids for acute pain management and its impact on the development of chronic pain after surgery. Recent findings: Recent meta-analyses have revealed that prior data likely have overestimated the beneficial effects of gabapentinoids in acute perioperative Gabapentin (Neurontin™) has gained significant interest as part of a multi-modal pain management strategy for the control of acute pain. There has been considerable variation in both the dose and the regimen used in recent clinical trials. Most have relied on pre-operative dosing and have utilized a single dose of 300 to 1200 mg. Higher Gabapentin (Neurontin, 900 to 3,600 mg per day) Advice to rest in bed versus advice to stay active for acute low-back pain and sciatica. Cochrane Database Syst Rev. 2010;6:CD007612. Prescribing gabapentin for chronic, non-specific low back pain is not recommended. Patients who suffer from nerve pain, numbness, and tingling in the legs from sciatica or have diabetic Gabapentinoid drugs—specifically gabapentin (Neurontin) and pregabalin (Lyrica)—are increasingly being prescribed for pain because physicians and patients seek alternatives to opioids in the Research suggests that combining gabapentin with epidural steroid injections yields enhanced pain relief, particularly following spinal disc surgery. This combination has shown effective results compared to relying solely on injections and non-steroidal anti-inflammatory drugs (NSAIDs). Medications with good evidence of short-term effectiveness for low back pain are NSAIDs, acetaminophen, skeletal muscle relaxants (for acute low back pain), and tricyclic antidepressants (for chronic low back pain). Evidence is insufficient to identify one medication as offering a clear overall net "The most important finding is that the widespread use of pregabalin or gabapentin for chronic non-specific low back pain, which is the most common chronic pain ailment today, is not supported by evidence," said study author Harsha Shanthanna, MD, MBBS, MSc, PhD, associate professor of anesthesiology and a chronic pain physician at St. Joseph's Healthcare, McMaster University, Hamilton, Canada. Acute, Radicular Back Pain (Sciatica) 80% of patients will ultimately improve without surgery. Treatment is mostly the same as for acute non-radicular back pain; Consider also gabapentin (titrate slowly) or TCAs (nortriptyline, amytriptyline) Gabapentin Oral: Immediate release: 400mg-1200mg PO TID; Spinal stenosis Gabapentin is FDA approved for pain management of a limited number of neuropathic pain conditions; Gabapentin is widely used off-label for various chronic pain conditions and for the treatment of acute pain, making it now one of the most commonly described analgesic drugs Secondary to gabapentin withdrawal, a patient with chronic back pain also developed generalized seizures and status epilepticus . Tapering should always be performed especially in patients taking higher doses; however, withdrawal syndrome can still rarely be observed despite dose tapering [ 62 ]. There is moderate- to high-quality evidence that anticonvulsants are ineffective for treatment of low back pain or lumbar radicular pain. There is high-quality evidence that gabapentinoids have a higher risk for adverse events. PROSPERO-CRD42016046363.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 | |
 |  |
 |  |
 |  |