Gallery
Photos from events, contest for the best costume, videos from master classes.
/GettyImages-1208951024-2e428199871a4aa084804cffb2461e21.jpg) |  |
/GettyImages-966762044-5c170db346e0fb00017d1f3c.jpg) |  |
 | :max_bytes(150000):strip_icc()/Health-abdominal-pain-7495814-HorizV3-8c8e90287dc140aea76cea26e9c670ed.jpg) |
/the-three-major-pairs-of-salivary-glands-141483130-5796772e3df78ceb863e678d.jpg) |  |
 |  |
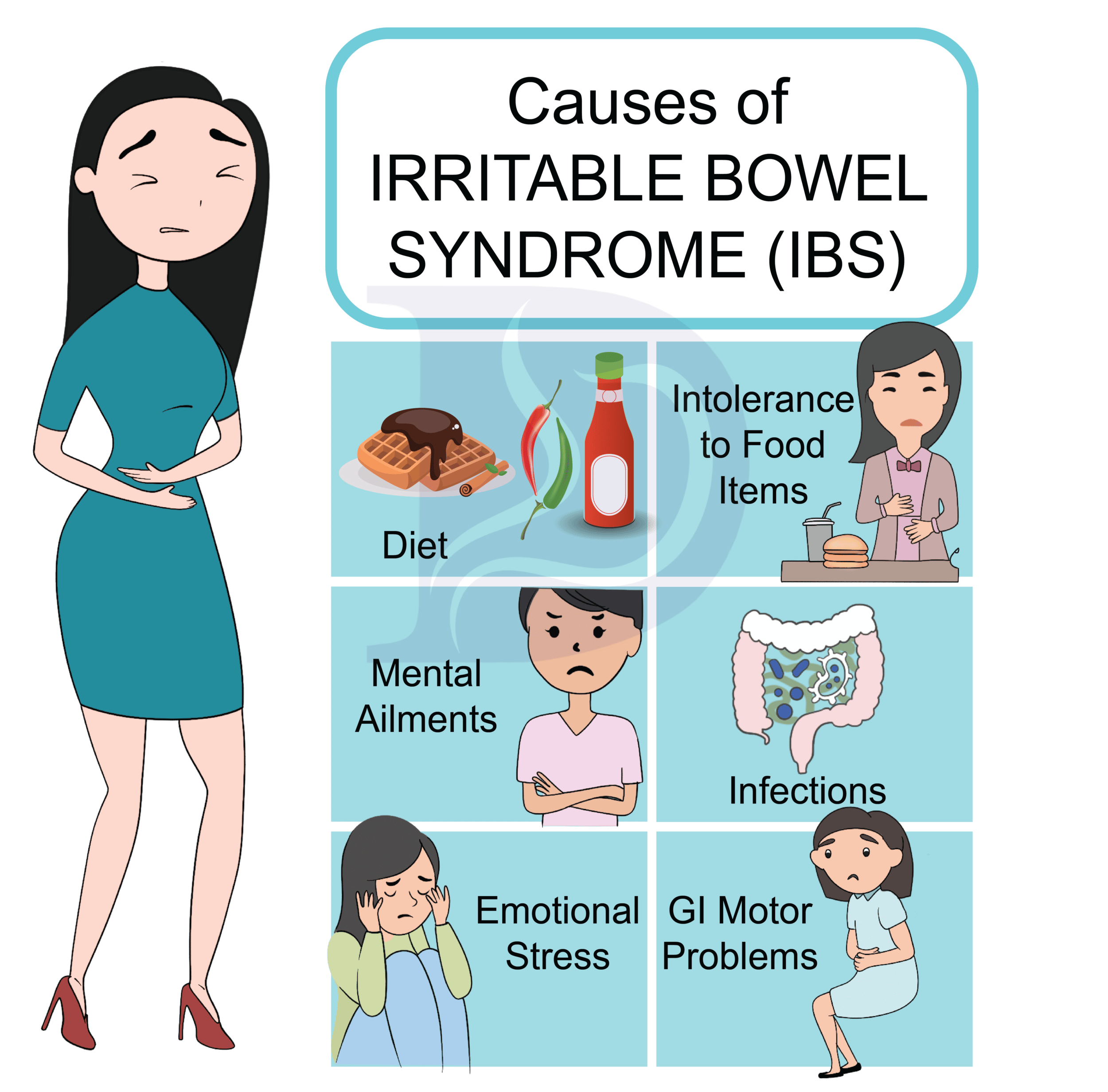 | 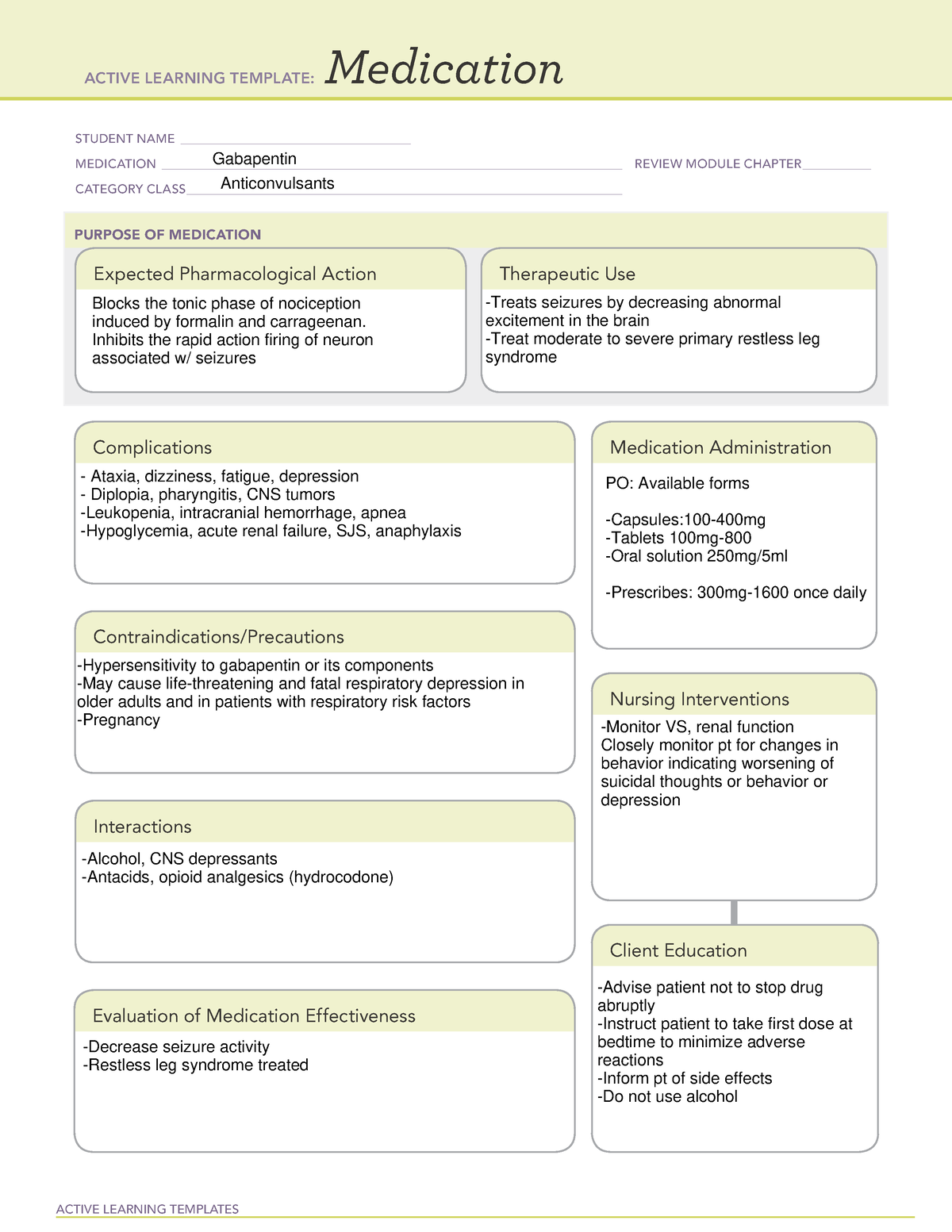 |
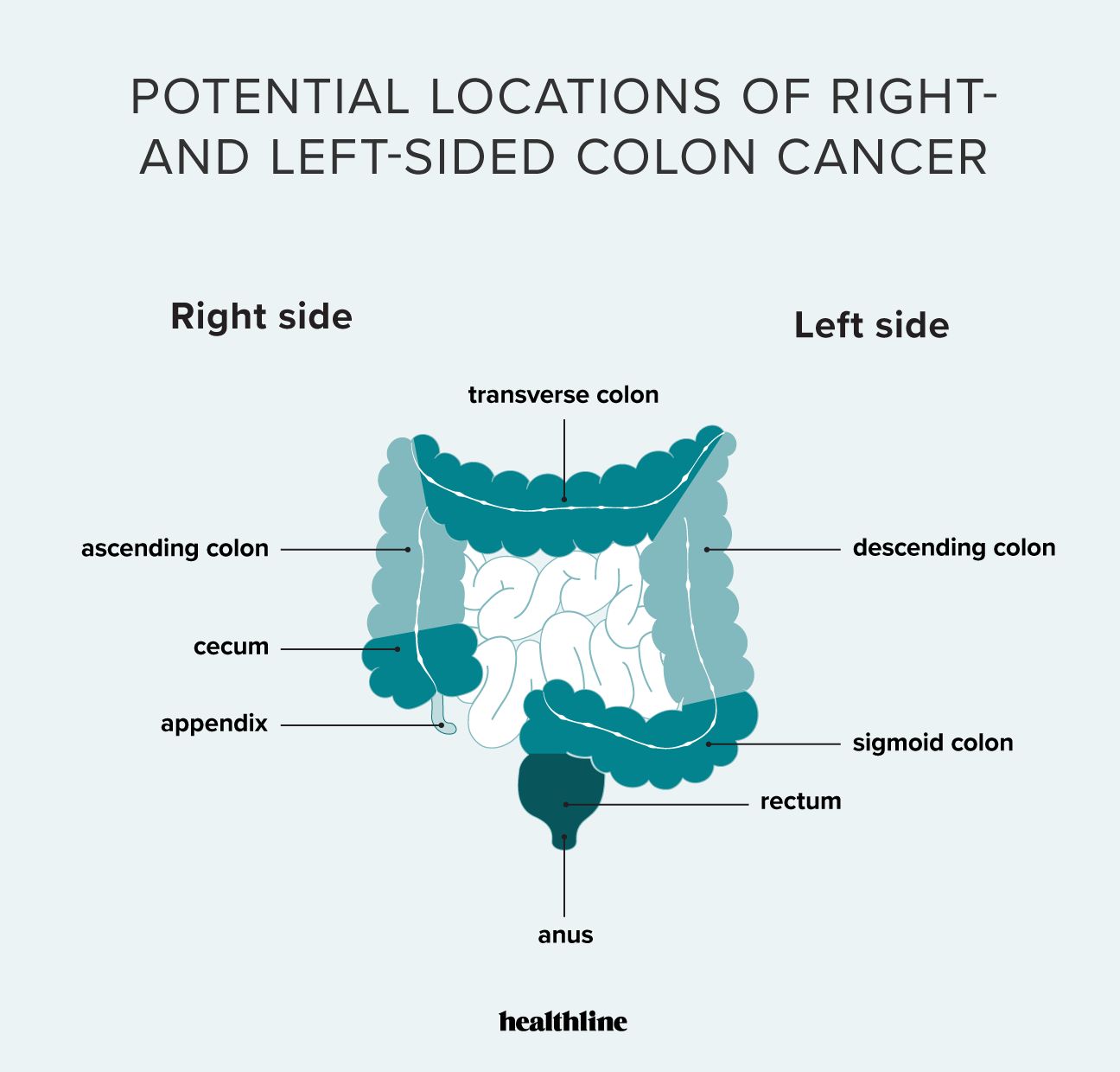
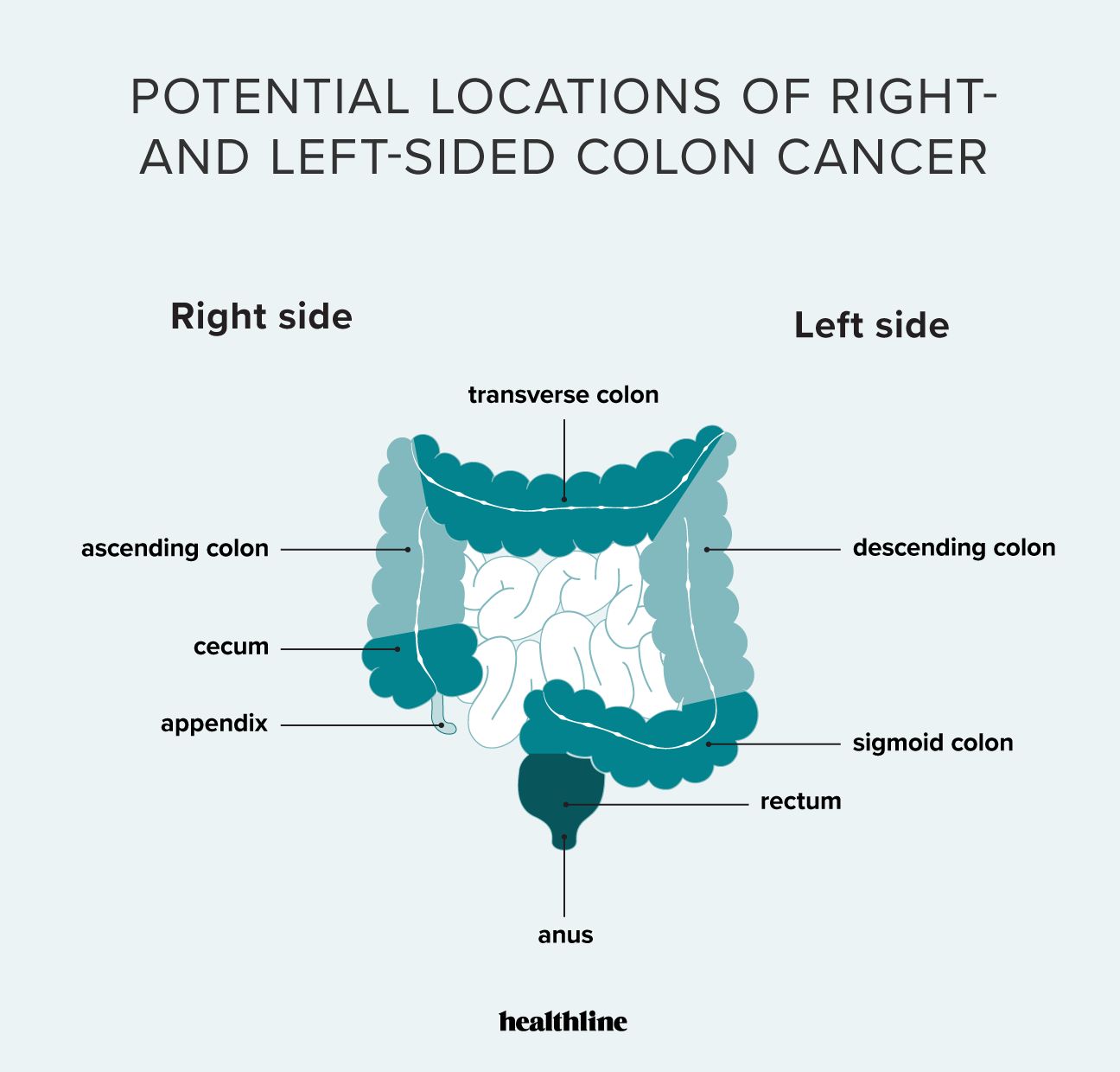
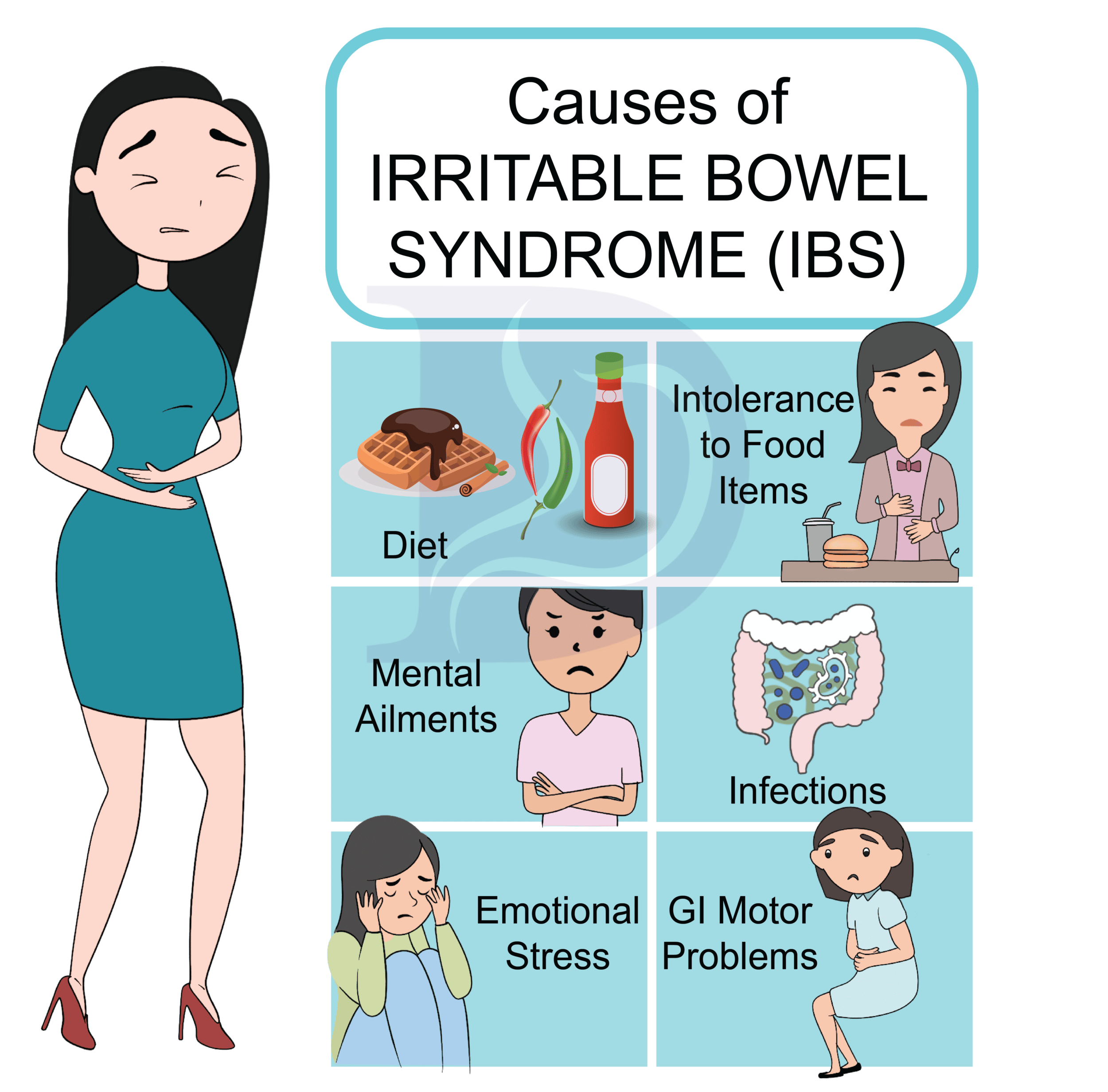
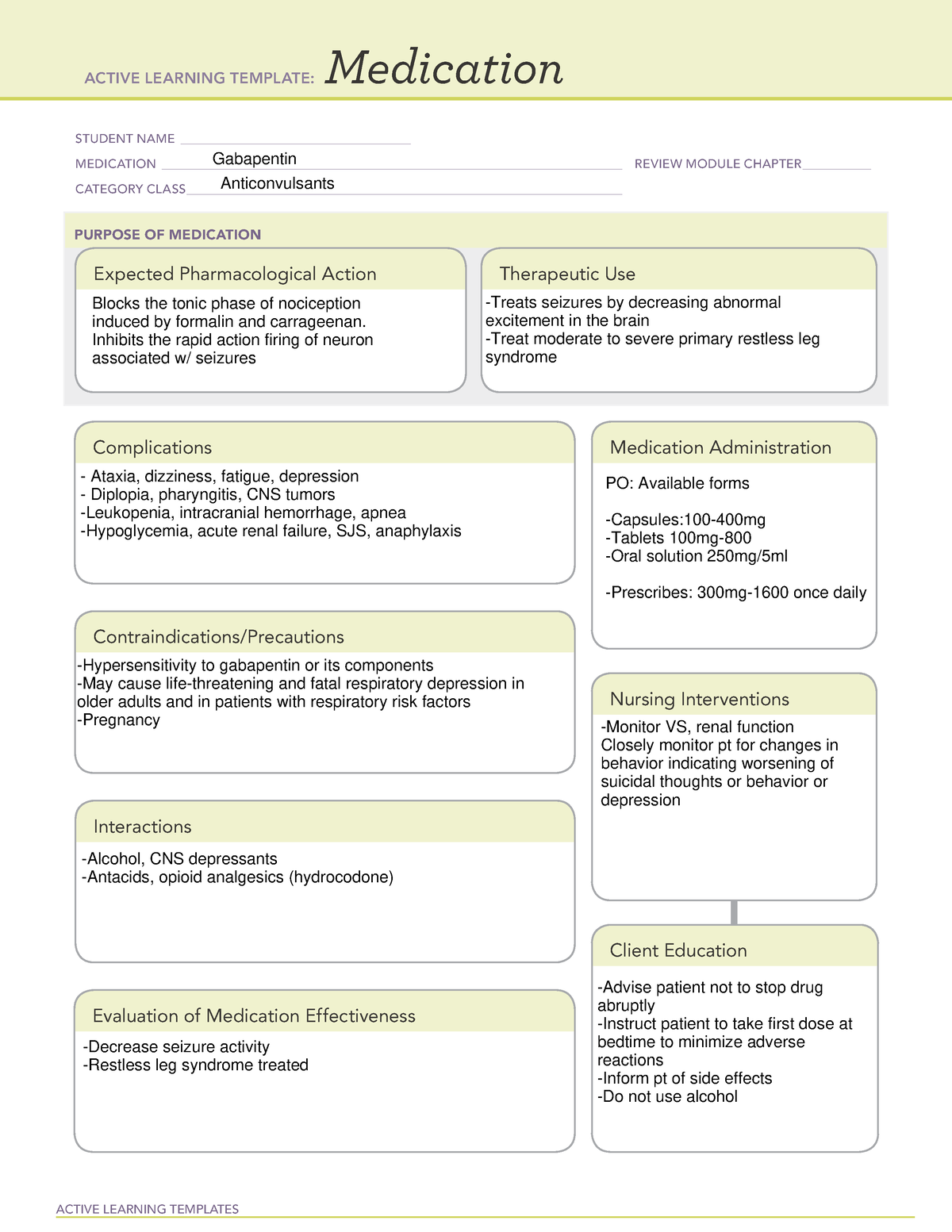
Pain is common in inflammatory bowel disease (IBD), yet many patients feel their pain is not addressed by healthcare professionals. Listening to a patient’s concerns about pain, assessing symptoms and acknowledging the impact these have on daily life remain crucial steps in addressing