Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
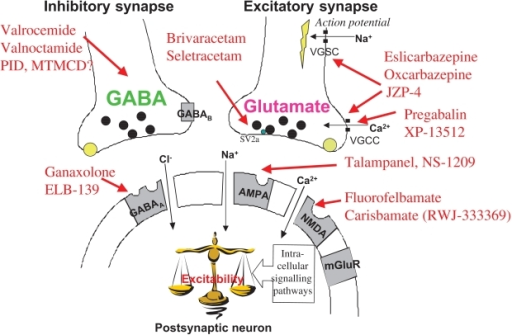 |  |
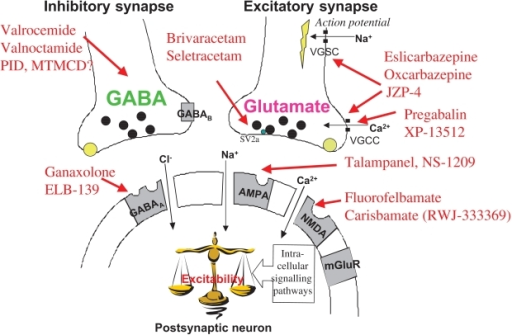
Efficacy of gabapentin in the management of chemotherapy-induced peripheral neuropathy: a phase 3 randomized, double-blind, placebo-controlled, crossover trial (N00C3). Cancer 110 (9), 2110–2118. 10.1002/cncr.23008 [ DOI ] [ PubMed ] [ Google Scholar ] Objective: This study evaluated the effectiveness of gabapentin to treat cancer-related neuropathic pain. Design: This was an open-label study. Two parallel groups of patients were recruited with either treatment-related (radiotherapy, surgery, chemotherapy) or tumor-related neuropathic pain. The proposed mechanism for efficacy of gabapentin in CIPN is related to its binding to the alpha-2-delta type-1 (α 2 δ-1) subunit of voltage-gated calcium channels, which displays increased expression in certain peripheral neuropathy models . Abstract. Neuropathic pain in pediatric oncology results from distinct causes of lesions or disease processes affecting the somatosensory system including chemotherapy-related neuronal injury, solid tumor related involvement of neural structures, post-surgical neuropathic pain including phantom limb pain and post-limb sparing pain, and the complex circumstances of neuropathic pain at the end Given the limited evidence in cancer related neuropathic pain, if ineffective, adjuncts should be weaned and stopped . A mild to moderate benefit of gabapentin for NCP is likely , although robust conclusions cannot be drawn due to the quality of evidence available. Results from a study looking at a combination of gabapentin with morphine showed improvement in sleep, daily activity, mood, and quality of life in cancer-related pain conditions.⁶² Gabapentin also is a useful medication for patients with malignancies of the upper abdomen such as pancreatic cancer; for reducing pain associated with With the initiation of neuropathy, gabapentin was given at 100 mg twice per day. Clinicians could increase gabapentin to 100 mg 3 times daily if the lower daily dose did not resolve symptoms. The abstract reported there was a disappearance of neuropathy symptoms, which continued even with the use of up to 14 total oxaliplatin doses. Three studies examined gabapentin in the short term in cancer‐related neuropathic pain (Caraceni 2004; Mishra 2012; Rao 2007). A parallel‐group study ( Caraceni 2004 ) randomised 121 participants to titration to a maximum of gabapentin 1800 mg daily or placebo, with 10 days of treatment. Gabapentin is effective in the treatment of cancer-related neuropathic pain: a prospective, open-label study. It was approved as an antiepileptic agent in the 1990s and later as an analgesic for neuropathic pain, including cancer-related pain, in which a complicating neuropathic component may occur 19 - 24. Some other symptoms, including hot flashes, nausea and vomiting, are treated by GBP ‘off-label’ 25 - 27. In the second phase of the study we evaluated the response to gabapentin treatment in a group of patients who developed neuropathy. Results: 78.7% of the patients developed chemotherapy related neuropathy. During the course of chemotherapy these patients experienced significant exacerbation of neuropathy symptoms (p < 0.0001), neuropathic pain Results: Recent studies showed effectiveness of gabapentin in improving the pain control in patients with neuropathic cancer pain, already treated with opiates. Moreover, gabapentin appeared promising in reducing the need for high total doses of opioids and avoiding unplanned treatment interruptions for patients with head and neck malignancies Peripheral neuropathy is damage to the nerves that carry messages between the brain, the spinal cord and the rest of the body. Different things can cause peripheral neuropathy, such as diabetes, injury, cancer and some cancer treatments. This information is about cancer-related causes of peripheral neuropathy. Background: To evaluate the efficacy of gabapentin at 20 mg/kg per day in the treatment of vincristine-related neuropathic pain. Procedure: Children aged 1-18 years who developed vincristine-induced neuropathy on a St Jude frontline acute lymphoblastic leukemia trial were prospectively enrolled on a randomized, double-blind, placebo-controlled, phase II trial with two treatment arms The aim of our study was to assess the presence of chemotherapy-induced peripheral neuropathy in ovarian cancer patients treated with first-line paclitaxel and carboplatin chemotherapy and evaluate the effectiveness of gabapentin in treatment of this condition. They received a fixed low-dose of gabapentin (800 mg/day). The control group consisted of 35 cancer patients with similar treatment history and symptomatology, who refused treatment with gabapentin and, therefore, received a fixed-dose combination of naproxen and codeine/paracetamol. BACKGROUND: Gabapentin (GBP), originally an antiepileptic drug, is more commonly used in the treatment of neuropathic pain. In recent years, GBP has been used as an adjunct or primary therapy in non-neuropathic pain, most commonly for the treatment of perioperative and cancer pain. Bruera et al concluded that methadone did not demonstrate an advantage over morphine in the treatment of cancer-related pain in terms of its efficacy or tolerability over a 1-month period.¹⁷ However, it is important to highlight that this RCT included a low number of patients with suspected neuropathic pain and did not include neuropathic Gabapentin, an antiepileptic drug that is structurally related to the neurotransmitter gamma- aminobutyric acid (GABA), has been shown to be effective in treating symptoms from several neuropathic syndromes. The World Health Organization and NCCN guidelines suggest that adjuvant analgesics should be combined with opioids to relieve cancer pain. Pregabalin and gabapentin have been proposed as first-line treatments for cancer-related neuropathic pain; these new-generation anticonvulsants have fewer side-effects than older drugs such as carbamazepine
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |