Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 | |
 |  |
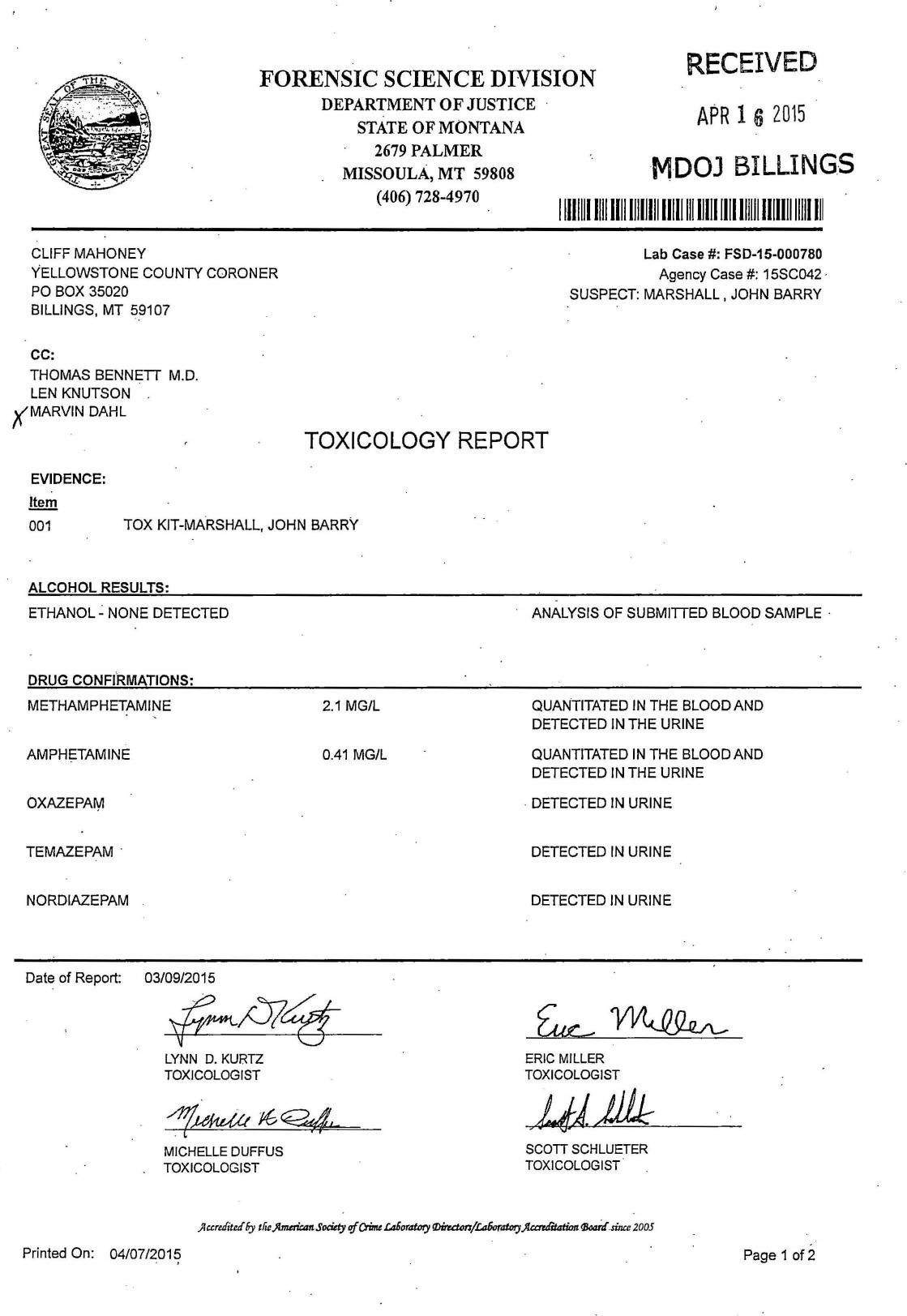
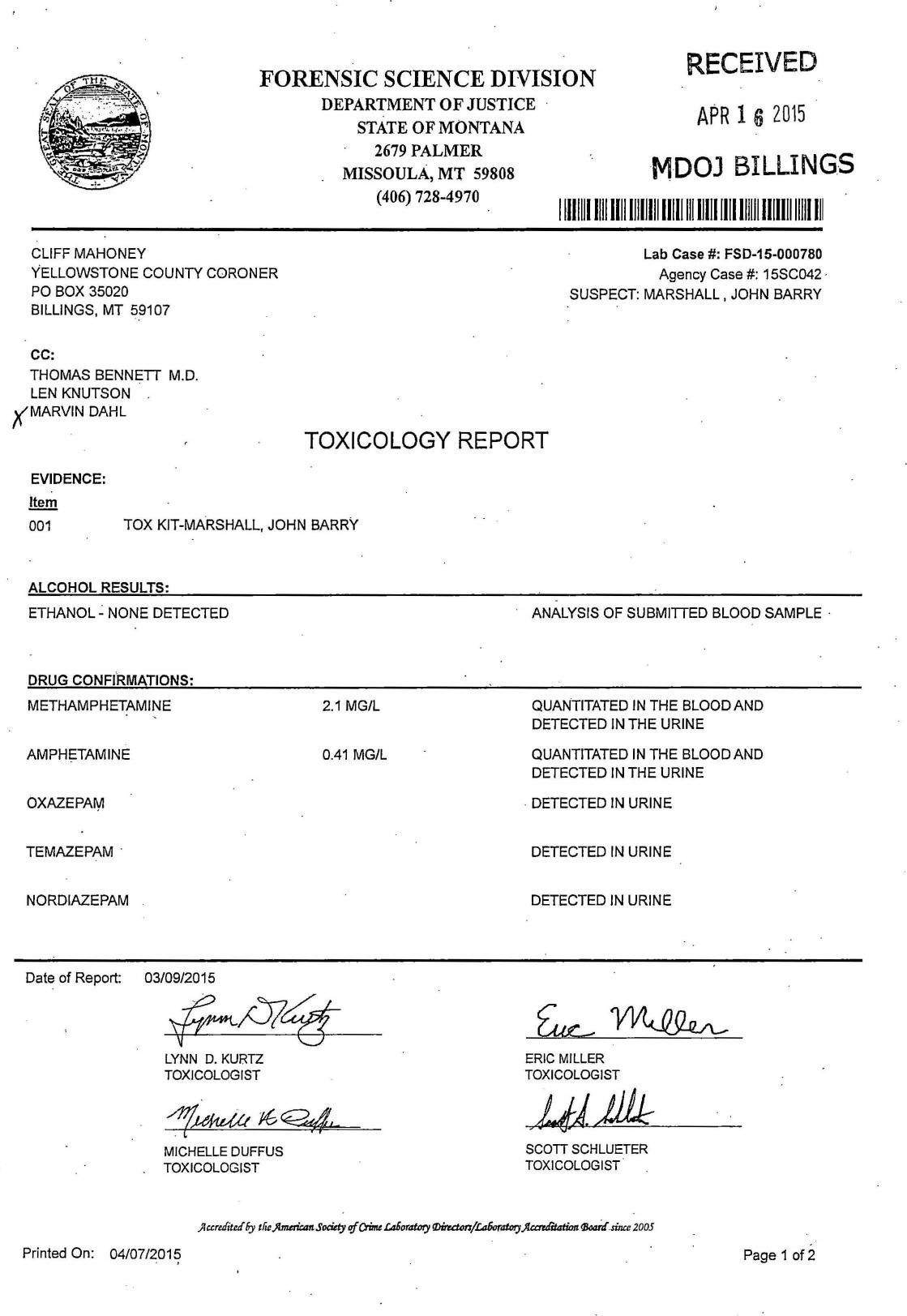
Compared with some drugs, such as opioids, gabapentin appears to be relatively non-lethal in overdose situations, meaning the morbidity associated with a toxic dose is low. 8 However, the primary danger of gabapentin overdose appears when individuals use gabapentin in conjunction with other drugs, such as alcohol or opioids. 9,10 Gabapentin was found at very high frequency in accidental mixed drug fatalities. Gabapentin concentrations were generally within the normal therapeutic range (2-20 μg/mL). It is unknown whether a synergistic effect with opioids may contribute to central respiratory depression. It isn’t as easy to overdose on gabapentin as it is to overdose on more potent drugs like heroin, fentanyl, or oxycodone. However, an overdose is possible if someone takes far too many pills or combines the drug with another intoxicating substance.[2] The objective of this review is to provide a repository of standard and emerging treatment modalities for loperamide, gabapentin and modafinil for the emergency medicine team. Expert opinion: Loperamide, gabapentin, and modafinil are becoming drugs of abuse, and as such, should be on the radar of healthcare providers. Recognizing their unique The purpose of this study is to document the clinical manifestations and outcomes of gabapentin exposures reported to poison centers. Methods: A multicenter prospective observational study of all gabapentin exposures reported to three poisoncenters was conducted between 4/1/98 and 4/1/2000. During that period, there were 62,652 overdose deaths, of which 58,362 had documented toxicology results. Of these, gabapentin was found in 9.7%. Gabapentin was judged to contribute to overdose death in 52.3% of those deaths—or 5.0% of the total deaths from overdose. Gabapentin is used as an anti-epileptic and for neuropathic pain. Adverse effects with gabapentin include severe myopathy, severe myoclonus, neutropenia, hypoglycaemia episodes and altered consciousness. Gabapentin is renally excreted; dose adjustments are required to prevent accumulation and toxicity. Acknowledgments Objective: To raise awareness of serious toxicity, including respiratory depression and PRES (posterior reversible encephalopathy syndrome) caused by gabapentin in the setting of overdose and abuse. Background Gabapentin, a structural analog of γ-aminobutyric acid, although developed for epilepsy, is often used for pain, insomnia and anxiety. Gabapentinoids are commonly ingested in self-harm attempts and often misused for their sedative and euphoric properties. These medications can cause lethargy or agitation in overdose, increase risk of death combined with opioids, and manifest a withdrawal syndrome. Postmortem toxicology tests detected gabapentin in almost 1 in 10 US overdose deaths between 2019 and 2020. In about half of the cases, a medical examiner or coroner ruled the drug was a cause of the death, according to a report from the CDC’s Division of Overdose Prevention. If you or someone you know is experiencing an overdose or toxic reaction to gabapentin, seek immediate medical attention. Don’t administer any medications or drinks unless instructed by qualified medical professionals. In cases in which gabapentin was determined to be a cause of death, the blood concentrations ranged from 1.1 to 134.0 mg/L. Persons who died of a gabapentin-related drug death were prescribed the drug legitimately 91.4% of the time, with 84.2% of those also having a known prior history of abuse or misuse of prescription medications. Data on 62,652 overdose deaths that occurred during 2019–2020 in the 24 jurisdictions were entered in SUDORS; among 58,362 deaths with documented toxicology results, a total of 5,687 (9.7%) had gabapentin detected on postmortem toxicology. Gabapentin-involved deaths occurred in 2,975 of 5,687 decedents (52.3%) with a positive gabapentin test toxicology. Gabapentin-involved deaths occurred in 2,975 of 5,687 decedents (52.3%) with a positive gabapentin test result. Across the study period, the demographic characteristics of decedents remained largely similar. Most gabapentin-involved overdose deaths occurred among non-Hispanic White persons (83.2%) and persons aged 35–54 years (52. Gabapentin, primarily used for treating seizures and neuropathic pain, has been increasingly detected in postmortem toxicology tests, with a rise in overdose deaths noted between 2019 and 2020. While overdose is often associated with misuse or intentional self-harm, accidental ingestion remains a critical concern. Klein-Schwartz W, Shepherd JG, Gorman S et al. Characterization of gabapentin overdose using a poison center case series. Journal of Toxicology-Clinical Toxicology 2003; 41(1):11-15. Lofton AL, Klein-Schwartz W. Evaluation of lamotrigine toxicity reported to poison centers. Annals of Pharmaotherapy 2004; 38:1811-1815. Routine gabapentin postmortem testing and linking of death certificate, medical examiner, coroner, toxicology, and prescription history data will provide more reliable information on the extent of gabapentin misuse, diversion, and implications for clinical care. Of the 58,362 overdose deaths with toxicology results in 2019 and 2020, 5,687 (9.7%) showed positive results for gabapentin. Gabapentin was believed to be a factor in 2,975 of these 5,687 deaths (52.3%). An overwhelming majority of these deaths — around 90% — also involved opioids like fentanyl. Common symptoms of gabapentin overdose are drowsiness, fast heartbeat, dizziness, low blood pressure, nausea, vomiting, and impaired coordination. In severe cases, lethargy, coma, and death may occur. Pregabalin is commonly used for the treatment of neuropathic pain. Overdose leads predominately to CNS effects. Management is supportive. Toxicity / Risk Assessment Management - Lone Pregabalin or Gabapentin exposures are usually well - Supportive care is the mainstay of management
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 | |
 |  |