Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 | %20for%20Post-operative%20Pain.png?md=1) |
 |  |
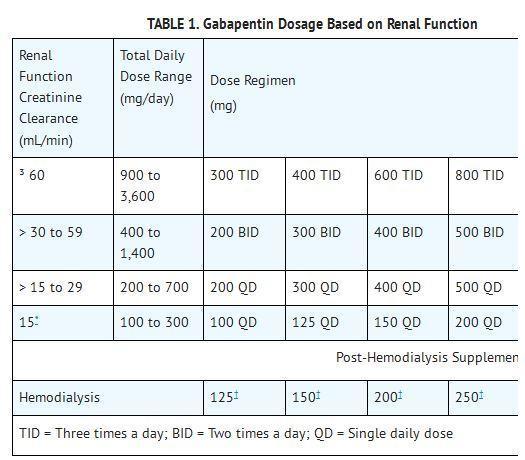
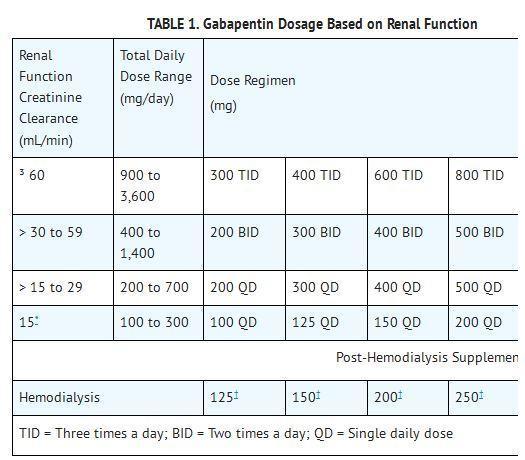
Background Gabapentin is an antiepileptic drug used in a variety of chronic pain conditions. Increasing numbers of randomized trials indicate that gabapentin is effective as a postoperative analgesic. This procedure-specific systematic review aims to analyse the 24-hour postoperative effect of gabapentin on acute pain in adults. Methods Medline, The Cochrane Library and Google Scholar were Gabapentin, an anticonvulsant, has recently been suggested as an effective postoperative ‘analgesic’ agent. The objective of the present study was to examine the analgesic effectiveness, opioid-sparing effects and side effects associated with the use of gabapentin in a perioperative setting. For example, in this study, 5 80% of gabapentin users received gabapentin on the day of surgery, suggesting that it was started prior to any patient report of pain, representing an opportunity to de-escalate gabapentin use for some patients. Second, engaging patients and caregivers in their care could allow us to better manage expectations for In summary, the administration of gabapentin was effective in decreasing postoperative narcotic consumption and the incidence of pruritus. There was a high risk of selection bias and a higher heterogeneity of knee flexion range in this analysis. Gabapentin is a novel drug used for the treatment of postoperative pain with antihyperalgesic properties and a unique mechanism of action, which differentiates it from other commonly used drugs. Various studies have shown that perioperative use of gabapentin reduces postoperative pain. 300 mg on day 1, 600 mg on day 2, and 900 mg from day 3 to day 30 after surgery: Acute post-operative pain intensity in gabapentin group was significantly lower than the placebo group p<0.05). The rate of PLP at the last follow-up was lower in the gabapentin group (43.48%) compared to placebo (77.27%, p=0.033). Hah et al., 2018 25 Gabapentin appears safe and well tolerated when used for persistent post-operative and post-traumatic pain in thoracic surgery patients, although minor side effects do occur. Gabapentin may relieve refractory chest wall pain in some of these patients, particularly those with more severe pain. But gabapentinoids also have risks and there is little evidence to support their use for postoperative pain relief, according to a large new study by a team of Canadian researchers. “No clinically significant analgesic effect for the perioperative use of gabapentinoids was observed. The shift towards multimodal pain regimens, including gabapentin, has taken place without attention to ensuring that they, like opioids, are appropriately discontinued soon after surgery. The prevalence of prolonged use of post-operative gabapentin among older adults is unknown, as are the factors associated with prolonged use. Background: Perioperative pain treatment often consist of combinations of non-opioid and opioid analgesics, 'multimodal analgesia', in which gabapentin is currently used. The aim was to document beneficial and harmful effects of perioperative gabapentin treatment. The efficacy of preoperative gabapentin in spinal surgery: a meta-analysis of randomized controlled trials. Pain Phys. 2017; 20(7):649-661. Medline, Google Scholar; 17. . Gabapentin for post-operative pain management—a systematic review with meta-analyses and trial sequential analyses. Gabapentin 250 mg is statistically superior to placebo in the treatment of established acute postoperative pain, but the NNT of 11 for at least 50% pain relief over 6 hours with gabapentin 250 mg is of limited clinical value and inferior to commonly used analgesics. Gabapentin (NeurontinTM) has gained significant interest as part of a multi-modal pain management strategy for the control of acute pain. There has been considerable variation in both the dose and the regimen used in recent clinical trials. The purpose of this review is to critically appraise the evidence for the use of gabapentinoids for acute pain management and its impact on the development of chronic pain after surgery. Recent findings: Recent meta-analyses have revealed that prior data likely have overestimated the beneficial effects of gabapentinoids in acute perioperative Perioperative gabapentin, 1200 mg, administered preoperatively plus 600 mg every 8 hours continued for 72 hours after surgery did not affect time to pain cessation, the rate of pain resolution, or the proportion of patients with chronic pain at 6 months or 1 year following surgery. Yu L, Ran B, Li M, Shi Z. Gabapentin and pregabalin in the management of postoperative pain after lumbar spinal surgery: a systematic review and meta-analysis. Spine. 2013;38(22):1947–52. doi: 10.1097/BRS.0b013e3182a69b90. Multi-modal approaches to managing post-operative pain after spinal surgery that include behavioral interventions have shown great promise in helping to ameliorate postoperative pain and the transition to chronic postsurgical pain. Questions remain in defining the timing, duration, and efficacy of these interventions. In 2006, Sihoe et al. evaluated gabapentin in the treatment of chronic pain after chest surgery (6). Twelve patients were chest trauma victims, 22 were status post video assisted thoracoscopic surgery (VATS), 8 had undergone open thoracotomies, and 3 had median sternotomies. Patients were started on a dose of gabapentin 300 mg daily some outcomes indirectness. Firm evidence for use of gabapentin is lacking as clinically relevant beneficial effect of gabapentin may be absent and harm is imminent, especially when added to multi-modal analgesia. Editorial Comment In this trustworthy systematic review, use of gabapentin for post-operative pain management was scrutinized. Randomised placebo-controlled trials (RCTs) investigating peri-operative gabapentin for post-operative pain management were eligible for inclusion. Eligible outcomes were relevant pain outcomes such as pain scores, time to first analgesic request and post-operative cumulative opioid consumption.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 | %20for%20Post-operative%20Pain.png?md=1) |
 |  |