Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 | |
 |  |
 |  |
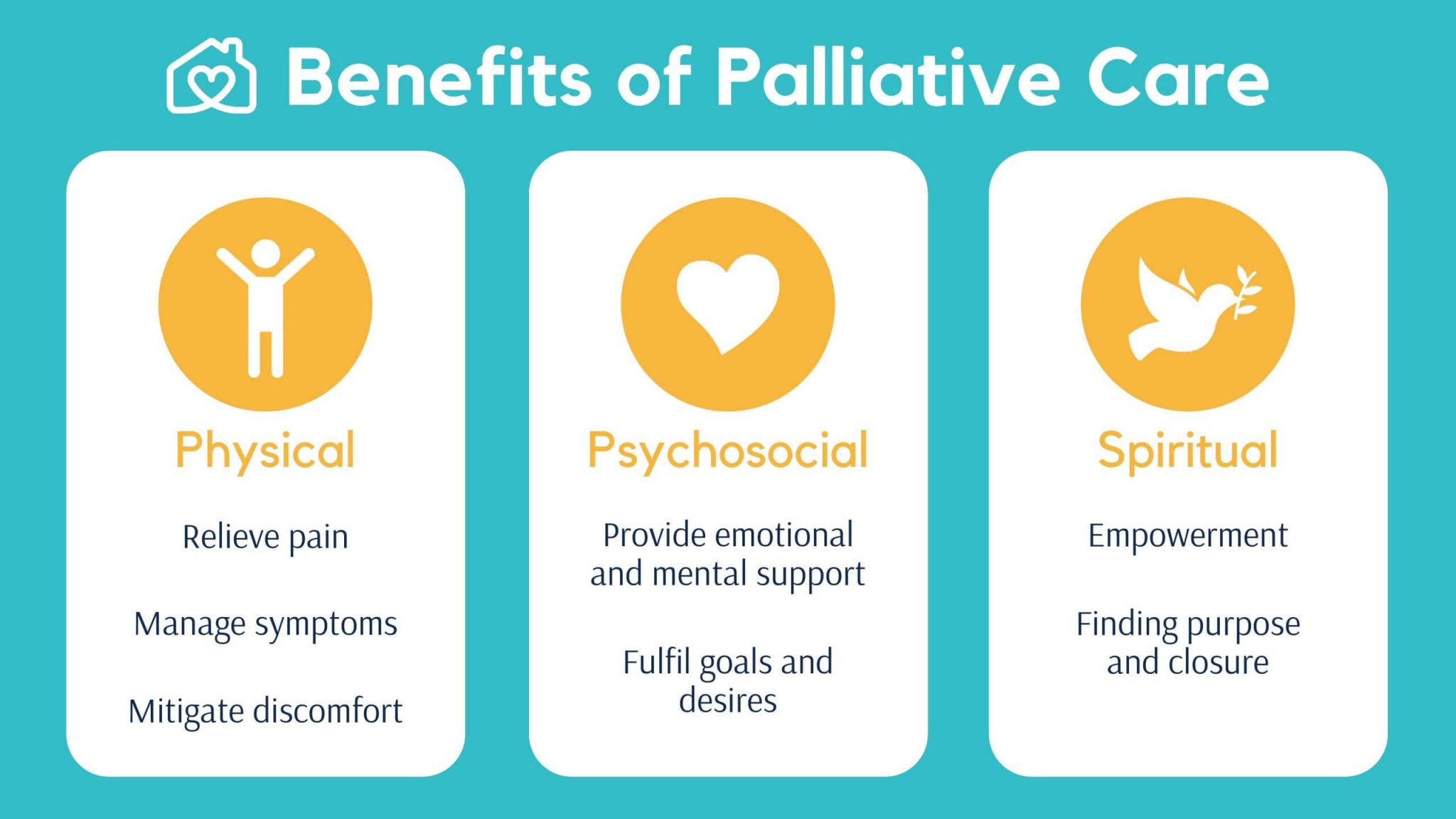
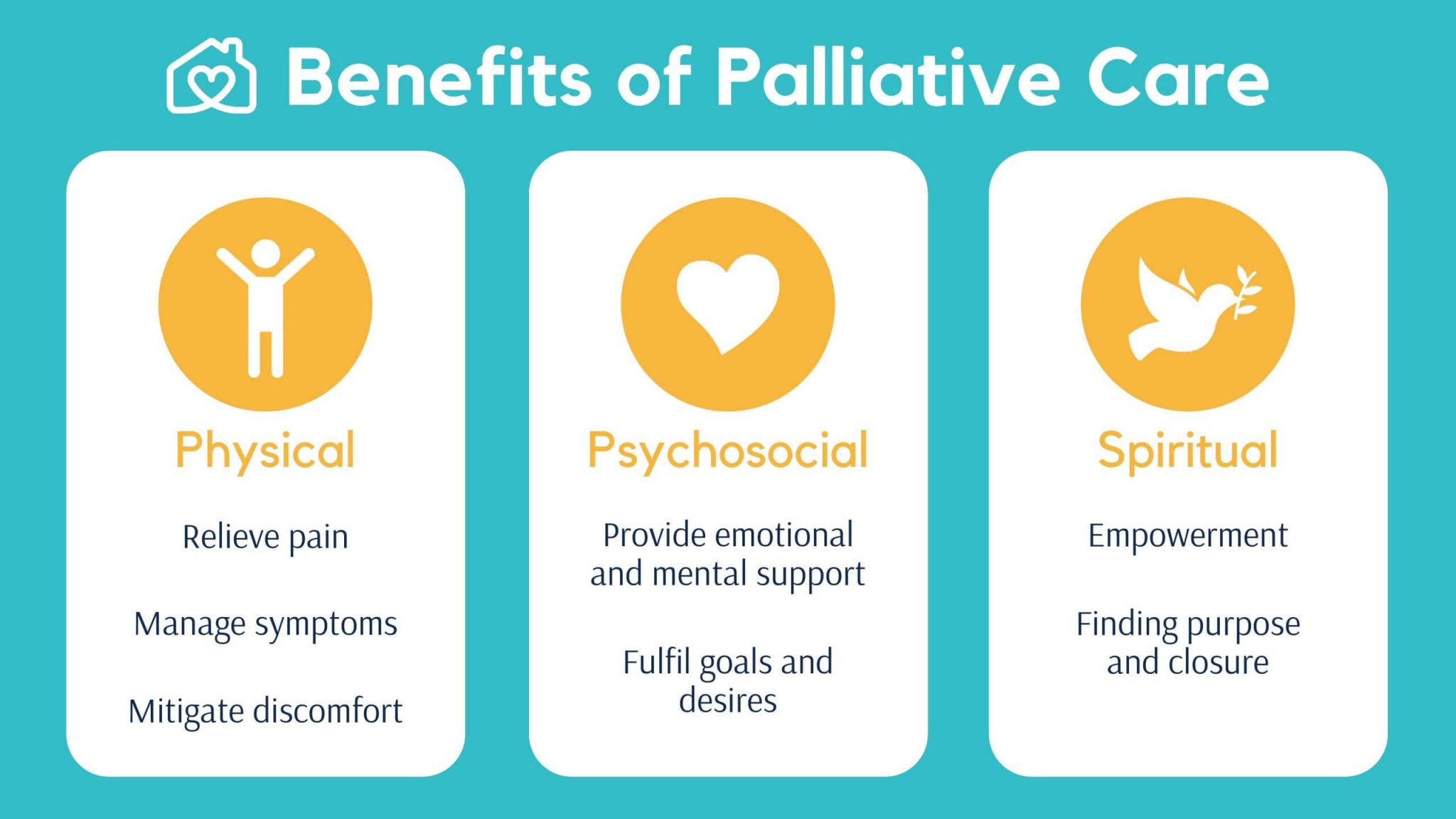
Chronic neuropathic pain is common and may be related to: the principal disease or diseases the person has (for example cancer or multiple sclerosis) treatment (for example post-operative neuropathic pain or chemotherapy-induced peripheral neuropathy) other co-morbid conditions (for example post-herpetic neuralgia or diabetic neuropathy). The purpose of this retrospective cohort study was to compare clinically meaningful pain reduction and other relevant outcomes among patients prescribed either gabapentin or pregabalin at the University of Arkansas for Medical Sciences (UAMS) Palliative Care Clinic (PCC). Gabapentin, a γ-amino butyric acid analogue antiepileptic drug, is commonly prescribed for neuropathic pain in hospice/palliative care. Most of the evidence however relates to non-malignant, chronic pain syndromes (diabetic neuropathy, postherpetic neuralgia, central pain syndromes, fibromyalgia). The recommendation to manage any treatable causes of neuropathic pain is based on a textbook on symptom relief in palliative care [Regnard, 2022], a textbook of symptom management in advanced cancer [Twycross, 2016], the Palliative Care Formulary [Wilcock, 2020], and a palliative care guideline [NHS Scotland, 2021]. Palliative care can be provided in hospitals, nursing homes, outpatient palliative care clinics and certain other specialized clinics, or at home. Medicare, Medicaid, and insurance policies may cover palliative care. Veterans may be eligible for palliative care through the Department of Veterans Affairs. Private health insurance might pay for Gabapentin, a γ-amino butyric acid analogue antiepileptic drug, is commonly prescribed for neuropathic pain in hospice/palliative care. Most of the evidence however relates to non-malignant, chronic pain syndromes (diabetic neuropathy, postherpetic neuralgia, central pain syndromes, fibromyalgia). Objectives: The main objective of this study was to describe the pattern of gabapentin use as an adjuvant analgesic for cancer-related neuropathic pain in patients admitted to a tertiary palliative care unit. Methods: A retrospective medical chart review for 150 patients admitted to a tertiary palliative care unit over a period of 10 months. In a recent article by Caraceni et al., 1 gabapentin was judged to be efficacious as an adjuvant analgesic for neuropathic cancer pain in 20 out of 22 patients. We report on our experience of gabapentin, which was associated with a much lower incidence of efficacy. Patients suitable for gabapentin should have a clear neuropathic pain syndrome, characterized by sharp, shooting, lancinating and/or burning pain, in a nerve root (radicular) or stocking/glove distribution. Adult dosing: Gabapentin is started at low doses (100 mg to 300 mg total daily) and increased by 100 – 300 mg every 1-3 days to effect. For particular causes of pain in palliative care, aggressive pain management techniques may be indicated, including radiation treatment, surgery, chemotherapy, and interventional pain techniques (including injections [eg. nerve blocks], implantable analgesic pumps, spinal cord stimulators). The aggregation of gabapentin having a doubtful, possible or probable contribution to serious event development averaged 5.2% over the study period which accords well with the 7% for severe AEs reported in a similar pharmacovigilance study in an unselected adult hospice/palliative care population prescribed gabapentin for neuropathic pain. 10 Gabapentin, a γ-amino butyric acid analogue antiepileptic drug, is commonly prescribed for neuropathic pain in hospice/palliative care. Most of the evidence however relates to non-malignant, chronic pain syndromes (diabetic neuropathy, postherpetic neuralgia, central pain syndromes, fibromyalgia). Consider capsaicin cream for people with localised neuropathic pain who wish to avoid, or who cannot tolerate, oral treatments. NICE draft guidance reports that both amitriptyline and gabapentin represent good value for money. Gabapentin prescribed at standard doses for advanced cancer and severe neurological injury in children under a pediatric palliative care service was associated with generally improved pain intensity at previously described levels of adverse effects. Gabapentin, a γ-amino butyric acid analogue antiepileptic drug, is commonly prescribed for neuropathic pain in hospice/palliative care. Most of the evidence however relates to non-malignant, chronic pain syndromes (diabetic neuropathy, postherpetic neuralgia, central pain syndromes, fibromyalgia). Gabapentin and pregabalin are widely prescribed as part of the routine approach to palliating neuropathic pain. Although they are often viewed as interchangeable agents, very little comparative data of their benefits and harms exists in clinical practice. The aggregation of gabapentin having a doubtful, possible or probable contribution to serious event development averaged 5.2% over the study period which accords well with the 7% for severe AEs reported in a similar pharmacovigilance study in an unselected adult hospice/palliative care population prescribed gabapentin for neuropathic pain. 10 Patients suitable for gabapentin should have a clear neuropathic pain syndrome, characterized by sharp, shooting, lancinating and/or burning pain, in a nerve root (radicular) or stocking/glove distribution. Adult dosing: Gabapentin is started at low doses (100 mg to 300 mg total daily) and increased by 100 – 300 mg every 1-3 days to effect. Gabapentin, a γ-amino butyric acid analogue antiepileptic drug, is commonly prescribed for neuropathic pain in hospice/palliative care. Most of the evidence however relates to Am Fam Physician. 2014;90(1):26-32 Related editorial: Beyond Analgesia in Palliative Care and End-of-Life Interventions Patient information: See related handout on managing pain at the end-of-life
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 | |
 |  |
 |  |