Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 | |
 |  |
 |  |
 |  |
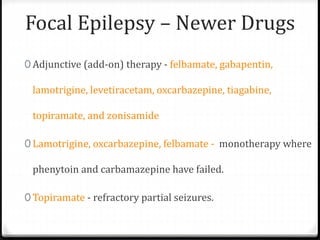
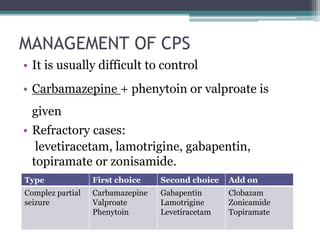
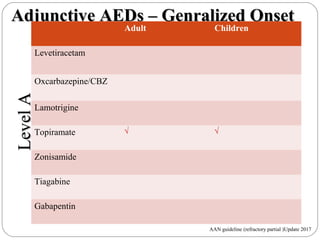
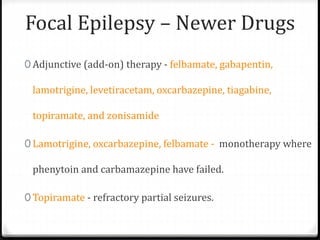
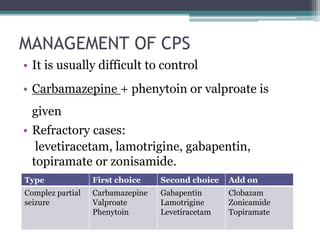
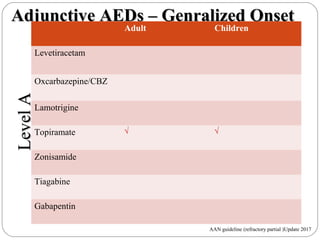
The results of three large, placebo-controlled, multicenter clinical trials of gabapentin as add-on therapy in patients with refractory partial seizures are summarized in a report from the Departments of Neurology and Psychiatry and the International Center for Epilepsy, University of Miami School of Medicine, and the Veterans Affairs Medical Gabapentin (usually 600 to 1800 mg/day) provides notable benefit, reducing seizure frequency by ⩾ 50% in 18 to 28% of patients with refractory partial seizures, as shown in 3 double-blind, placebo-controlled trials. Addition of gabapentin to phenobarbitone and/or potassium bromide increased the interictal period and shortened the post-seizure recovery in some canine epileptics. In some dogs, seizures were prevented completely, while in others there was an increase in interictal period. The short-half life of ga This therapy may improve if combination therapy with potassium bromide (KBr) is used. More recently, several human drugs, such as gabapentin and levetiracetam, have been evaluated for seizure therapy in veterinary patients. This article will discuss anticonvulsant drug use in dogs with so-called 'refractory' or 'intractable' epilepsy. Gabapentin. Gabapentin is a recent addition to the human anti-convulsant market, which has primarily been used as an adjunctive drug for humans with uncontrolled partial seizures with and without secondary generalization. Gabapentin is well absorbed from the duodenum in dogs with maximum blood levels reached in 1 hour after oral administration. A 2005 study investigated gabapentin as an add-on anticonvulsant in dogs with refractory seizures and found that in a 4-month period, 3 of 17 dogs were seizure-free and 4 other dogs had a 50% reduction in seizure frequency. In people with drug‐resistant focal epilepsy, gabapentin has efficacy as an add‐on treatment. Moderate‐certainty evidence for the outcomes from this review suggests that a dose of 1800 mg/day will reduce seizure frequency by at least 50% in 25.3% of people (95% confidence interval 19.3% to 32.3%). Our experience indicates that gabapentin can be an effective adjunctive AED in children with refractory partial seizures. About a third of the patients had a greater than 50% reduction in seizure frequency, and two patients became seizure free. Gabapentin may be an effective adjunctive medication in children with refractory partial seizures. Behavioral side effects were reversible when the drug was discontinued and were most prominent in the mentally retarded. The efficacy of gabapentin in the management of refractory canine epilepsy has been evaluated in two studies (Platt et al, 2006; Govendir et al, 2005). The first study reported 11 dogs that were already receiving phenobarbital and potassium bromide at therapeutic serum concentrations and were deemed to have poor seizure control (Platt et al, 2006). Delahoy and colleagues 29 showed that in patients with refractory partial epilepsy, pregabalin was more effective than gabapentin on clinical response and the number of seizure-free days over the last 28 days. The efficacy and safety of gabapentin (GBP) as add-on therapy in 237 children, aged 3 to 12 years, with refractory partial seizures were studied at the Alder Hey Children’s Hospital, There are two clinical reports of gabapentin use as an add-on drug for dogs with refractory epilepsy. Overall, the responder rate of these dogs was between 41% and 55%. Because of its short t ½, gabapentin probably needs to be administered at least every 8 hrs, and possibly every 6 hrs, in order to maintain serum gabapentin concentrations The second study evaluated 17 dogs with refractory seizures that were administered gabapentin at a dose of 35 to 50 mg/kg/day divided twice or three times daily, also in conjunction with phenobarbital and potassium bromide (16 dogs) or phenobarbital alone (1 dog).9 This study found no significant decrease in the number of seizures over the The National Institute for Health and Care Excellence (NICE) recommends gabapentin only as adjunctive treatment for refractory focal seizures in children, young people, and adults and for treatment of children and young people with benign epilepsy with centrotemporal spikes, Panayiotopoulos syndrome, or late‐onset childhood occipital epilepsy Drugs used for the treatment of refractory epilepsy that demonstrated the best short-term efficacy tolerability include vigabatrin, sodium valproate, gabapentin, and levetiracetam. Vigabatrin's association with visual changes with chronic use excludes it from joining sodium valproate, levetiracetam, and gabapentin in demonstrating the most control seizure activity. Gabapentin, a commonly prescribed AED, has shown efficacy in the treatment of epilepsy. This abstract aims to summarize the effectiveness of gabapentin in managing epilepsy based on available clinical evidence. Numerous studies have investigated the efficacy of gabapentin in epilepsy treatment. Gabapentin (GBP) is one of several novel anti-epileptic drugs effective as an add-on therapy for intractable seizures but has not been studied in patients with cerebral tumours. This short-term inpatient study in adults demonstrates that gabapentin monotherapy is an effective and safe treatment for refractory complex partial and secondarily generalized seizures. conclude that gabapentin can be a useful adjunctive medication in the treatment of refractory partial epilepsy in children. (J Pediatr 1996; 128:829-33) Epilepsy is an important cause of morbidity in children, With an estimated prevalence of 0.5% to 1%. 1 Approximately one
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 | |
 |  |
 |  |
 |  |