Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
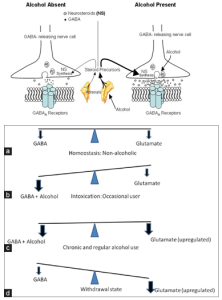
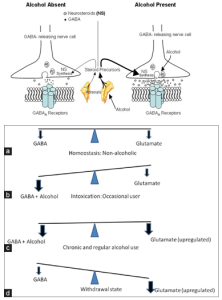
Gabapentin dependence and withdrawal requiring an 18-month taper in a patient with alcohol use disorder: a case report. Gabapentin has been widely used to manage post-herpetic neuralgia, peripheral neuropathy, seizure disorders, alcohol use disorder (AUD), alcohol withdrawal, and insomnia. Prescribing information and the American Addiction Centers recommend tapering gabapentin over a minimum of one week. Using a slow taper by reducing the daily dose at a rate of 300 mg every 4 days may be particularly useful for elderly patients or other patients vulnerable to withdrawal symptoms. See tables 1 through 5 for case reports describing gabapentin tapers. A PHB taper has also been studied, DeFoster RE, Morgan RJ, Leung JG, et al. Use of gabapentin for alcohol withdrawal syndrome in the hospital setting: a safety profile, gabapentin may be a viable ad-juvant because emerging data may suggest a potential role in the management of acute alcohol withdrawal.12,14,15 Gabapentin for Alcohol Withdrawal at VAPORHCS Although not currently included in the alcohol withdrawal protocol at Veterans Affairs Port-land Health Care System (VAPORHCS), gaba- Find out what you need to know about gabapentin for alcohol withdrawal and discover the pros, cons, risks, and benefits, and how it may affect health. Gabapentin is effective at reducing drinking among people with alcohol use disorder (AUD) and strong withdrawal symptoms, according to a study published in JAMA Internal Medicine. While gabapentin is not yet an FDA-approved treatment for alcoholism, a number of studies support the its use withdrawal and cravings: In a 12-day study detoxifying with either gabapentin or lorazepam (a benzodiazepine prescribed with the brand name Ativan), the former was less likely to drink – and had less craving, anxiety, and sedation. Early initiation of high-dose gabapentin was associated with a significant reduction in benzodiazepine exposure, faster stabilization of alcohol withdrawal-related symptoms, and shorter hospital length of stay. Physicians should monitor outpatients with alcohol withdrawal syndrome daily for up to five days after their last drink to verify symptom improvement and to evaluate the need for additional Gabapentin has been shown to be safe and effective for mild alcohol withdrawal but is not appropriate as mono-therapy for severe withdrawal owing to risk of seizures. During early abstinence, gabapentin may improve sleep, cravings, and mood—factors associated with relapse. We would like to show you a description here but the site won’t allow us. UpToDate ⦁ Gabapentin is advantageous for withdrawal because (unlike benzos) it can be continued for long-term treatment to prevent future alcohol relapse Moderate Outpatient Withdrawal With Benzodiazepines Clonazepam (Klonopin) is usually the first-choice benzodiazepine for outpatient withdrawal due to a lower likelihood of causing euphoria. Gabapentin is one medication shown in small studies to reduce the need for benzodiazepines in the setting of alcohol withdrawal. The continuation of gabapentin after alcohol withdrawal appears to be safe during early sobriety and may aid in reducing alcohol-related cravings or returning to alcohol consumption. Alcohol Clin Exp Res. 2009 Sep; 33(9): 1582–1588. PMID: 19485969; ↑ Myrick, H et al. A double-blind trial of gabapentin versus lorazepam in the treatment of alcohol withdrawal. Alcohol Clin Exp Res. 2009 Sep;33(9):1582-8. PMID: 19485969; ↑ Barrons R et al. The role of carbamazepine and oxcarbazepine in alcohol withdrawal syndrome. Prior withdrawal is a risk factor for future episodes. Prior alcohol withdrawal seizures is a risk factor for more severe alcohol withdrawal. 50% of persons with history of long term, heavy alcohol use will have mild alcohol withdrawal. 10% of symptomatic individuals will progress. Generalized tonic clonic seizures. Gabapentin is efficacious for the treatment of acute alcohol withdrawal symptoms 29,30 and also provides short-term relapse prevention after medicated alcohol detoxification, 31 perhaps by an effect on sleep normalization. 32,33 Post hoc analysis has shown effectiveness of treatment with gabapentin, in combination with flumazenil 34 or A fixed-dose gabapentin taper protocol appears to be an effective and safe alternative to CIWA-driven benzodiazepines in patients hospitalized with alcohol withdrawal syndrome, though further research is necessary to define the potential subpopulations that benefit most. Gabapentin has been widely used to manage post-herpetic neuralgia, peripheral neuropathy, seizure disorders, alcohol use disorder (AUD), alcohol withdrawal, and insomnia. Although usually well tolerated, gabapentin has been reported to cause severe physiologic dependence and withdrawal. Tapering gab The propensity score for being treated with gabapentin was estimated using a logistic regression model incorporating the following pretreatment variables: age, sex, number of prior admissions with alcohol withdrawal, prior documented alcohol withdrawal seizures or delirium tremens, prior treatment of alcohol withdrawal with gabapentin, prior
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |