Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
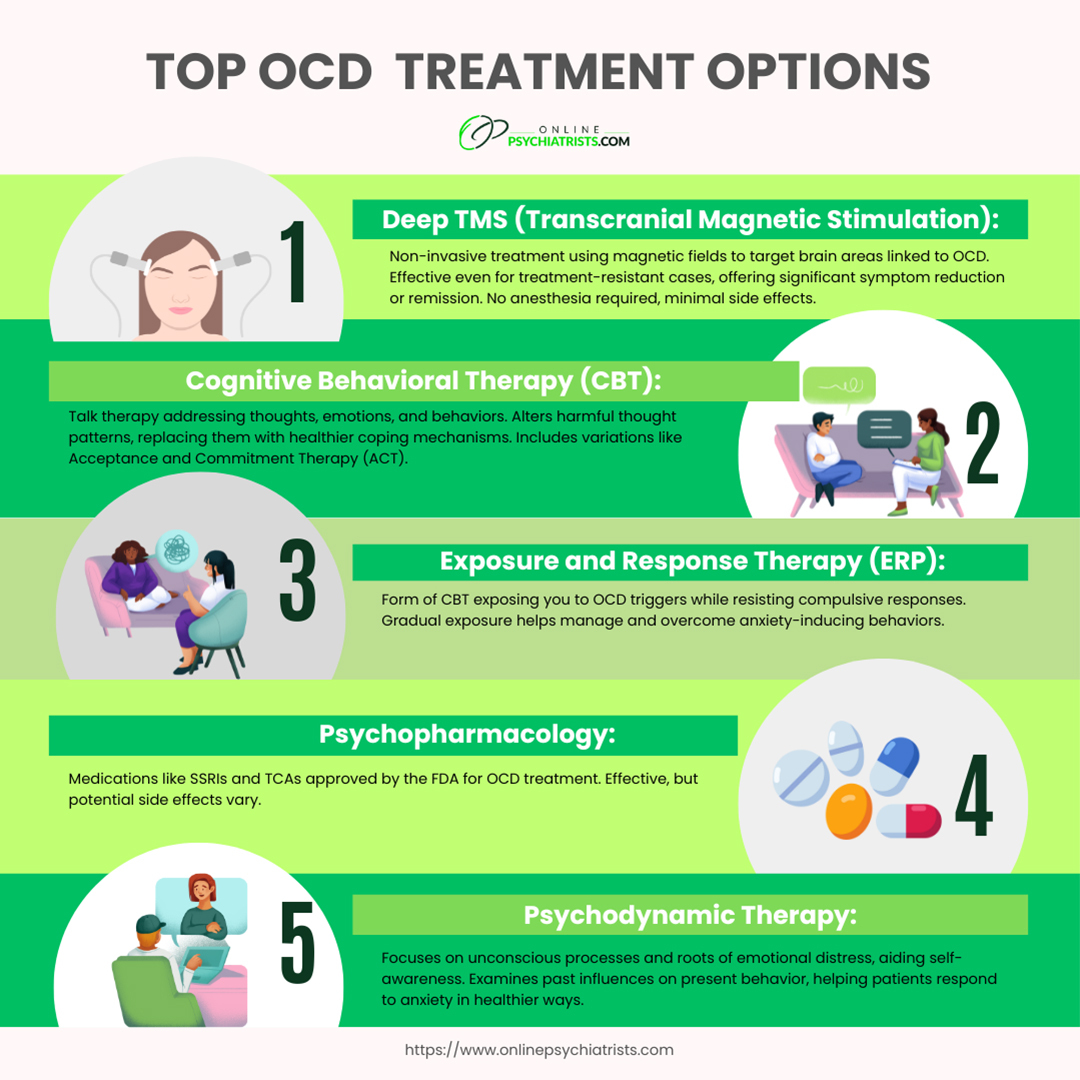
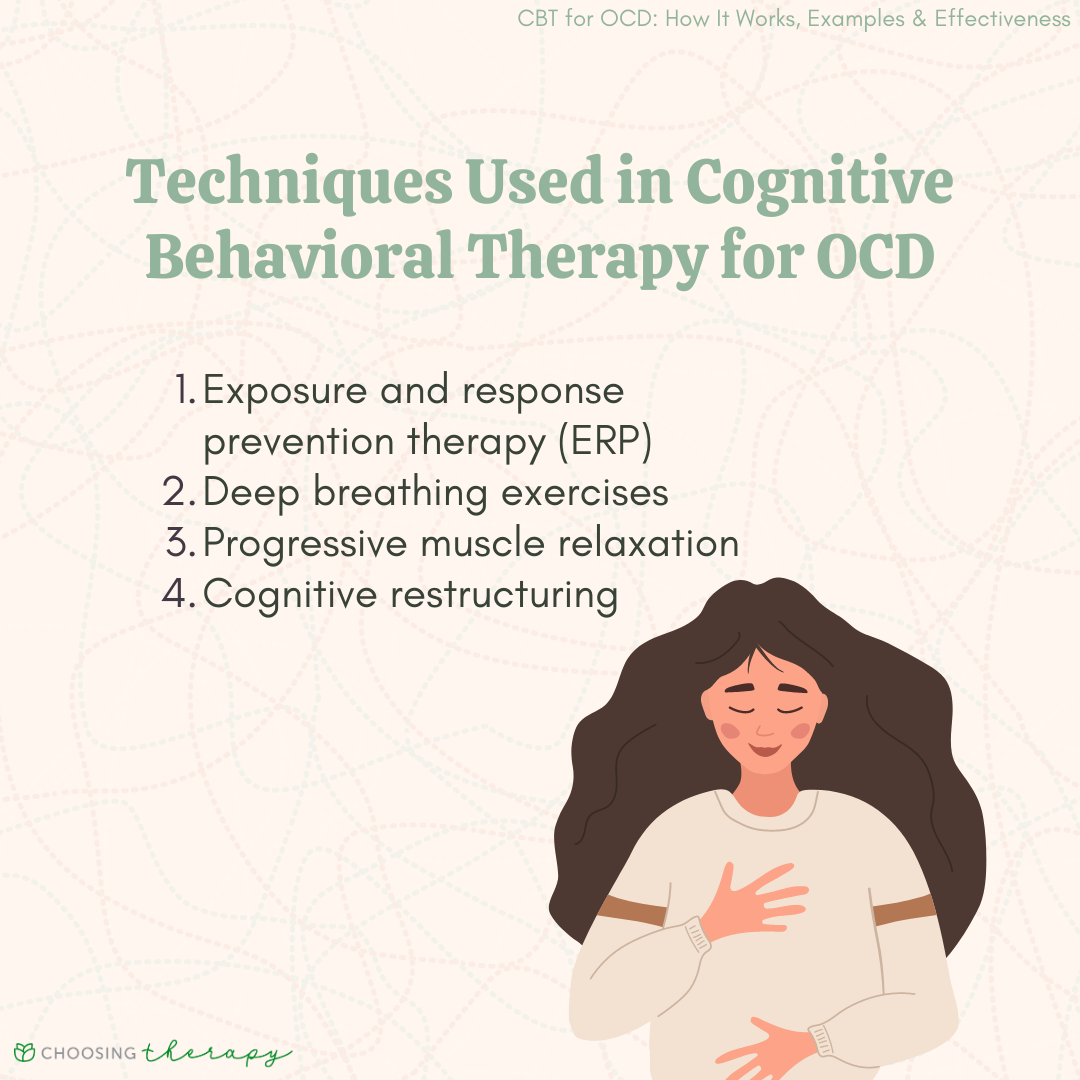
Gabapentin is not a typical medication for OCD, although it is often prescribed “off-label” if a medical provider deems it necessary. Thus, researchers have found that gabapentin can ease OCD symptoms in some people. The mechanism of action of the drugs effective in treating OCD (clomipramine, a non-selective serotonin reuptake inhibitor, and the selective serotonin reuptake inhibitors [SSRIs]: citalopram, fluoxetine, fluvoxamine, sertraline and paroxetine) has given rise to the hypothesis that deficient serotonin function is a key element in the pathophysiology of OCD. However, a post-hoc analysis found that patients with severe panic disorder who received gabapentin treatment showed a significant improvement in PAS scores (p=0.04), compared to the placebo group. 15 The authors could not find any RCTs assessing the efficacy of gabapentin in the treatment of posttraumatic stress disorder (PTSD). 5,6,16 In one Objective: The aim of this study was to compare efficacy of fluoxetine alone and co-administration of gabapentin and fluoxetine in patients with obsessive compulsive disorder (OCD). Methods: Forty outpatients with a DSM-IV diagnosis of OCD were randomized to open label treatment, 20 of whom were treated with fluoxetine alone and the remaining The present pattern of results suggests that glutamatergic medications such as gabapentin and memantine adjuvant to a standard treatment with an SSRI have no additional positive impact on patients with OCD, as measured with the Y-BOCS. Additionally, side-effects were reported. Future studies should The interaction between glutamatergic and GABAergic systems has been considered to improve the symptoms of OCD, and gabapentin has been shown to be efficient in reducing the symptoms of anxiety; therefore, we thought that gabapentin might be useful in the treatment of OCD as add-on medication. Gabapentin has clearer efficacy for alcohol craving and withdrawal symptoms and may have a role in adjunctive treatment of opioid dependence. There is no clear evidence for gabapentin therapy in depression, PTSD prevention, OCD, or other types of substance abuse. Objective: This article reviews evidence-based psychiatric uses of gabapentin, along with associated risks. Method of Research: An extensive literature review was conducted, primarily of articles searchable in PubMed, relating to psychiatric uses, safety, and adverse effects of gabapentin. Results: Evidence supports gabapentin as a treatment for alcohol withdrawal and alcohol use disorder OCD can't be cured, but it can be controlled with medication, therapy, and support. What you can control is your decision to get treatment. Some anticonvulsant drugs (such as gabapentin or When patients do not respond to or are cannot tolerate SSRIs, the evidence supports several next steps. Here, I briefly review options for pharmacological management of treatment-resistant OCD, summarizing the evidence supporting each. As we look to the future, the role of gabapentin in mental health treatment continues to evolve. Ongoing research is exploring its potential in treating other conditions, such as obsessive-compulsive disorder and eating disorders. It’s like we’re still uncovering new layers of this versatile medication. While gabapentin is not currently FDA-approved for the treatment of OCD, there is growing interest in its potential as an alternative or adjunctive therapy for this condition. Several studies have explored the use of gabapentin in OCD, with mixed but promising results. Depending on how serious your OCD is, you may need long-term, ongoing or more-intensive treatment. The two main treatments for OCD are psychotherapy and medicines. Psychotherapy also is known as talk therapy. Often, a mix of both treatments is most effective. A recent meta-analysis conducted on 21 RCTs , which included 1047 subjects with a severe anxiety disorder or OCD or PTSD randomized to receive DCS or placebo in addition to CBT, showed add-on DCS to correlate with symptom improvement only from pre-treatment to post-treatment, but not from pre-treatment to mid-treatment or from pre-treatment to OCD is a common and chronic anxiety disorder associated with considerable morbidity and socioeconomic burden. 3-6 Because many previous studies have demonstrated the clinical efficacy of selective serotonin reuptake inhibitors (SSRI) in treating OCD, 7 SSRI have been considered the first-line treatment for OCD. 8-10 However, approximately 40 However, a post-hoc analysis found that patients with severe panic disorder who received gabapentin treatment showed a significant improvement in PAS scores (p=0.04), compared to the placebo group. 15 The authors could not find any RCTs assessing the efficacy of gabapentin in the treatment of posttraumatic stress disorder (PTSD). 5, 6, 16 In In a small, randomized, controlled trial involving patients with obsessive-compulsive disorder (OCD), Gabapentin was added to their treatment regimen alongside Fluoxetine. The study found some promise in accelerating the treatment response. Another study focused on breast cancer survivors experiencing nonspecific anxiety symptoms. One study on 40 people showed that gabapentin enhanced the effectiveness of SSRIs at alleviating early OCD symptoms . Similarly, pregabalin enhanced the effectiveness of conventional OCD therapy and reduced the symptoms by 26% in a case series of 12 patients. Research on GABA levels in OCD patients has yielded intriguing results. Several studies using magnetic resonance spectroscopy (MRS) have found reduced GABA concentrations in specific brain regions of individuals with OCD compared to healthy controls. Obsessive-Compulsive Disorder. Only 1 study has evaluated gabapentin use for obsessive-compulsive disorder (OCD). Onder et al 68 studied fluoxetine monotherapy versus fluoxetine with adjunctive gabapentin in controlling OCD symptoms. Forty patients were randomized (open-label) to fluoxetine 20 mg/d or fluoxetine 20 mg/d with gabapentin 600 mg/d.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |