Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 | |
 |  |
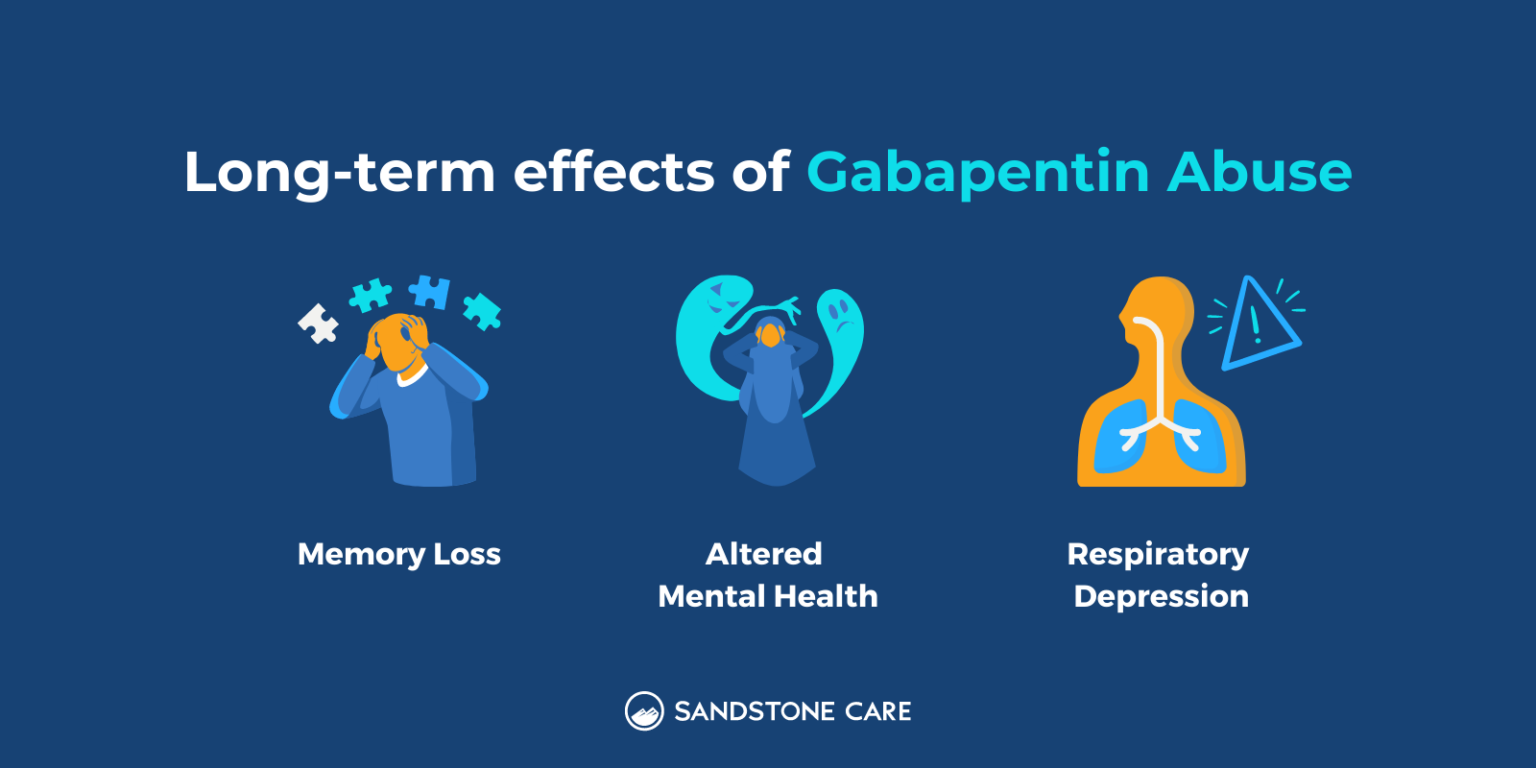
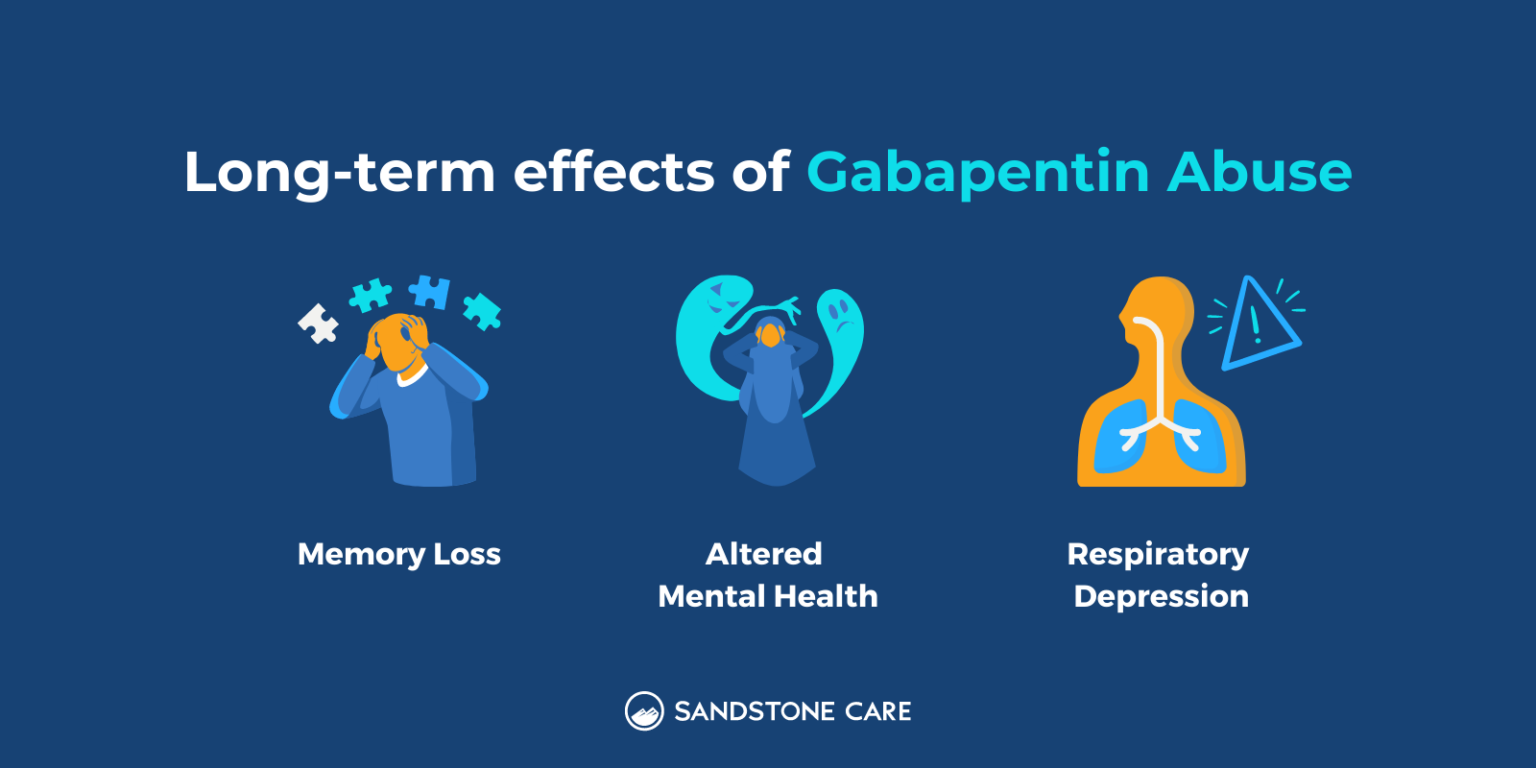
In the study suggesting that there was a dementia risk, it was strongest in younger people. I conclude that you aren’t doomed. Long-term Gabapentin therapy for chronic pain is not associated with a differential risk of dementia across dosage levels, irrespective of age or gender. Further study into its potential cognitive impacts is essential. Background: Gabapentin is increasingly prescribed to older adults, which raises concerns about its potential to cause neurocognitive changes. Therefore, we aimed to examine the association of gabapentin use with neurocognitive changes (i.e., cognitive decline, functional status decline, and motor function change) in older adults. The adjusted odds ratio for dementia risk associated with gabapentin use was 0.91 (95 % C.I. 0.83–1.01), indicating no substantial increase in risk. Conclusion Long-term Gabapentin therapy for chronic pain is not associated with a differential risk of dementia across dosage levels, irrespective of age or gender. Given the known increased risk of dementia with certain medications, we try to get patients off of these medications, if possible. We have seen patients’ cognition improve as a result. Q. Especially in older adults, gabapentin is prescribed to treat behavioral and psychological symptoms of dementia (BPSD) (Kim et al., 2008). Several studies have reported that gabapentin has a deleterious effect on cognition (Leach et al., 1997; Meador et al., 1999; Shem et al., 2018). This study investigated prevalence of gabapentin use from 2006 to 2019 and found increasing trends among all levels of cognitive status. Of concern, a high proportion of participants with dementia seemed to be more at risk of inappropriate use of gabapentin with concurrent CNS-active medications. One drug in that last class, gabapentin, accounted for one-third of all the days of prescription supply that the patients in the study received during the study period. While gabapentin is approved to treat epilepsy, few of these older adults had a seizure disorder. We conducted this population-based cohort study to understand the risk of acute altered mental status and mortality within 30 days of initiating a high versus low dose of gabapentin in older adults, a segment of the population at higher risk of adverse drug events. Several studies suggest that using gabapentin and pregabalin for epilepsy control is associated with an increased risk of dementia, and the effect appears to be lifelong (Knight et al., 2021). However, these studies specifically involved patients with epilepsy or medically ill patients. Even people taking nonsteroidal anti-inflammatory drugs (NSAIDs) for pain had a high risk of developing dementia. It’s unclear whether the risk of dementia is related to taking pain medication or to the effects of chronic pain on the brain, or both. One newer study showed that older adults with chronic pain had a higher risk of developing The evidence of gabapentin and dementia is mixed, with two studies looking at hundreds of thousands of people and coming to completely different conclusions. No significant difference in the risk of dementia was found between low and high cumulative doses of gabapentin. The adjusted odds ratio for dementia risk associated with gabapentin use was 0.91 (95 % C.I. 0.83–1.01), indicating no substantial increase in risk. Gabapentin use was significantly associated with decline in cognitive and functional status among older adults with initially normal cognition. Further studies are needed to examine the association. The multivariate-adjusted hazard ratio of risk of dementia for gabapentin or pregabalin exposure versus the matched non-exposed group was 1.45 (95% confidence interval [CI], 1.36-1.55). The risk of dementia increased with higher cumulative defined daily doses during the follow-up period. Gabapentin has been increasingly prescribed to older adults for off-label indications, and accumulating evidence suggests potential for gabapentin misuse and related adverse events. However, the relation between gabapentin initiation and longer-term neurocognitive changes is not well understood. As the FDA and the Beers 2019 criteria warn about using gabapentin concurrently with some medications due to risk of respiratory depression (U.S. Food and Drug Administration, 2019; By the 2019 American Geriatrics Society Beers Criteria® Update Expert Panel, 2019), further studies are needed to examine the risk of concurrently using gabapentin Moreover, dementia risk increased along with the cumulative dose. Taking an anticholinergic for the equivalent of three years or more was associated with a 54% higher dementia risk than taking the same dose for three months or less. The University of Washington study is the first to include nonprescription drugs. The short answer is: yes, emerging evidence suggests that gabapentin, and its close relative pregabalin, may indeed increase the risk of developing dementia, particularly with long-term use and higher cumulative doses. While it’s not a definitive “cause,” studies are highlighting a concerning correlation that warrants further The multivariate-adjusted hazard ratio of risk of dementia for gabapentin or pregabalin exposure versus the matched non-exposed group was 1.45 (95% confidence interval [CI], 1.36–1.55). The risk of dementia increased with higher cumulative defined daily doses during the follow-up period.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 | |
 |  |