Gallery
Photos from events, contest for the best costume, videos from master classes.
 | /commonly-used-pain-medication-2564482_FINAL-5c3b9479c9e77c0001c79d66.png) |
 |  |
 |  |
 |  |
 |  |
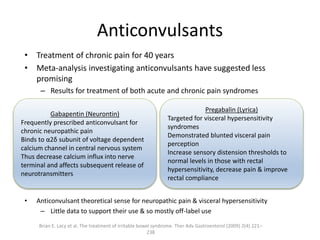 |  |
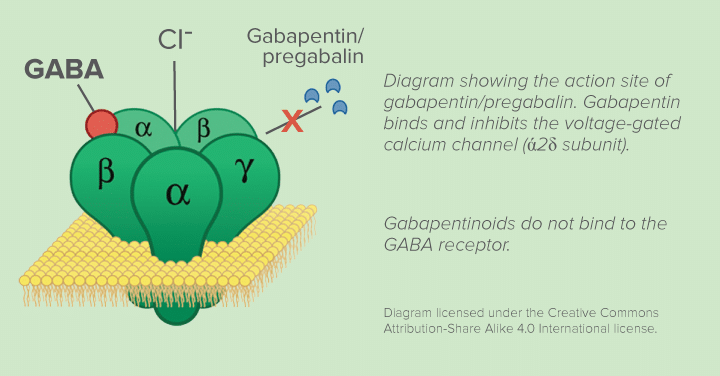
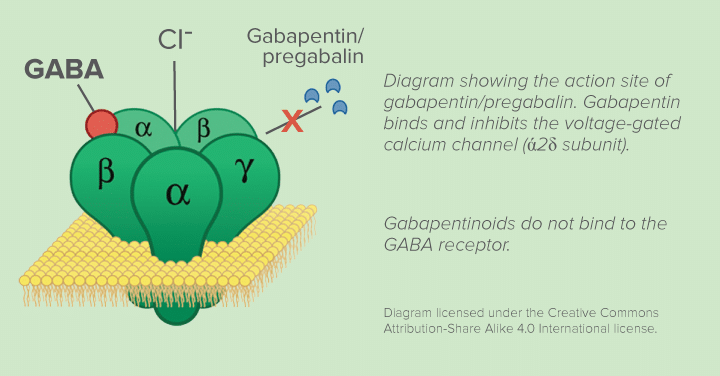
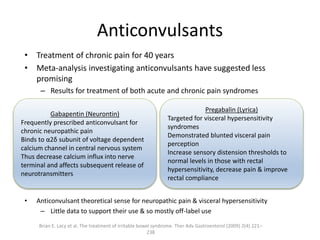
Gabapentin for chronic neuropathic pain in adults. Bottom line. There is moderate‐quality evidence that oral gabapentin at doses of 1200 mg daily or more has an important effect on pain in some people with moderate or severe neuropathic pain after shingles or due to diabetes. Background. Neuropathic pain comes from damaged nerves. Gabapentin is FDA approved for pain management of a limited number of neuropathic pain conditions; Gabapentin is widely used off-label for various chronic pain conditions and for the treatment of acute pain, making it now one of the most commonly described analgesic drugs Since gabapentin is an anticonvulsant with a proven analgesic effect in various neuropathic pain syndromes, we sought to study the efficacy of the anticonvulsant gabapentin as treatment for pain in patients with CRPS I. Gabapentin provides pain relief of a high level in about a third of people who take if for painful neuropathic pain. Adverse events are frequent, but mostly tolerable. Gabapentin is widely used for the treatment of pain, particularly in patients with chronic neuropathic pain. Wiffen and colleagues performed a systematic review of randomized trials assessing the The clinical impression is that they are useful for chronic neuropathic pain, especially when the pain is lancinating or burning. Objectives: To evaluate the analgesic effectiveness and adverse effects of gabapentin for pain management in clinical practice. Background. This is an update of a Cochrane review published in 2011. That review was an update of a previous Cochrane review titled 'Gabapentin for acute and chronic pain' (Wiffen 2005), which itself was an extension to a review previously published in The Cochrane Library on 'Anticonvulsant drugs for acute and chronic pain' (Wiffen 2000). The analgesic efficacy of TCAs has been demonstrated in a number of neuropathic and other chronic pain conditions, including headaches, low back pain, irritable bowel syndrome, and fibromyalgia. 62, 66 The evaluation of TCAs for treatment of neuropathic pain, in comparison to anticonvulsants such as gabapentin and pregabalin, has produced Abstract Introduction: Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) and interstitial cystitis/bladder pain syndrome collectively referred to as urologic CPPS (UCPPS) is defined by the absence of identifiable bacterial infection as a cause for the chronic pain and urinary symptoms. Management of patients with chronic pain in primary care practice can be difficult. When faced with patients who are struggling with pain, the path of least resistance is often to write a This topic will discuss an approach to pharmacologic management based on the type of pain, and an overview of drug choices. Graded treatment recommendations can be found in treatment topics for specific chronic pain conditions (eg, chronic back pain, postherpetic neuralgia, fibromyalgia). There's no known cure for complex regional pain syndrome (CRPS), but a combination of physical treatments, medicine and psychological support can help manage the symptoms. It's estimated around 85% of people with CRPS slowly experience a reduction in their pain and some of their symptoms in the first 2 years. Coexisting chronic overlapping pain conditions that contribute to CPP include back pain, bladder pain syndrome (interstitial cystitis), chronic fatigue, chronic migraines, endometriosis A randomized controlled trial of amitriptyline versus gabapentin for complex regional pain syndrome type I and neuropathic pain in children. Canadian Journal of Pain, 2014 61: S1–S165). 8. Ching, C.B., et al., Interdisciplinary pain management is beneficial for refractory orchialgia in children. Journal of pediatric urology, 2015. In patients with neuropathic pain, this review shows that gabapentin is associated with a greater likelihood of achieving substantial or moderate pain relief vs placebo. The general approach to the management of chronic non-cancer pain and nonpharmacologic therapies for chronic pain are discussed separately. Evaluation of chronic pain and the use of opioids for chronic non-cancer pain are also discussed separately. (See "Approach to the management of chronic non-cancer pain in adults".) Chronic pain is a serious health condition that can lead to complications beyond physical symptoms. People with chronic pain may experience depression, anxiety and trouble sleeping. Chronic pain is pain that is long lasting. It can affect every aspect of life — from relationships to finances. Baron R. Mechanistic and clinical aspects of complex regional pain syndrome (CRPS). Novartis Found Symp 2004;261:220–33; discussion 233–8, 256–61. Search PubMed; Harden RN, Bruehl S, Stanton-Hicks M, Wilson PR. Proposed new diagnostic criteria for complex regional pain syndrome. Pain Med 2007;8:326–31. Search PubMed; Mellick LB, Mellick GA. For chronic pain, topical lidocaine is usually used in the form of a patch or plaster. Data supporting the efficacy of topical lidocaine are limited , and the best evidence suggests that it may be beneficial for postherpetic neuralgia, and possibly for painful diabetic neuropathy. Chronic pelvic pain in women is defined as persistent, noncyclic pain perceived to be in structures related to the pelvis. 1 An arbitrary duration of six months is usually considered chronic. A
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 | /commonly-used-pain-medication-2564482_FINAL-5c3b9479c9e77c0001c79d66.png) |
 |  |
 |  |
 |  |
 |  |
 |  |