pain in IBD. While acute pain may be effectively controlled by pain medication, chronic pain is more complex Yes, Gabapentin can be used for the treatment of Irritable Bowel Syndrome (IBS). Many researchers have monitored the effects of gabapentin in the management of IBS and have observed positive results. What does research suggest? Visceral pain is a leading symptom for patients with irritable bowel syndrome (IBS) that affects 10% - 20 % of the world population. Conventional pharmacological treatments to manage IBS-related visceral pain is unsatisfactory. Recently, medications Abstract. Pain control is an integral part of Enhanced Recovery after Surgery (ERAS) protocols for colorectal surgery. While opioid therapy remains the mainstay of therapy for postsurgical pain, opioids have undesired side effects including delayed recovery of bowel function, respiratory depression, and postoperative nausea and vomiting. Gabapentin may make you poop a lot or induce watery, more frequent stools. However, this side effect can vary greatly because some people suffer from constipation and spend days without having a bowel movement. moderate‐to‐severe postoperative pain. Although opioids are the mainstay for acute postoperative pain, their many adverse effects such as respiratory depression, nausea, vomiting, and bowel dysfunction, limits their use. This creates a challenging scenario as Similar to tricyclic antidepressants, anticonvulsant medicines, such as gabapentin and pregabalin, can also be used in low doses to treat chronic nerve pain (neuropathic pain). They can be suitable for use by adults and children with IBD, and are only available on prescription. Background: Gabapentin has been shown to reduce elements of central sensitization in human experimental hyperalgesia. It remains uninvestigated whether gabapentin has beneficial effects for irritable bowel syndrome associated with visceral hypersensitivity. For healthcare professionals. Applies to gabapentin: compounding powder, oral capsule, oral solution, oral tablet, oral tablet extended release. General adverse events. The most common adverse reactions associated with the use of this drug were dizziness, somnolence, and peripheral edema. Gabapentin may cause constipation, but it is not a common side effect. In clinical trials of adults taking gabapentin for nerve pain, only about 4% of people reported constipation. Some people in these trials took an inactive medicine (placebo). It remains uninvestigated whether gabapentin has beneficial effects for irritable bowel syndrome associated with visceral hypersensitivity. Aims: To evaluate the effects of gabapentin on sensory and motor function of the rectum in patients with diarrhoea-predominant irritable bowel syndrome. Pain management in patients with inflammatory bowel disease: insights for the clinician. Therap Adv Gastroenterol. 2012;5(5):339-357. Srinath A, Young E, Szigethy E. Pain management in patients with inflammatory bowel disease: translational approaches from bench to bedside. Inflamm Bowel Dis. 2014;20(12):2433-2449. Gastroenterologists at Massachusetts General Hospital have begun prescribing low-dose gabapentin for patients with functional dyspepsia because it is thought to be capable of relieving visceral pain. Gabapentin as an adjunctive drug could be more effective in reducing the severity of GI symptoms in patients with dyspepsia, especially neurological symptoms (such as pain, reflux, and indigestion). Keywords: Functional dyspepsia, gabapentin, gastrointestinal disorders. Pain is a common complaint among patients with inflammatory bowel disease (IBD). 1 – 3 Pain is a component of several disease activity indices, and it is one of the principal concerns for patients. 4, 5 Pain is a common reason for the poor quality of life (QOL) often seen in patients with IBD. 2, 6, 7 Also, the uncontrollable aspects of pain are associated with profound anxiety. Since I started taking this for sciatic nerve pain, it's like my muscles aren't working for bowel movements. I have always been regular with no problems and that's why I suspect gabapentin is doing it. Gabapentin (Neurontin) is the most frequently prescribed anticonvulsant for the treatment of chronic neuropathic pain. It first gained FDA approval in 1994 for epilepsy, and its labeling was expanded to include neuropathic pain in 2002. Gabapentin inhibits bowel inflammation by regulating mast cell signaling. Furthermore, it activates the PPAR-gamma receptor, which in turn inhibits the activation of NFκB, and consequently results in reduced activation of inflammatory genes involved in inflammatory bowel diseases. Keywords: Colitis; Gabapentin; Peroxisome-gamma. Gabapentin is an anticonvulsant drug that is also used for post-herpetic neuralgia and neuropathic pain. Recently, gabapentin showed anti-inflammatory effect. Nuclear factor kappa B (NFκB) is a regulator of the inflammatory process, and Peroxisome Proliferator-activated Receptor gamma (PPAR-gamma) is an important receptor involved in NFκB Gabapentin can significantly impact bowel function and lead to diarrhea or constipation in some individuals. These effects are thought to occur due to gabapentin’s actions on calcium channels, opioid receptors, and serotonin in the GI tract.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
/GettyImages-1208951024-2e428199871a4aa084804cffb2461e21.jpg) |  |
/GettyImages-966762044-5c170db346e0fb00017d1f3c.jpg) |  |
 | :max_bytes(150000):strip_icc()/Health-abdominal-pain-7495814-HorizV3-8c8e90287dc140aea76cea26e9c670ed.jpg) |
/the-three-major-pairs-of-salivary-glands-141483130-5796772e3df78ceb863e678d.jpg) |  |
 |  |
 |  |