Gallery
Photos from events, contest for the best costume, videos from master classes.
/GettyImages-538882863-e51a40e5b8da40ce82e98e79576e7230.jpg) |  |
 |  |
 |  |
 |  |
 |  |
 | 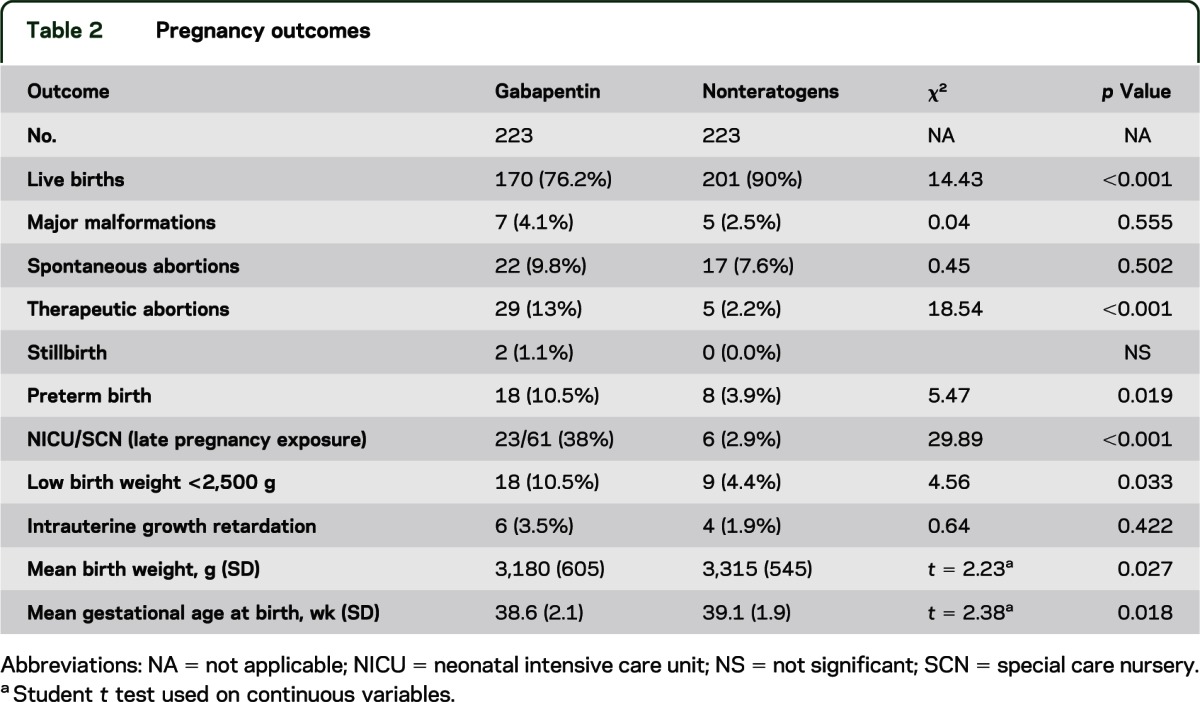 |
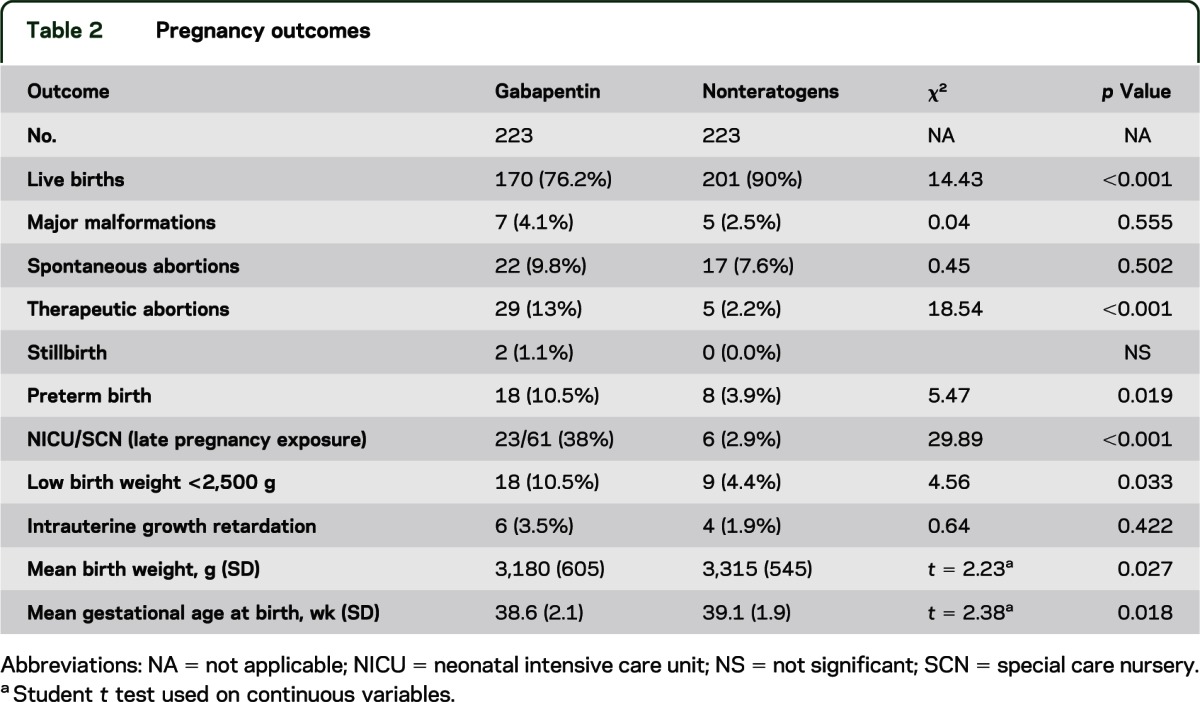
We examined the risk of major congenital malformations and cardiac defects associated with gabapentin exposure during the first trimester (T1), and the risk of preeclampsia (PE), preterm birth In our study, only 28% of the women continued taking gabapentin throughout pregnancy as two-thirds of the women (66%) discontinued in the first trimester, most following pregnancy confirmation between 6 and 8 weeks’ gestation. There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to antiepileptic drugs (AEDs), such as gabapentin, during pregnancy. Encourage women who are taking gabapentin during pregnancy to enroll in the North American Antiepileptic Drug (NAAED) Pregnancy Registry by calling the toll free number 1-888-233-2334 or Ideally you'll take high dose folic acid for 3 months before you start trying to get pregnant and for the first 12 weeks of pregnancy. Do not worry if you have not taken it before you get pregnant, but start taking it as soon as possible once you know that you are pregnant. It helps your baby to grow normally. Pregnancy-related problems, such as preterm delivery (birth before week 37) or low birth weight (weighing less than 5 pounds, 8 ounces [2500 grams] at birth) have been reported in some studies looking at the use of gabapentin during pregnancy. We examined the risk of major congenital malformations and cardiac defects associated with gabapentin exposure during the first trimester (T1), and the risk of preeclampsia (PE), preterm birth (PTB), small for gestational age (SGA), and neonatal intensive care unit admission (NICUa) associated with gabapentin exposure early, late, or both early Does taking gabapentin in pregnancy increase the chance of other pregnancy-related problems? Pregnancy-related problems, such as preterm delivery (birth before week 37) or low birth weight (weighing less than 5 pounds, 8 ounces [2500 grams] at birth) have been reported in some studies looking at the use of gabapentin during pregnancy. pattern of birth defects associated with the use of gabapentin in pregnancy. One study looked at the pregnancy outcomes of women who received prescriptions for gabapentin. When looking at the outcomes of all the study participants, gabapentin exposure during early pregnancy does not appear to increase There was an increased risk of preterm birth among women exposed to gabapentin either late (RR=1.28 [CI 1.08-1.52], p < 0.01) or both early and late in pregnancy (RR=1.22 [1.09-1.36], p < 0.001). Gabapentin use in pregnancy is not very well-studied. While the available information does not strongly suggest that it causes problems for the baby, further research is required to prove that gabapentin is safe. In a large population-based study, we evaluated neonatal and maternal outcomes in over 4,000 women exposed to gabapentin early in pregnancy and approximately 2,000 women exposed in late pregnancy. Topiramate use early in pregnancy and the risk of oral clefts, A pregnancy cohort study. Neurology. 2018;90:e342-e351. results from the Gabapentin Pregnancy Registry. Epilepsy Behav. 2003 Jun gabapentin early in pregnancy appears to rule out large increases in risk, although available studies included small numbers of gabapentin-exposed pregnancies and therefore were not well powered to identify potential smaller teratogenic effects [4–11]. With maternal doses up to 2.1 g/day, estimated doses for fully breastfed infants are 0.2 to 1.3 mg/kg/day (equivalent to 1.3 to 3.8% of the maternal weight-adjusted dose). An expert panel has deemed this drug is an acceptable choice for refractory restless leg syndrome during lactation. The American College of Obstetricians and Gynecologists (ACOG) has released guidelines on psychiatric medication used by women during pregnancy and lactation. The use of psychotropic medications Early intervention and treatment of these patients may prevent progression to hyperemesis gravidarum, which, although rare, may require enteral or parenteral nutrition, a trial of psychiatric medications if the patient has psychiatric comorbidities, or corticosteroids or gabapentin in refractory cases . Five studies reported significant findings with increased risks of overall congenital anomalies, specific anomalies (nervous system, eyes, oro-facial clefs, urinary and genital system), miscarriage, stillbirth and specific neurodevelopmental outcomes after exposure to pregabalin during pregnancy. Antiepileptic drug: Safety in pregnancy: Efficacy in neuropathic pain: Gabapentin: Major congenital malformations: 1.47%* (95% CI 0.26-3.64) Based on data from three studies (n=190) There was a higher risk of preterm birth among women exposed to gabapentin either late (RR, 1.28 [1.08–1.52], p < 0.01) or both early and late in pregnancy (RR, 1.22 [1.09–1.36], p < 0.001), SGA among women exposed to gabapentin early (1.17 [1.02–1.33], p = 0.02), late (1.39 [1.01–1.91], p = 0.05), or both early and late in pregnancy Selected References: Blotiere PO, et al. 2020. Risk of early neurodevelopmental outcomes associated with prenatal exposure to the antiepileptic drugs most commonly used during pregnancy: a French nationwide population-based cohort study. BMJ Open 10(6). Brannon GE, Rolland PD. Anorgasmia in a patient with bipolar disorder type 1 treated with gabapentin. J Clin Psychopharmacol. 2000;20(3):379
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
/GettyImages-538882863-e51a40e5b8da40ce82e98e79576e7230.jpg) |  |
 |  |
 |  |
 |  |
 |  |
 |  |