Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
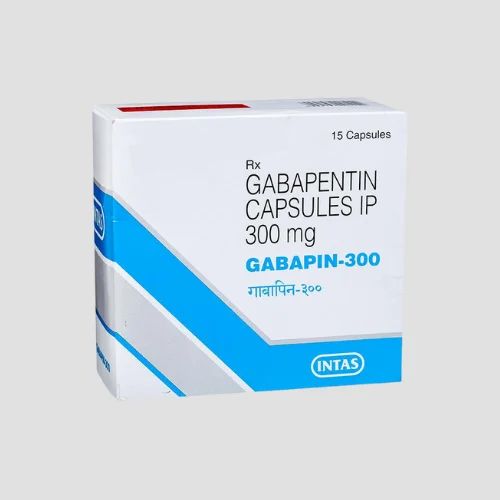
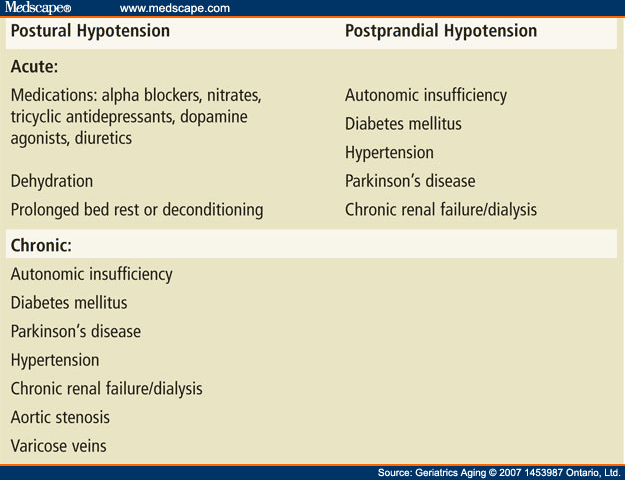
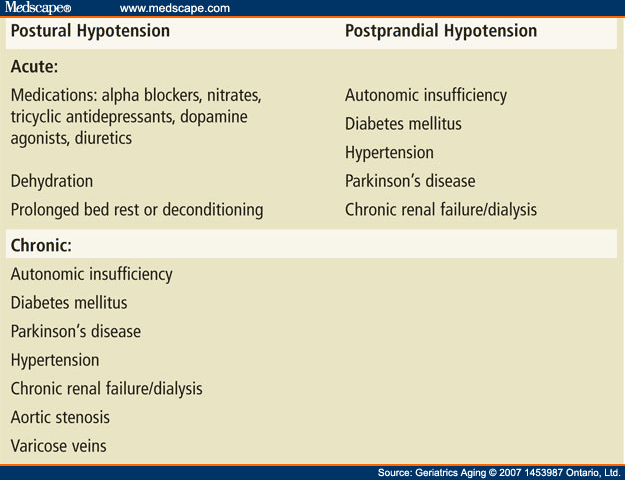
Orthostatic (or postural) hypotension is defined as • a sustained reduction of systolic blood pressure (BP) of ≥20 mmHg and/or diastolic BP of ≥10 mmHg or • systolic BP fall >30 mmHg in hypertensive patients with supine systolic BP > 160 mmHg, when assuming a standing Drug-induced orthostatic hypotension is an important clinical problem. When symptomatic, it is poorly tolerated by the patient, and can be a cause for discontinuing treatment. It may have more serious consequences if it leads to syncope, falls and injury, or to sustained loss of perfusion of vital o Patients can be asymptomatic and they should be assessed to confirm postural hypotension, with a medication review carried out. Measure the BP. Postural hypotension is defined as a sustained reduction in the systolic BP by at least 20 mmHg or the diastolic BP of at least 10 mmHg within 3 minutes of standing or a 60° head tilt. Child 6–11 years 10 mg/kg once daily (max. per dose 300 mg) on day 1, then 10 mg/kg twice daily (max. per dose 300 mg) on day 2, then 10 mg/kg 3 times a day (max. per dose 300 mg) on day 3; usual dose 25–35 mg/kg daily in 3 divided doses, some children may not tolerate daily increments; longer intervals (up to weekly) may be more appropriate, daily dose maximum to be given in 3 divided Orthostatic hypotension is defined as a decrease in blood pressure of 20 mm Hg or more systolic or 10 mm Hg or more diastolic within three minutes of standing from the supine position or on What causes postural hypotension? Postural hypotension can be caused by many factors but common causes include: • Certain medications (such as blood pressure tablets) • Dehydration • Prolonged bed rest • Heart conditions • Warm environments • Damage to the nervous system (for example Parkinson’s disease) We would like to show you a description here but the site won’t allow us. Orthostatic hypotension (OH) is a common side effect of drugs. It causes a reduction in blood pressure (BP) on standing, which results in reduced cerebral blood flow that is linked to falls, strokes, cognitive impairment, and increased mortality. Over 250 medications are associated with OH. Orthostatic hypotension is a condition described by a significant reduction in blood pressure that typically occurs upon standing or assuming an upright posture. It may be asymptomatic or symptomatic and can be due to impaired autonomic reflexes or intravascular volume depletion. Abstract. Neurogenic orthostatic hypotension is a distinctive and treatable sign of cardiovascular autonomic dysfunction. It is caused by failure of noradrenergic neurotransmission that is associated with a range of primary or secondary autonomic disorders, including pure autonomic failure, Parkinson’s disease with autonomic failure, multiple system atrophy as well as diabetic and Chronic orthostatic hypotension (OH) is a common, often underdiagnosed, disorder, defined by an excessive fall in blood pressure (BP) with standing. OH can be associated with postural lightheadedness, dizziness, fatigue, coat hanger pain, and, in extreme situations, syncope, falls, and injuries. Hoehn MM 1975. Levodopa-induced postural hypotension. Treatment with fludrocortisone. Arch Neurol 32, 50–51. [Google Scholar] Hoeldtke RD, Horvath GG, Bryner KD, Hobbs GR 1998. Treatment of orthostatic hypotension with midodrine and octreotide. J Clin Endocrinol Metab 83, 339–343. [Google Scholar] Orthostatic hypotension (OH) is an impaired blood pressure (BP) response to the upright position which is defined by a systolic BP drop ≥ 20 mmHg or by an absolute systolic BP value ≤ 90 mmHg and/or a diastolic BP drop ≥ 10 mmHg within 3 minutes of standing [1, 2]. Orthostatic hypotension is a frequent cause of falls and syncope, impairing quality of life. It is an independent risk factor of mortality and a common cause of hospitalizations, which exponentially increases in the geriatric population. We present a management plan based on a systematic literature review and understanding of the underlying pathophysiology and relevant clinical pharmacology Figure. Spectrum of orthostatic hypotension (OH). Clinical development of OH requires the presence of autonomic impairment (due to aging, diabetes, and primary autonomic neuropathies) often in combination with aggravating factors that overwhelm or impair compensatory autonomic responses (volume depletion, infections, deconditioning, and medications). The overall rate is approximately 36 per 100,000 US adults and increases exponentially with age. 1 In patients older than the age of 75 years, the annual hospitalization rate related to orthostatic hypotension increases to 233 per 100,000 patients. 2 The prevalence of orthostatic hypotension in institutionalized patients ranges between 30% and The depressor effect of gabapentin in the NTS recovered gradually over 90 min after L-NAME treatment (-8 ± 2 versus -20 ± 3 mmHg and -13 ± 3 versus -36 ± 8 bpm; Figure 2B). These results indicated that gabapentin may have induced NOS to induce hypotension and bradycardia in the NTS of the SHR rats. Figure 2. Orthostatic hypotension (OH) is a common side effect of drugs. It causes a reduction in blood pressure (BP) on standing, which results in reduced cerebral blood flow that is linked to falls, strokes, cognitive impairment, and increased mortality. Over 250 medications are associated with OH. Orthostatic hypotension is a chronic, debilitating illness that is difficult to treat. The therapeutic goal is to improve postural symptoms, standing time, and function rather than to achieve upright normotension, which can lead to supine hypertension. Drug therapy alone is never adequate. Perioperative gabapentin administra-tion has been associated with greater incidence of dizzi-ness, visual disturbances, and increased risk for postop-erative pulmonary complications. We present a 13-year-old female who experienced intraoperative hypotension which was eventually attributed to the preoperative ad-ministration of gabapentin.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |