Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
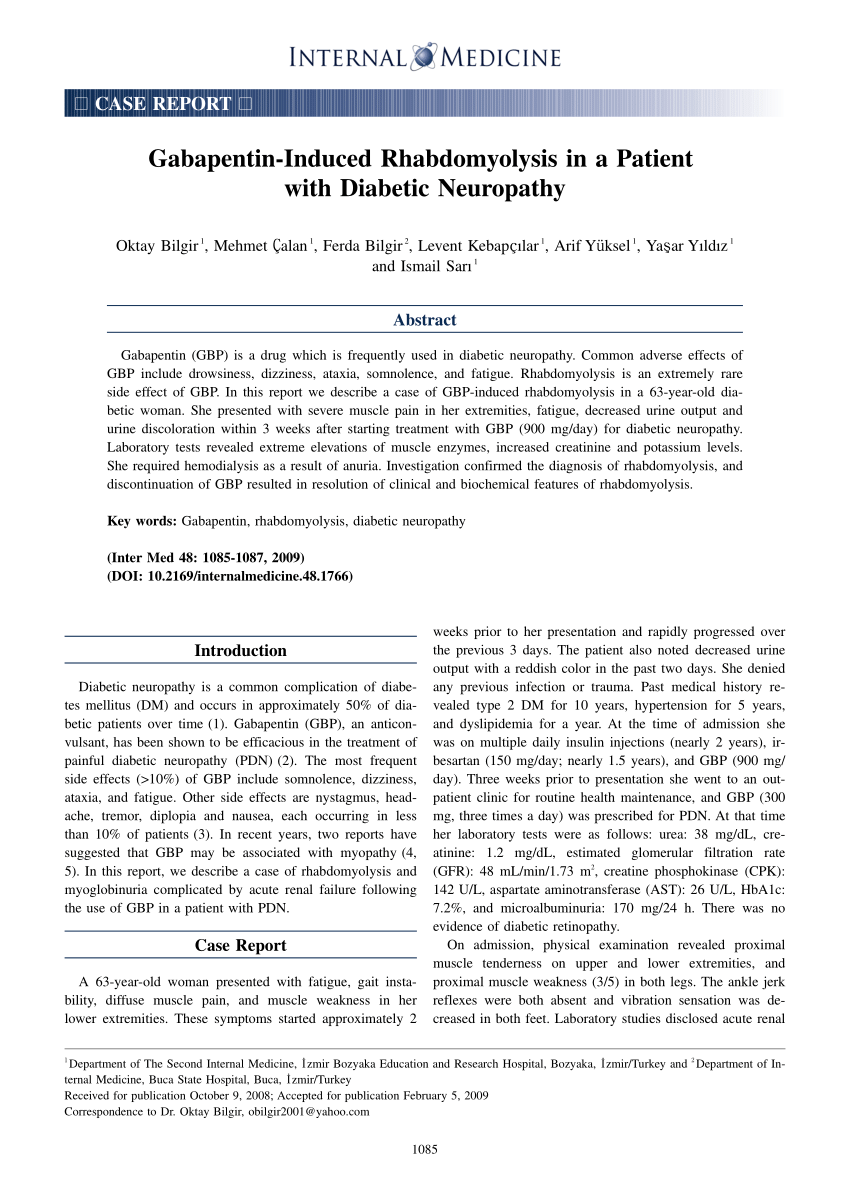
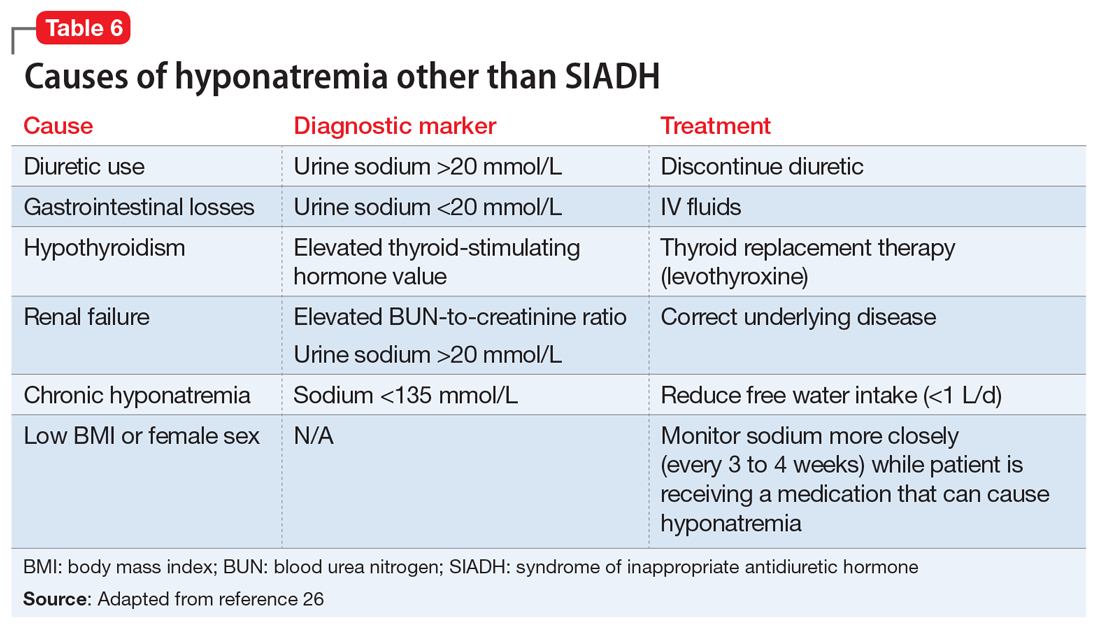
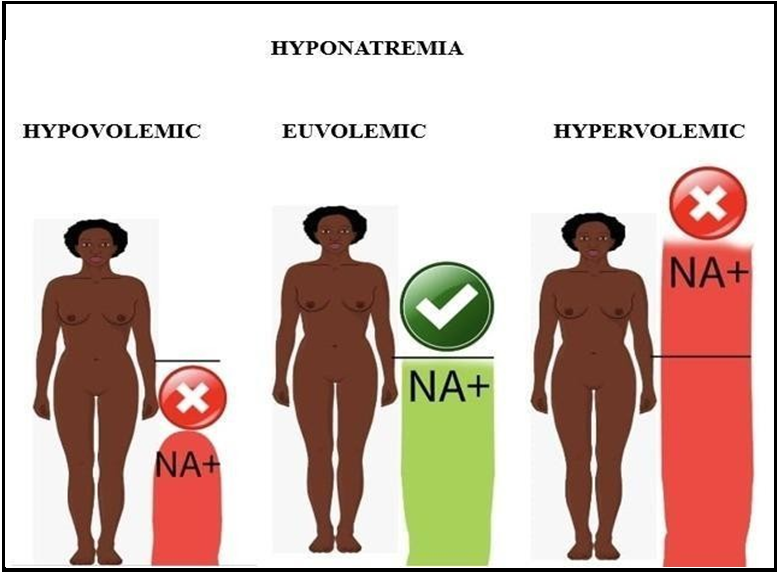
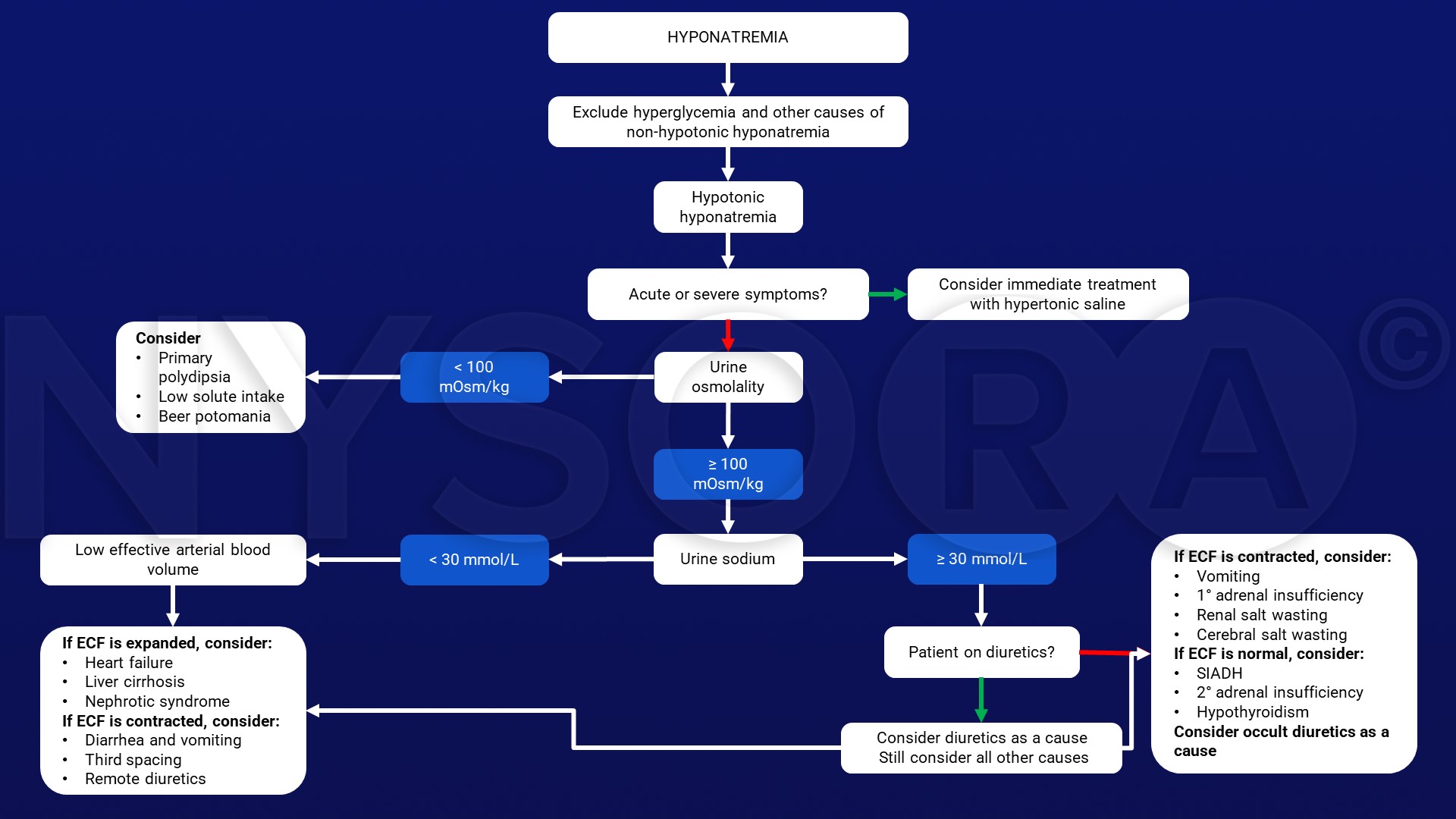
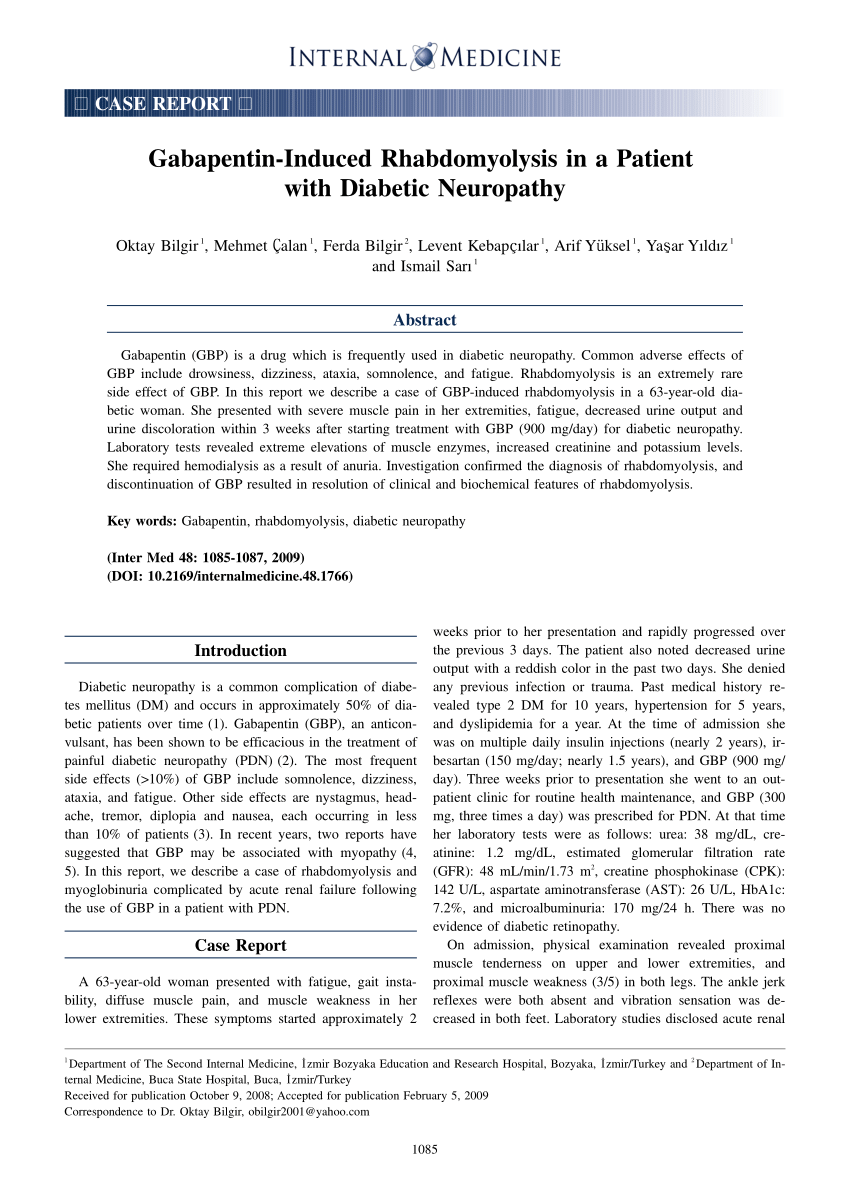
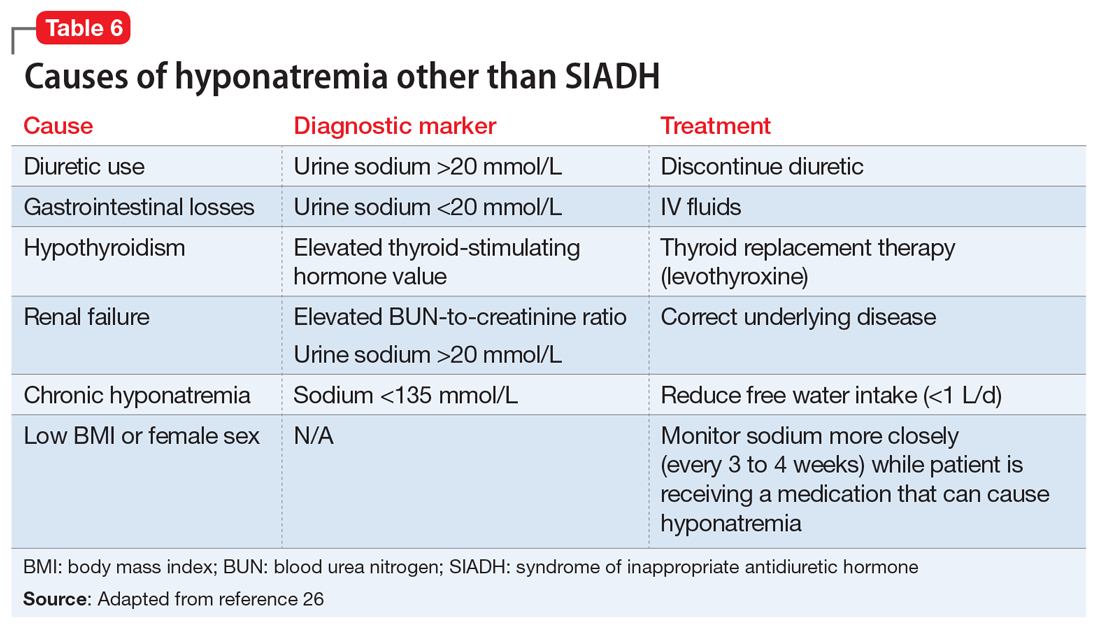
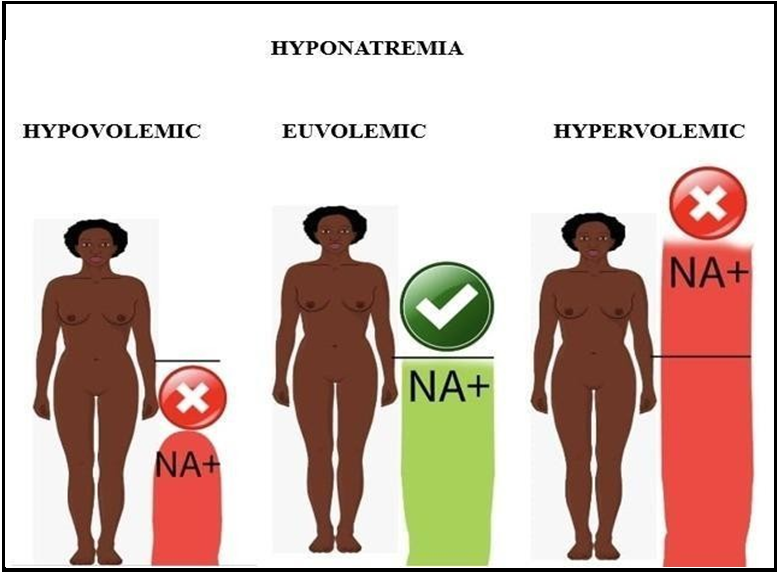
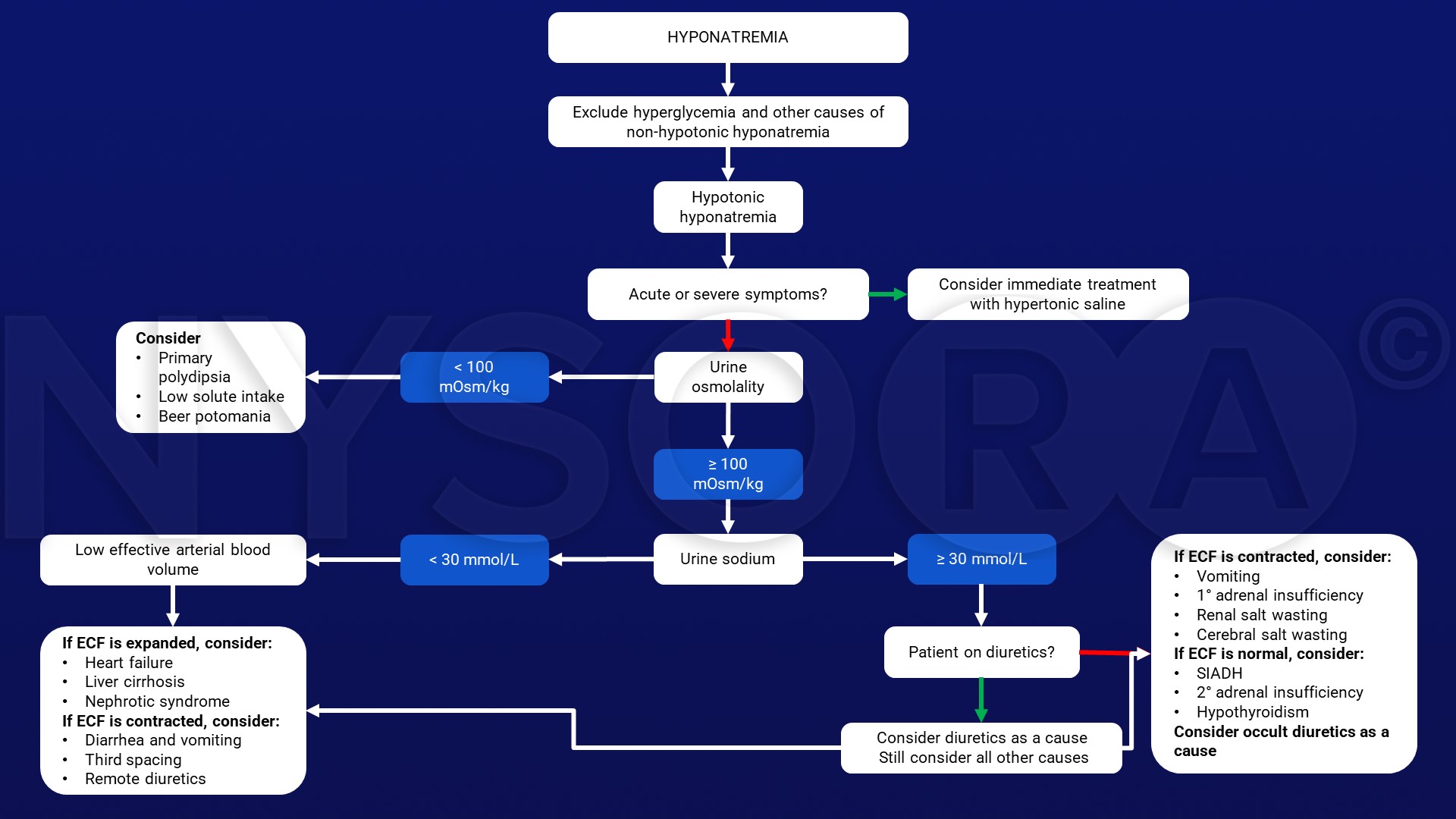
Signs of Gabapentin-Induced Hyponatremia. Gabapentin-induced hyponatremia is a serious condition that can have potentially dangerous consequences if left untreated. It is essential to recognize the signs and symptoms of this condition to ensure prompt medical intervention. Some common signs of gabapentin-induced hyponatremia include: 1. Expert opinion: Carbamazepine and oxcarbazepine are the most common AEDs which induce hyponatremia in patients with epilepsy. Recently, other AEDs, such as eslicarbazepine, sodium valproate, lamotrigine, levetiracetam and gabapentin have also been reported to cause hyponatremia. Carbamazepine and oxcarbazepine are the anticonvulsants most commonly reported to be associated with hyponatremia in patients with epilepsy, although other anticonvulsants, such as eslicarbazepine, sodium valproate, lamotrigine, levetiracetam, and gabapentin, have also been reported to cause hyponatremia . The most frequent electrolyte disorder in hospitalized patients is hyponatremia [1]. The clinical spectrum in hyponatremia ranges from mild, non-specific symptoms such as fatigue, headache, and gait instability to life-threatening symptoms such as seizures, coma and ultimately death, secondary to brain oedema [2,3]. Pharmaceutical drugs, e.g., thiazide diuretics, antidepressants and Hyponatremia (defined as a serum sodium level < 134 mmol/L) is the most common electrolyte abnormality in hospitalized patients. Certain drugs (eg, diuretics, antidepressants, and antiepileptics) have been implicated as established causes of either asymptomatic or symptomatic hyponatremia. Howeve Lamotrigine and gabapentin had the lowest risk both during initiation and ongoing treatment and may be advantageous in patients at risk of developing hyponatremia. Keywords: Adverse effect; Antiepileptic drugs; Hyponatremia; SIADH. Both oxcarbazepine- and eslicarbazepine acetate-induced hyponatremia occurred particularly in elderly epilepsy patients. Recent evidence suggests that eslicarbazepine acetate (ESL) might be an appropriate alternative to carbamazepine (CBZ) and oxcarbazepine (OXC) due to its better safety profile. Although gabapentin is generally well tolerated, 1 potential reported adverse effect is peripheral edema. However, due to the extensive number of etiologies of peripheral edema, medication causes may be overlooked on an inpatient psychiatric unit. According to a population-based case-control study, use of CBZ, phenytoin (PHT), VPA, LTG, LEV, or gabapentin increases the risk of hospitalization for hyponatremia [17]. However, this study was based on a national hospitalization database, which means the patients showed an age bias (mean age: 74 years) and the influence of dosage was not with diuretic-induced hyponatremia and an SIADH-like profile, unless there is strong evi-dence to suggest an underlying cause for SIADH, a comprehensive diagnostic evalua-tion should be postponed for 2 to 3 weeks. However, taking into consideration that thia-zides may aggravate the hyponatremia induced by SIADH, an evaluation is a prudent ap- The reported incidence of carbamazepine-induced hyponatremia ranges widely from <1% to 40%. 9 Several small clinical studies have noted decreases in the concentration of serum sodium following carbamazepine use, but most were uncontrolled and none quantified the magnitude of risk. 10-17 Hyponatremia with valproic acid was identified in a single However, many drugs were not included in the investigators' list of medications that cause hyponatremia. Nicotine patch therapy can induce hyponatremia. The proposed mechanism is a possible syndrome of inappropriate antidiuretic hormone (SIADH) induced by this drug. Hyponatremia is reported as a side effect among people who take Gabapentin (gabapentin), especially for people who are male, 60+ old, have been taking the drug for < 1 month also take Ondansetron, and have Stress and anxiety. Here we report a patient with pregabalin-induced hyponatremia who met the criteria for SIADH; after discontinuation of the drug, his condition rapidly improved. This case can help clinicians diagnose and treat new-onset hyponatremia in patients who recently initiated pregabalin therapy. Hyponatremia (defined as a serum sodium level < 134 mmol/L) is the most common electrolyte abnormality in hospitalized patients. Certain drugs (eg, diuretics, antidepressants, and antiepileptics) have been implicated as established causes of either asymptomatic or symptomatic hyponatremia. Of the five previously published cases with levetiracepam-induced hyponatremia [7], [21], [22], [23], four had a predisposition to SIADH. Whether a peripheral process (such as a direct effect on renal tubules), as discussed above, could be a contributing factor to levetiracepam-induced hyponatremia remains speculative. Gabapentin and pregabalin are less likely to cause hyponatremia, although a few isolated cases have been reported. The association between CBZ, OXC, and hyponatremia dates back to the 1970s and 1980s, with varying reported incidences across different studies [ 17 , 18 ]. Learning how gabapentin can cause hyponatremia is key. Hearing from those who have been affected gives us deep insights. Their stories help others understand what they might face. Drug-induced hyponatremia caused by renal water retention is mainly due to syndrome of inappropriate antidiuresis (SIAD). SIAD can be grouped into syndrome of inappropriate antidiuretic hormone secretion (SIADH) and nephrogenic syndrome of inappropriate antidiuresis (NSIAD). The former is characterized by uncontrolled hypersecretion of arginine vasopressin (AVP), and the latter is produced by Recently, other AEDs, such as eslicarbazepine, sodium valproate, lamotrigine, levetiracetam and gabapentin have also been reported to cause hyponatremia. Understanding the risk associated with AED-induced hyponatremia and taking effective measures to combat serum sodium imbalance induced by AED therapy are necessary.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |