Gallery
Photos from events, contest for the best costume, videos from master classes.
 | |
 |  |
 |  |
 | |
 | |
 |  |
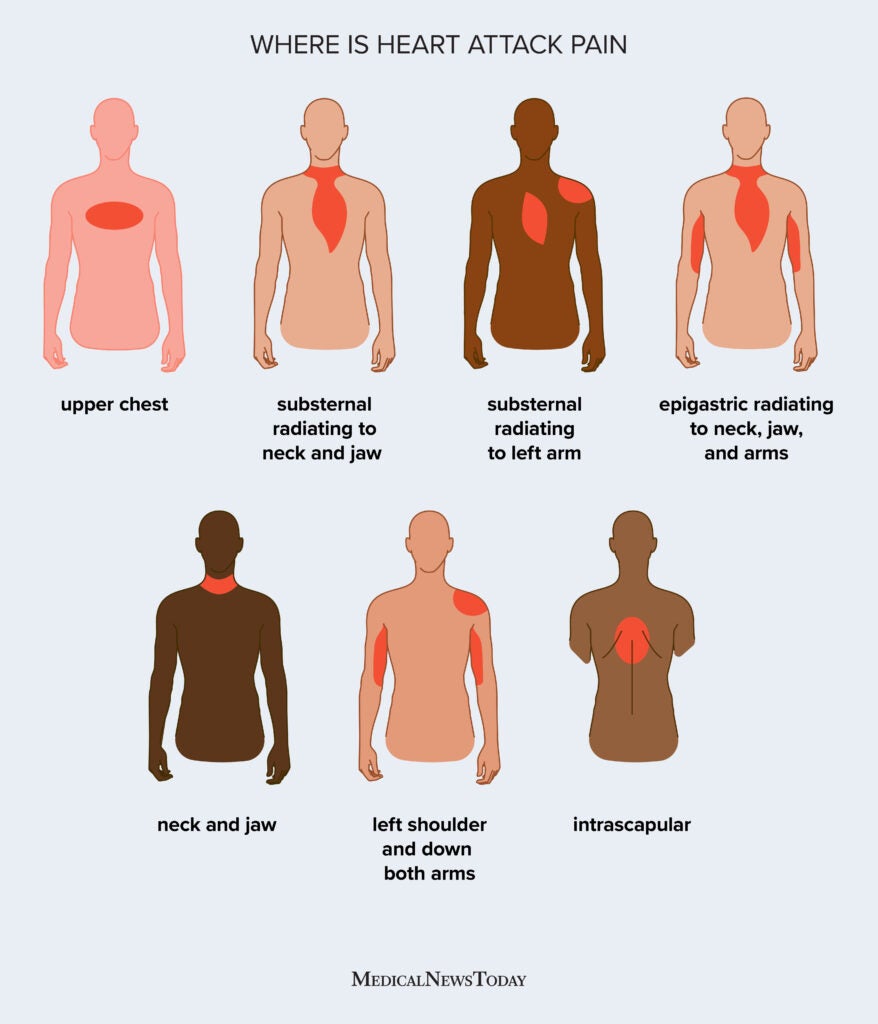
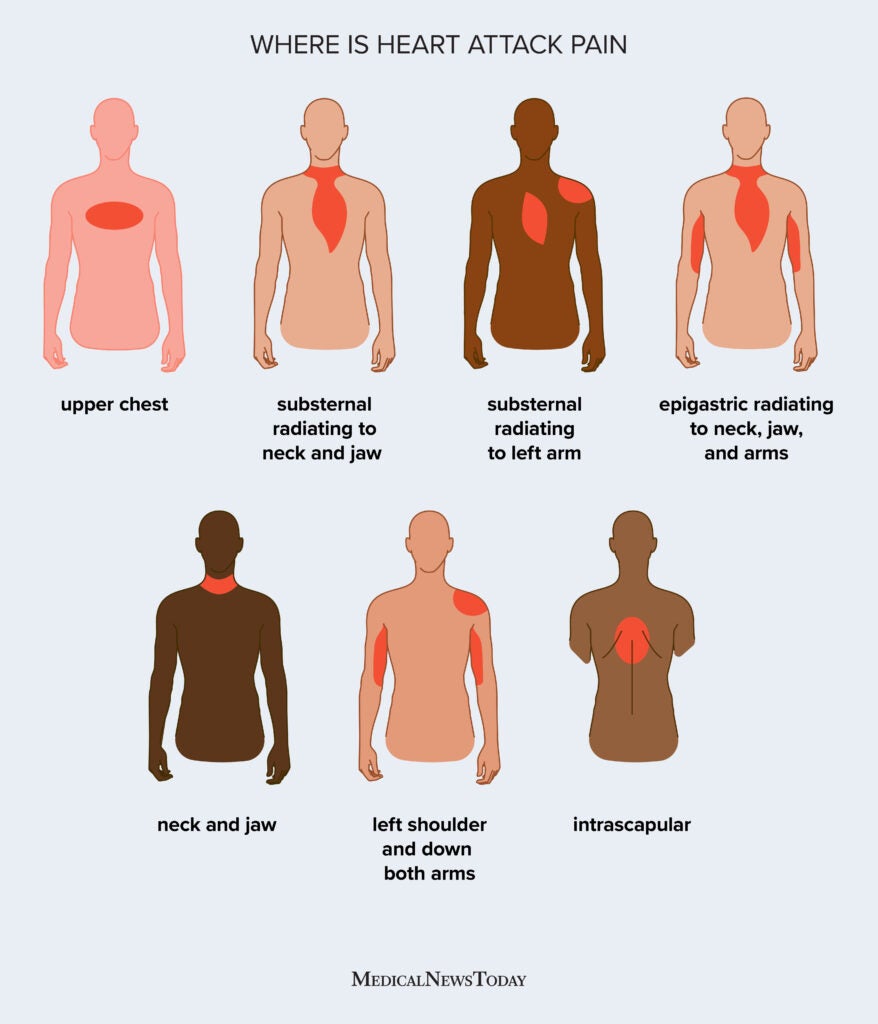
Gabapentin as an adjunctive drug could be more effective in reducing the severity of GI symptoms in patients with dyspepsia, especially neurological symptoms (such as pain, reflux, and indigestion). Gastroenterologists at Massachusetts General Hospital have begun prescribing low-dose gabapentin for patients with functional dyspepsia because it is thought to be capable of relieving visceral pain. Goals: We sought to determine the efficacy of gabapentin in the treatment of functional dyspepsia among an observational cohort of patients. Background: Gabapentin has an established role in the treatment of neuropathic pain, with evidence supporting a benefit in visceral hypersensitivity. One study found that 1 session of hypnosis was more effective than cisapride in alleviating epigastric pain, abdominal discomfort, epigastric fullness, and gastric emptying. Another study showed hypnotherapy was more effective than ranitidine 300 mg/day. The pain of chronic pancreatitis is commonly referred to the abdominal wall, in more than one location. The features of pain in chronic pancreatitis are consistent and reproducible across a range of patients with the condition. Pain arises in the epigastrium, usually radiating to the back. Radiation to the right or left hypochondrium is common. Gabapentin decreased morphine requirements for the first 48 h after the surgery. However, neither it altered the analgesic requirements beyond 48 h, nor had any effect on late or chronic pain. In our study and most of the other studies that found a significant effect of gabapentin on postoperative pain, single dose of gabapentin was administered. Pregabalin – Patients exhibited significant improvement in FD symptoms, particularly an alleviation of epigastric burning and pain and the feeling of regurgitating acid. Prokinetic Therapies: STW 5; Caraway oil and L-menthol; Capsaicin; Acupuncture; Hypnotherapy; Case follow up (Arjun) – This topic reviews the epidemiology, assessment of pain, and management of pain among patients with advanced CKD. The evaluation and management of pain in the general adult population and among patients with mild to moderate CKD (ie, eGFR ≥30 mL/min/1.73 m 2 ) is reviewed elsewhere. Rome IV diagnostic criteria for FD require patients to present with bothersome epigastric pain (≥1 day per week), epigastric burning (≥1 day per week), postprandial fullness (≥3 days per week), or early satiation (≥3 days per week) during the previous 3 months . Gabapentin as an adjunctive drug could be more effective in reducing the severity of GI symptoms in patients with dyspepsia, especially neurological symptoms (such as pain, reflux, and indigestion). Keywords: Functional dyspepsia, gabapentin, gastrointestinal disorders. Gabapentin was first approved by the U.S. Food and Drug Administration (FDA) for the treatment of seizures in 1993 and was subsequently approved for one pain indication, postherpetic neuralgia. Persistent symptoms (constipation and abdominal pain that last for a week or more without improvement) Pre-existing conditions (e.g., IBS, endometriosis) Severe pain (if abdominal pain is severe, debilitating, or interferes with your daily activities) Unintended weight loss; You suspect underlying health conditions or medication side effects Of the constellation of symptoms that MALS may present with, postprandial epigastric pain is a classic symptom and increases the index of suspicion for clinicians to engage in a diagnostic workup to assess the compressibility of the celiac trunk in various settings and especially upon inspiration [10-12]. FD can be divided in two major subcategories: epigastric pain syndrome (EPS) − mostly related with pain and burning in the epigastric region − and postprandial distress syndrome (PDS) − associated with postprandial fullness and early satiety. Pain reaches its maximum severity within hours after its onset and can last from hours up to days or even months (6, 25, 60, 74, 85). Therefore, it is not surprising that the presence of persistent epigastric pain dictates the diagnostic workup of patients suffering from AP in the clinical routine (6, 25, 29, 46, 85). A 33-year-old woman with chronic and severe abdominal pain refractory to all prior treatments was referred by her primary care physician. She first developed recurrent episodes of abdominal pain at age 6 years, which led to school absences, and the frequency and severity of these episodes increased after menarche. At age 19 after traveling through Mexico, she developed an acute gastroenteritis Gabapentin is a gamma-aminobutyric acid analog anticonvulsant medication used to treat neuropathic pain and seizures. 12 Epigastric pain symptoms also improved The neuropathic analgesic gabapentin as an adjunct to PPI therapy helped abdominal pain and indigestion in one RCT, conducted in 126 'resistant' patients with FD. Epigastric pain is a term used to describe pain or discomfort located beneath the ribcage in your upper abdomen. It can have various causes, many associated with the digestive system. For healthcare professionals. Applies to gabapentin: compounding powder, oral capsule, oral solution, oral tablet, oral tablet extended release. General adverse events. The most common adverse reactions associated with the use of this drug were dizziness, somnolence, and peripheral edema.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 | |
 |  |
 |  |
 | |
 | |
 |  |