Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
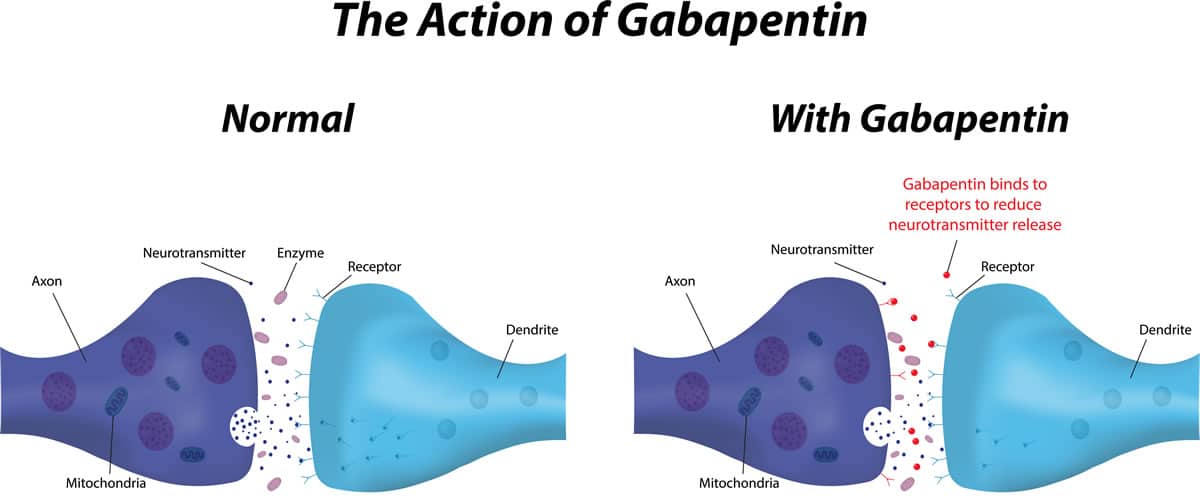 |  |
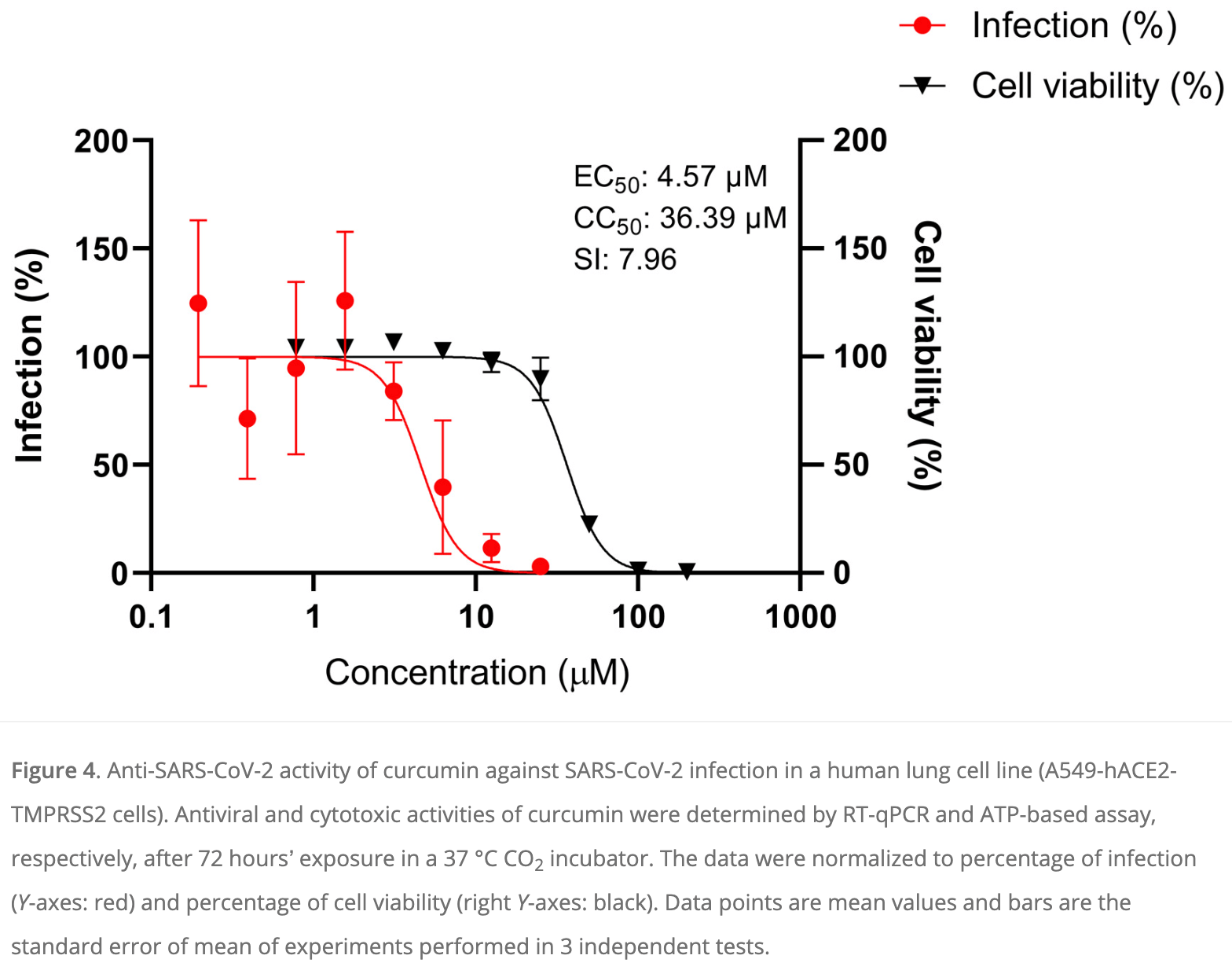
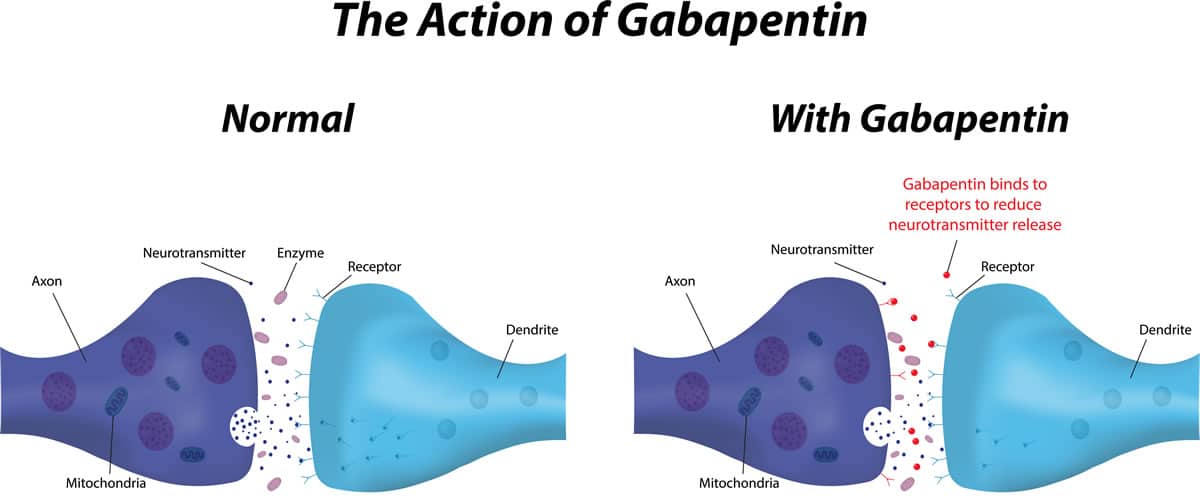
Gabapentinoids are opioid substitutes whose elimination by the kidneys is reduced as kidney function declines. To inform their safe prescribing in older adults with chronic kidney disease (CKD), we examined the 30-day risk of serious adverse events according to the prescribed starting dose. As a result, metabolism-related factors do not necessitate dosage alterations of gabapentin and concomitant AEDs after prolonged therapy. The drug is excreted unchanged in urine; plasma clearance is linearly related to creatinine clearance; and dosage is readily adjusted based on renal function. Absorption of gabapentin is solely dependent on LAT that are easily saturable, resulting in dose-dependent pharmacokinetics. As the dose of gabapentin increases, the area under the plasma concentration–time curve (AUC) does not increase proportionally. Gabapentin CL/F and CLR were linearly correlated with creatinine clearance. Total urinary recovery of unchanged drug was comparable in all subjects, indicating that the extent of drug absorption was unaffected by renal function. There was no evidence of gabapentin metabolism even in subjects with severe renal impairment. In summary, impaired Gabapentin has a favorable pharmacokinetic profile, because it is not protein-bound or metabolized and has no known drug–drug interactions. 10 Gabapentin has been widely used in elderly patients with multiple comorbidities, including chronic kidney disease. However, gabapentin is eliminated solely through the kidney, and kidney impairment Gabapentin is an anticonvulsive medication that received approval from the US Food and Drug Administration (FDA) in 1993 and has been available in generic form in the USA since 2004. Gabapentin was originally used as a muscle relaxant and an anti-spasmodic. However, it was later discovered that gabapentin has the potential of an anticonvulsive medication and can be used as an adjunct to more Unlike other drugs, gabapentin is not metabolized in the liver and is solely excreted by the kidneys. Therefore, it is crucial to adjust the dosage in patients with renal insufficiency to avoid severe adverse effects. Patients with chronic kidney disease often receive inappropriately high gabapentin dosage for their kidney function, occasioning overt toxicity; advanced age and comorbidity predispose these patients for toxicity. Gabapentin (Neurontin) usually isn’t bad for your liver or kidneys. In most cases, it has little effect on these organs. In rare instances, gabapentin can cause DRESS (drug reaction with eosinophilia and systemic symptoms) syndrome. CKD alters renal drug elimination by affecting glomerular blood flow, filtration rate, tubular secretion and reabsorption, and renal bioactivation and metabolism. 18 Additionally, pharmacokinetic handling of medications (absorption, distribution, metabolism, and elimination) may be affected. 19 Reducing the dose is recommended for medications Gabapentin enacarbil is converted to gabapentin during absorption, before reaching the systemic circulation. 16 Gabapentin produced by hydrolysis of gabapentin enacarbil is also eliminated by the renal clearance pathway, without further metabolism.16, 17 In patients with normal CrCL (≥60 mL/min), CL R after oral administration of gabapentin Gabapentin is almost exclusively cleared by the kidney and thus presents challenges in patients with kidney failure. Gabapentin is known to be effectively cleared by hemodialysis, but the efficiency of clearance by peritoneal dialysis (PD) has not been previously described. We report a case of gabapentin toxicity in a patient Gabapentin’s apparent total clearance is 100 mL/min in adults with normal renal function, which is essentially equivalent to CrCl and does not suggest the involvement of tubular reabsorption. 1 Some evidence suggest that active tubular secretion mediated by organic cation transporter-1 (OCT-1) may play a role in gabapentin’s renal clearance. Unlike many drugs metabolized by the liver, gabapentin’s primary pathway out of the body is through the kidneys. In healthy individuals, the kidneys efficiently filter gabapentin from the blood, ensuring the medication is removed as waste in urine. It is entirely excreted through the renal system so this needs to be considered in any patient becoming acutely ill and developing renal failure. We describe a patient who developed significant deterioration in her conscious level due to iatrogenic gabapentin overdose. Gabapentin is cleared via renal excretion, and its elimination is proportional to creatinine clearance (CrCL); CrCL can, therefore, be used as a predictor of gabapentin renal clearance. Gabapentin produced from hydrolysis of gabapentin enacarbil is also eliminated via the renal clearance pathway. Gabapentin for dogs is commonly prescribed for pain, anxiety, or seizures. It's generally safe, but there are some known side effects to be aware of. Metabolism and Renal Excretion. Gabapentin is not metabolized in humans and is excreted primarily as unchanged drug in the urine. Renal clearance is linearly related to creatinine clearance in both pediatric and adult populations. Therefore, dosage reductions based on declining renal function are recommended (Table 268-1). Gabapentin is a unique anticonvulsant that is used as adjunctive therapy in management of epilepsy and for neuropathic pain syndromes. Therapy with gabapentin is not associated with serum aminotransferase elevations, but several cases of clinically apparent liver injury from gabapentin have been reported. The risks are not directly kidney damage from gabapentin, but that reduced kidney function affects its metabolism and can lead to adverse effects. Working closely with your veterinarian to determine the appropriate dosage, closely monitoring your cat’s response, and regular blood work to evaluate kidney function is vital.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |