Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 | |
 |  |
 | 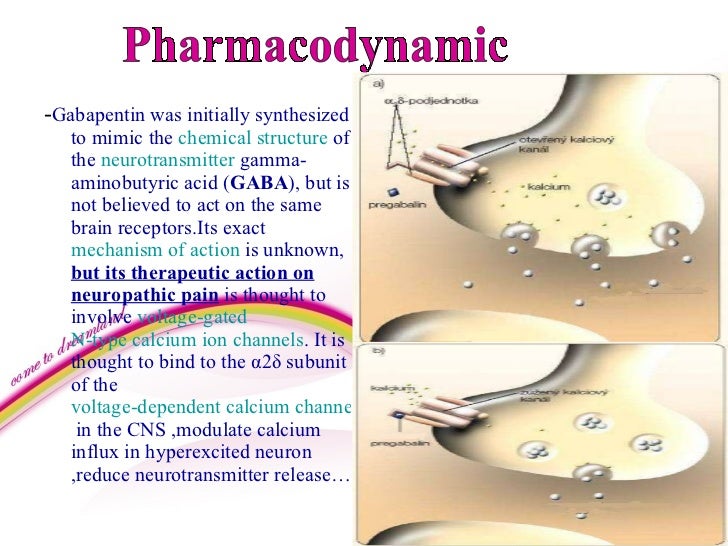 |
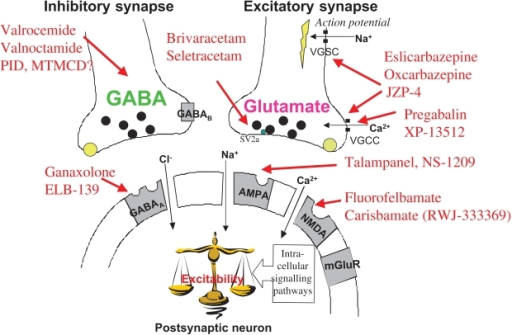
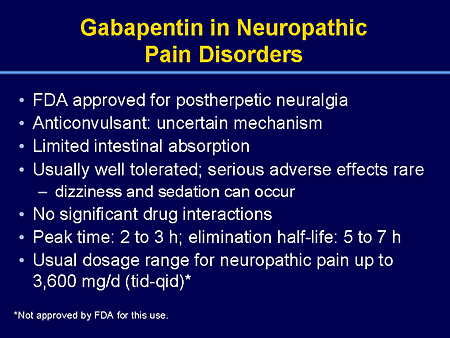
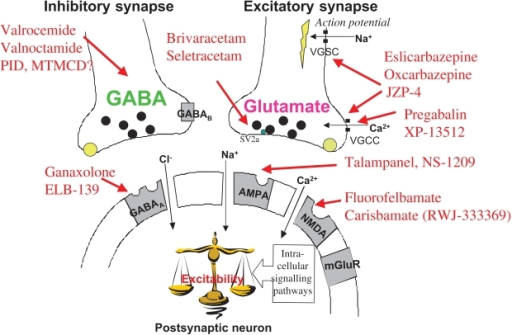
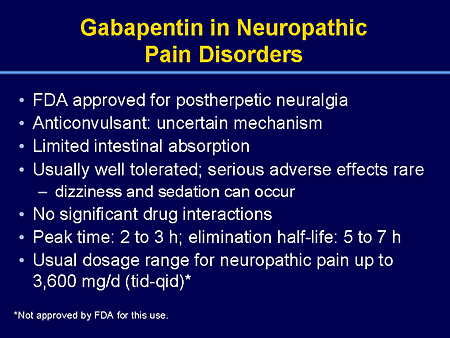
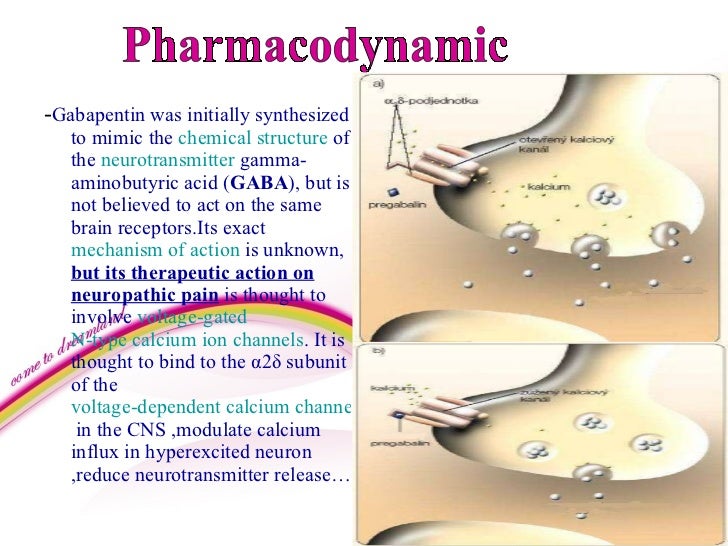
Gabapentin has become popular as a first-line treatment for neuropathic pain because of its efficacy as an antineuropathic agent and relatively benign side-effect profile. However, its mechanism of action is far from clear. Gabapentinoids, including gabapentin and pregabalin, are extensively used for treatment of neuropathic pain, restless legs syndrome, and focal seizures. Their efficacy in these disorders is primarily attributed to their effects in inhibiting the functions of the α2δ subunit of presynaptic VGCCs, thereby reducing neurotransmitter release. The gabapentinoids are often recommended as first-line treatments for the management of neuropathic pain. The differing pharmacodynamic and pharmacokinetic profiles can have implications for clinical practice. This article has summarised these key Gabapentin (GBP) is a Health Canada approved antiepileptic drug. 5 In the UK, GBP is licensed for the treatment of peripheral and central neuropathic pain in adults and in the US it is marketed for post-herpetic neuralgia (PHN). 3 The mechanism of action for GBP relates to its ability to bind with high-affinity to the alpha-2-delta subunit of vo A recent study has shown the effectiveness of gabapentin (5 or 50 mg/kg, i.p.) in attenuating neuropathic pain behavior in forelimb neuropathic pain model (due to partial injury to medial and ulner nerves) in a dose-dependent manner (Yi et al. 2011). Generic Name Gabapentin DrugBank Accession Number DB00996 Background. Gabapentin is a structural analogue of the inhibitory neurotransmitter gamma-aminobutyric acid that was first approved for use in the United States in 1993. 16 It was originally developed as a novel anti-epileptic for the treatment of certain types of seizures 14,5 - today it is also widely used to treat neuropathic pain. 8 N.B. Indication = peripheral neuropathic pain: 1–4 patches to the painful area for 30–60 min every 3 months: WEAK: Moderate–high N.B. Potential safety concerns over sensation with long–term use: Moderate–high: Lidocaine plasters N.B. Indication = peripheral neuropathic pain: 1–3 5% plasters to region of pain one per day for up to 12 Gabapentin (GBP) is a 3,3-disubstituted derivative of gamma-aminobutyric acid (GABA). It is recommended as a first-line treatment for chronic neuropathic pain, particularly in diabetic neuropathy Its mechanisms of action appear to be a complex synergy between increased GABA synthesis, non-NMDA receptor antagonism and binding to the α, δ subunit of voltage dependent calcium channels. The latter action inhibits the release of excitatory neurotransmitters. Keywords: pregabalin, gabapentin, neuropathic pain, pain, meta-analysis, systematic review Citation: Mayoral V, Galvez R, Ferrándiz M, Miguéns Vázquez X, Cordero-García C, Alcántara Montero A, Pérez C and Pérez-Páramo M (2025) Pregabalin vs. gabapentin in the treatment of neuropathic pain: a comprehensive systematic review and meta 2d-1 can cause neuropathic pain even in the absence of nerve damage. Transgenic mice that overexpress a 2d-1 show symptoms of allodynia even when nerve damage is absent, which suggests that increased concentrations of a 2d-1 are sufficient to cause neuropathic pain.18 The frequency of miniature excitatory postsynaptic The injury can be induced by chronic nerve compression, either by partial sciatic nerve ligation, i.e. tight ligation of one-third to half of the sciatic nerve (Seltzer et al., 1990), spinal nerve ligation, i.e. tight ligation of L5 and L6 spinal nerves (Kim and Chung, 1992), chronic constriction injury, consisting in loosely constrictive Gabapentin has no direct GABAergic action and does not block GABA uptake or metabolism. Gabapentin blocks the tonic phase of nociception induced by formalin and carrageenan, and exerts a potent inhibitory effect in neuropathic pain models of mechanical hyperalgesia and mechanical/thermal allodynia. Gabapentin is an anti-epileptic agent but now it is also recommended as first line agent in neuropathic pain, particularly in diabetic neuropathy and post herpetic neuralgia. α2δ-1, an auxillary subunit of voltage gated calcium channels, has been documented as its main target and its specific binding to this subunit is described to produce Neuropathic pain. Gabapentin has proved to be efficacious in the treatment of neuropathic pain and is now approved for this indication in patients over 18 years of age. Evidence for its efficacy is discussed below. Dosage and administration. Oral doses of gabapentin are administered three times a day (tds) because of its short half-life. Originally designed as analogs of GABA, the gabapentinoids bind to the α 2 δ ‐1 and α 2 δ ‐2 auxiliary subunits of calcium channels, though only the former has been implicated in the development of neuropathy in animal models. Because spinal plasticity and sensitization have been intensely studied in neuropathic pain, most laboratory studies have focused on actions of gabapentinoids in the spinal cord, where they reduce primary afferent traffic and excitation of spinal nociceptive neurons, via interaction with α2δ subunits of voltage-gated Ca 2+ channels. The analgesic effect in neuropathic pain is well evidenced but the role in postoperative pain is less certain. Medline and EMBASE database searches were conducted to identify studies relating to mechanisms of action and effects in experimental animal models of inflammatory and postoperative pain and human models of experimental pain. Narrative: Neuropathic pain, when the pain generator is the nerve itself, occurs in a variety of conditions including diabetes mellitus and postherpetic neuropathy. The exact mechanism of action There is overlap between chronic and neuropathic pain: neuropathic pain is chronic but not all chronic pain is neuropathic. Most likely as a result of increased activity of the endogenous pro-nociceptive neuropeptide CCK, neuropathic pain does not respond well to opioids (Wiesenfeld-Hallin et al., 2002).
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 | |
 |  |
 |  |