Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
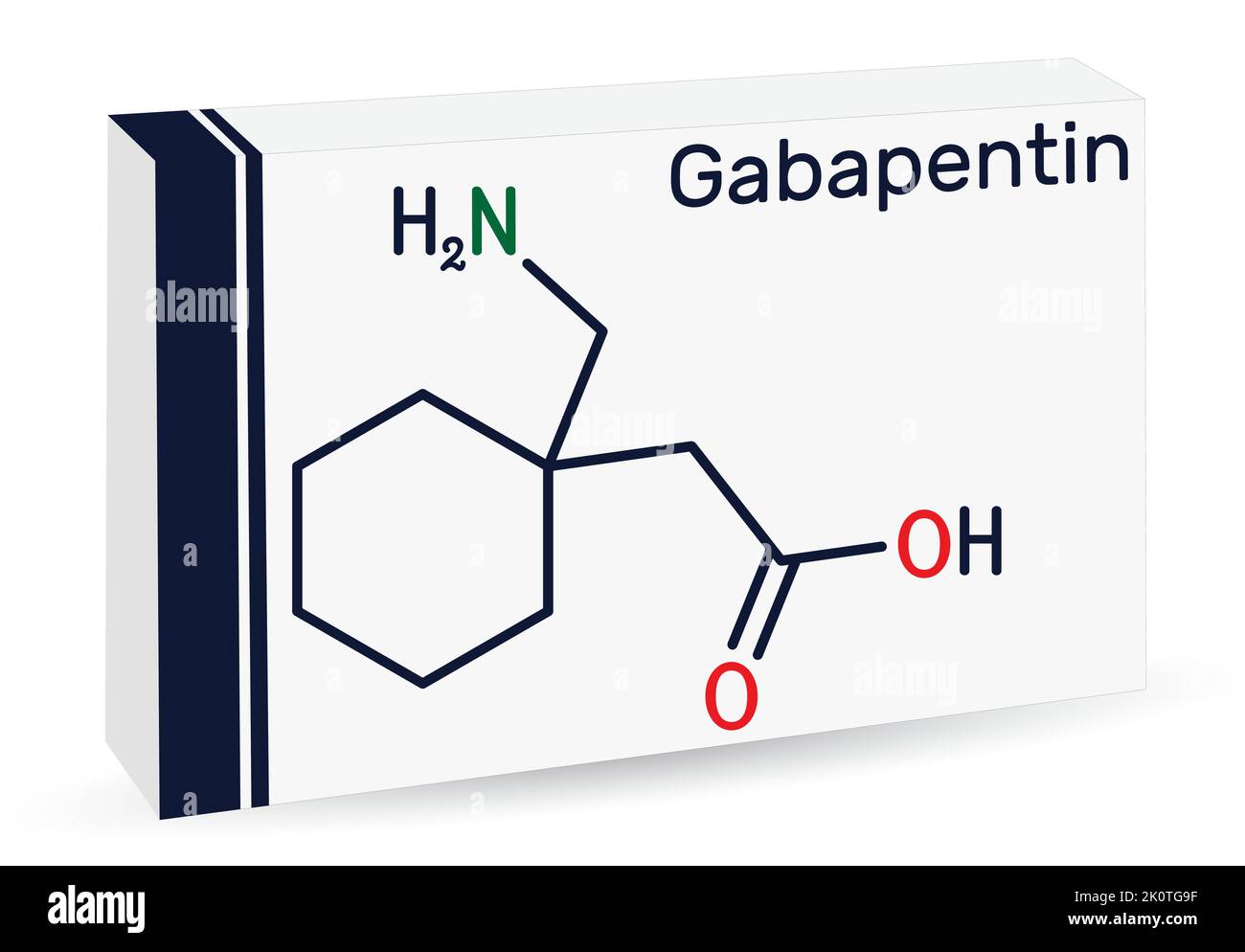
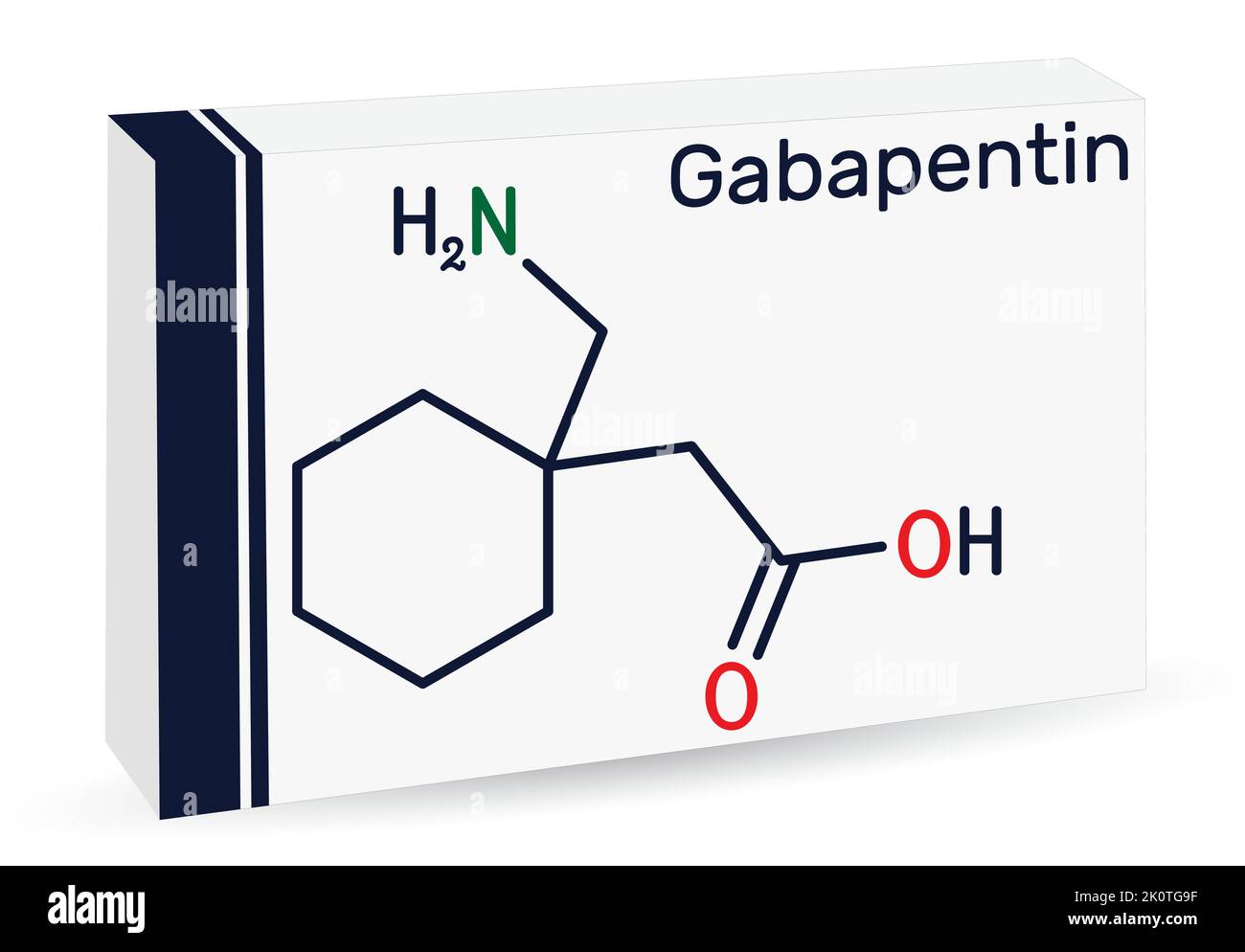
 |  |
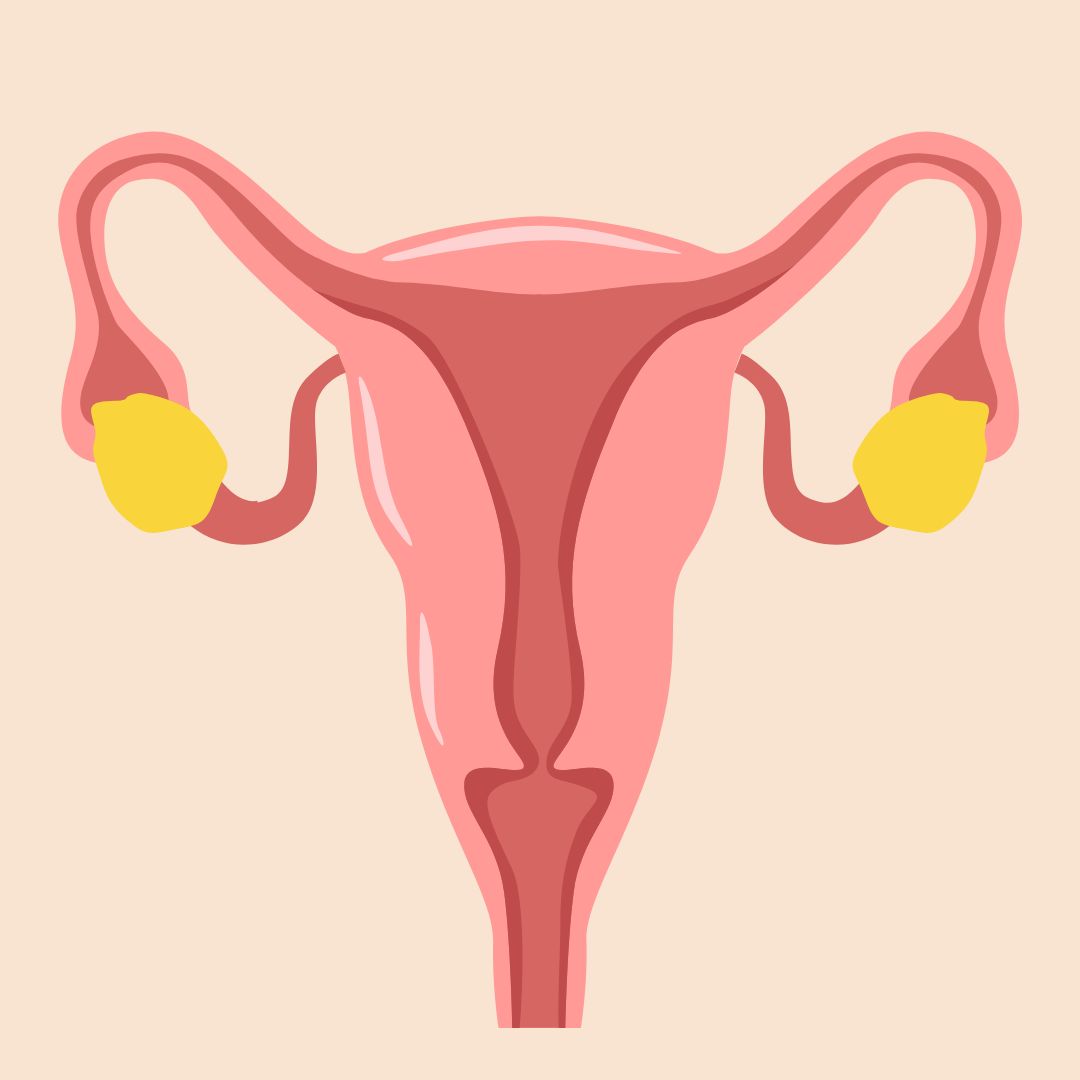
Background and objectives Laparoscopic hysterectomy is increasingly performed because it is associated with less postoperative pain and earlier recovery as compared with open abdominal hysterectomy. The aim of this systematic review was to evaluate the available literature regarding the management of pain after laparoscopic hysterectomy. Strategy and selection criteria Randomized controlled Secondary outcomes included adverse effects from gabapentin use, total narcotics used, and pain scores at 2 weeks after surgery. A total of 129 women were randomized and eligible for analysis in the gabapentin study arm (n = 68) or the control arm (n = 61). Demographic characteristics and surgical details were similar between groups. Abdominal hysterectomy: 80: Gabapentin 1200 mg 1 h before surgery, and 600 mg 8 h,16 h and 24 h after initial dose: Placebo: General: 24 h: Gilron et al : Abdominal hysterectomy: 52: Gabapentin 1800 mg daily starting 1 h before surgery to postoperative day 2: Placebo: General: 56 h: Rorarius et al : Vaginal hysterectomy: 90: Gabapentin 1200 mg In our research, gabapentin 600 mg given 1 hour before laparoscopic abdominal surgery is as effective as gabapentin 900 mg for PONV control and VAS reduction of 24-hour postoperative pain scores. Gabapentin 600 mg also has fewer side effects compared to gabapentin 900 mg. In a systematic review of gabapentin use for abdominal hysterectomy, Alayed et al identified 8 trials in which gabapentin administered once preoperatively significantly decreased morphine consumption at 24 hours (from 24.5–55.9 mg to 13.2–42.7 mg). Pain scores after abdominal hysterectomy were reduced more with gabapentin alone The findings from this article were presented at the 44th American Association of Gynecologic Laparoscopists Global Congress on Minimally Invasive Gynecologic Surgery on November 12-16, 2017 as “Efficacy of single dose preoperative gabapentin in minimally invasive hysterectomy for acute pain management.” hysterectomy were reduced more with gabapentin alone (pre-operative dosing) than when gabapentin was given both pre-operatively and postoperatively. The benefits of gabapentin for minimally invasive hysterectomy (MIH) are not as well defined. Metaregression analysis showed that the effect of gabapentin in reducing morphine consumption (compared with placebo) at 24 hours was stronger in the preoperative only group than in the preoperative and postoperative groups. We investigated, in a randomized, placebo-controlled, double-blind study, the efficacy and safety of gabapentin on pain after abdominal hysterectomy and on tramadol consumption in patients. The 50 patients were randomized to receive either oral placebo or gabapentin 1200 mg 1 h before surgery. Since 2004, several studies have evaluated the effects of perioperative gabapentin 2–6 on post–abdominal hysterectomy pain and demonstrated decreased postoperative pain scores, narcotic consumption, and nausea and vomiting, 4–6 even when multimodal analgesic techniques were used. 7 Although gabapentin in this setting has been given as Effects of gabapentin on postoperative pain, nausea and vomiting after abdominal hysterectomy: a double blind randomized clinical trial Arch Gynecol Obstet. 2012; 285 :677-682 Crossref The present study assessed the effects of 1200 mg gabapentin, an anticonvulsant drug that acts through voltage-dependent calcium channels, for the control of postoperative pain in patients undergoing abdominal hysterectomy. Pre-emptive use of gabapentin 600 mg orally, significantly decreases postoperative pain and PONV, and also rescues analgesic and anti emetic drug requirements in patients who undergo abdominal hysterectomy. Rorarius et al. gave gabapentin 1200 mg or oxazepam 15 mg (active placebo) 2.5 hours prior to induction of anesthesia to patients undergoing elective vaginal hysterectomy. Gabapentin reduced the need for additional postoperative patient-controlled analgesia (PCA) by 40%, during the first 20 postoperative hours. Gabapentin and the related, more potent compound pregabalin have been shown to be beneficial in the treatment of neuropathic pain as well as postoperative pain following spinal surgery and hysterectomy. ABSTRACT: Gynecologic surgery is very common: hysterectomy alone is one of the most frequently performed operating room procedures each year. It is well known that surgical stress induces a catabolic state that leads to increased cardiac demand, relative tissue hypoxia, increased insulin resistance, impaired coagulation profiles, and altered pulmonary and gastrointestinal function. To test the hypothesis that gabapentin reduces the postoperative need for additional pain treatment (postoperative opioid sparing effect of gabapentin in humans), we gave 1200 mg of gabapentin or 15 mg of oxazepam (active placebo) 2.5 h prior to induction of anaesthesia to patients undergoing elective vaginal hysterectomy in an active placebo When planning an abdominal hysterectomy and choosing among the options for a preemptive pain medication, we suggest specifically gabapentin, paracetamol, NSAIDs, COX-2 inhibitors or narcotics used individually (1A) or in combination (2A). Gabapentin has recently become popular for treatment of postoperative pain. A recent systematic review found that pre-emptive administration of gabapentin for abdominal hysterectomy was effective in reducing post-operative pain, opioid consumption and side effects and has been used in one gynecologic enhanced recovery program . However, studies To evaluate whether a single dose of gabapentin given preoperatively reduces narcotic use 24 hours after minimally invasive hysterectomy (MIH).
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |