Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
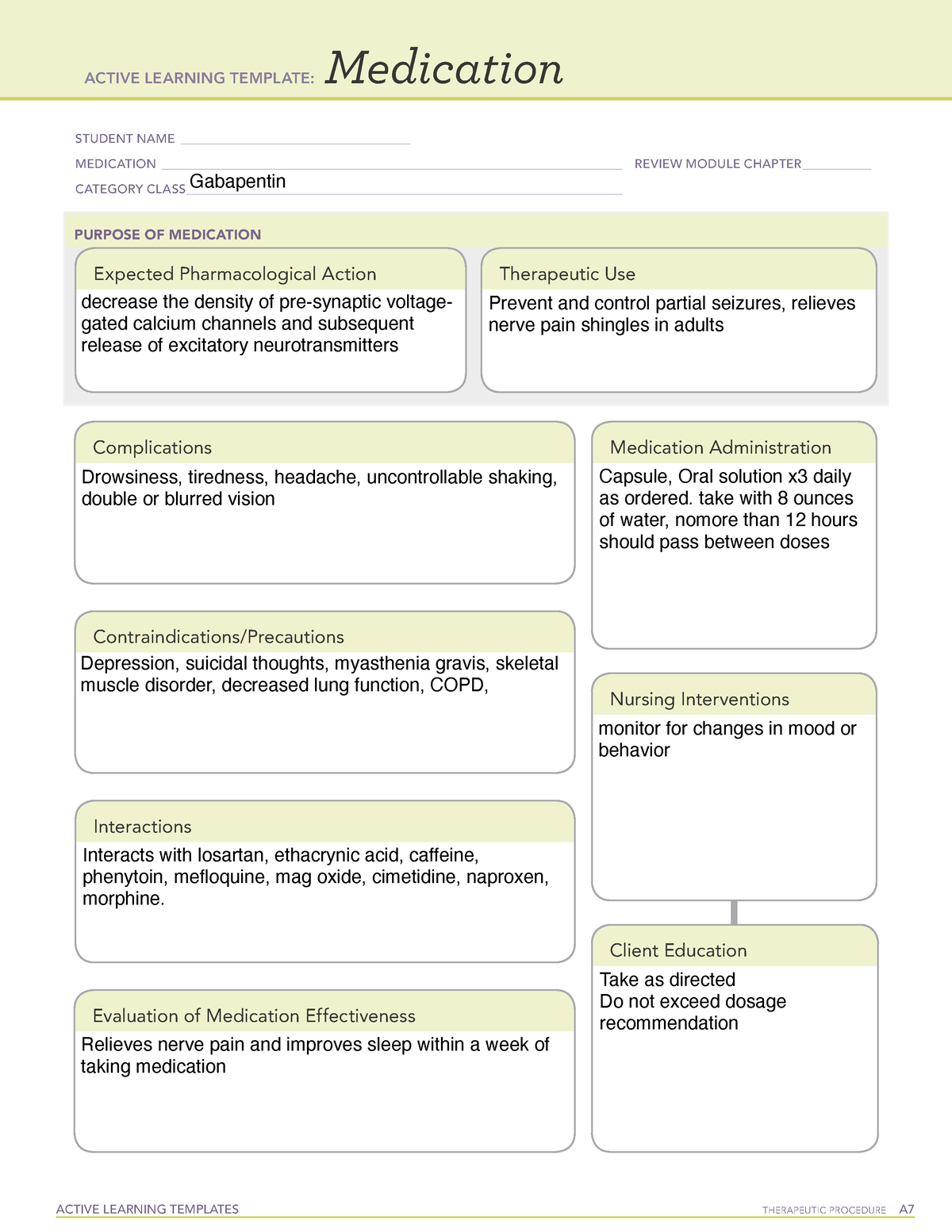 | 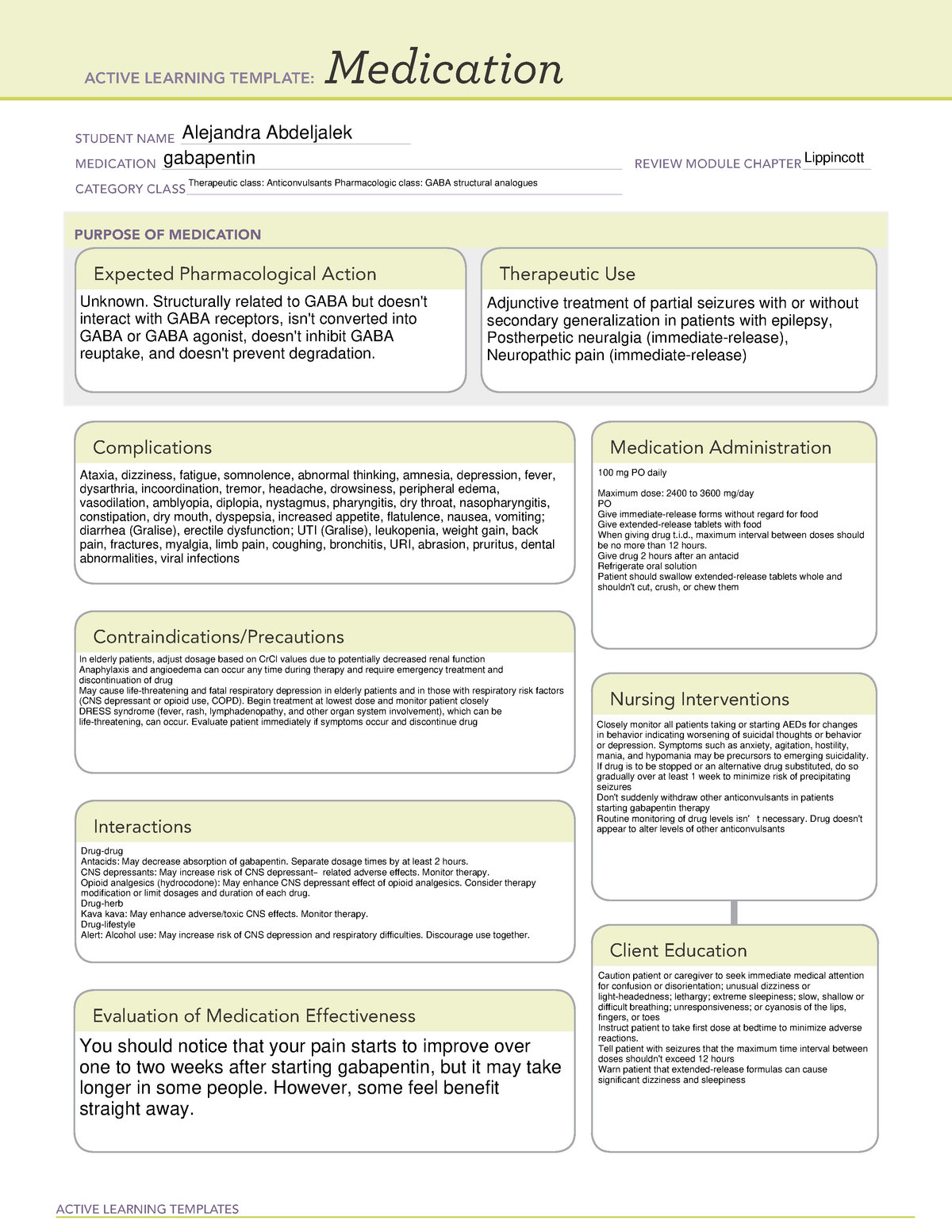 |
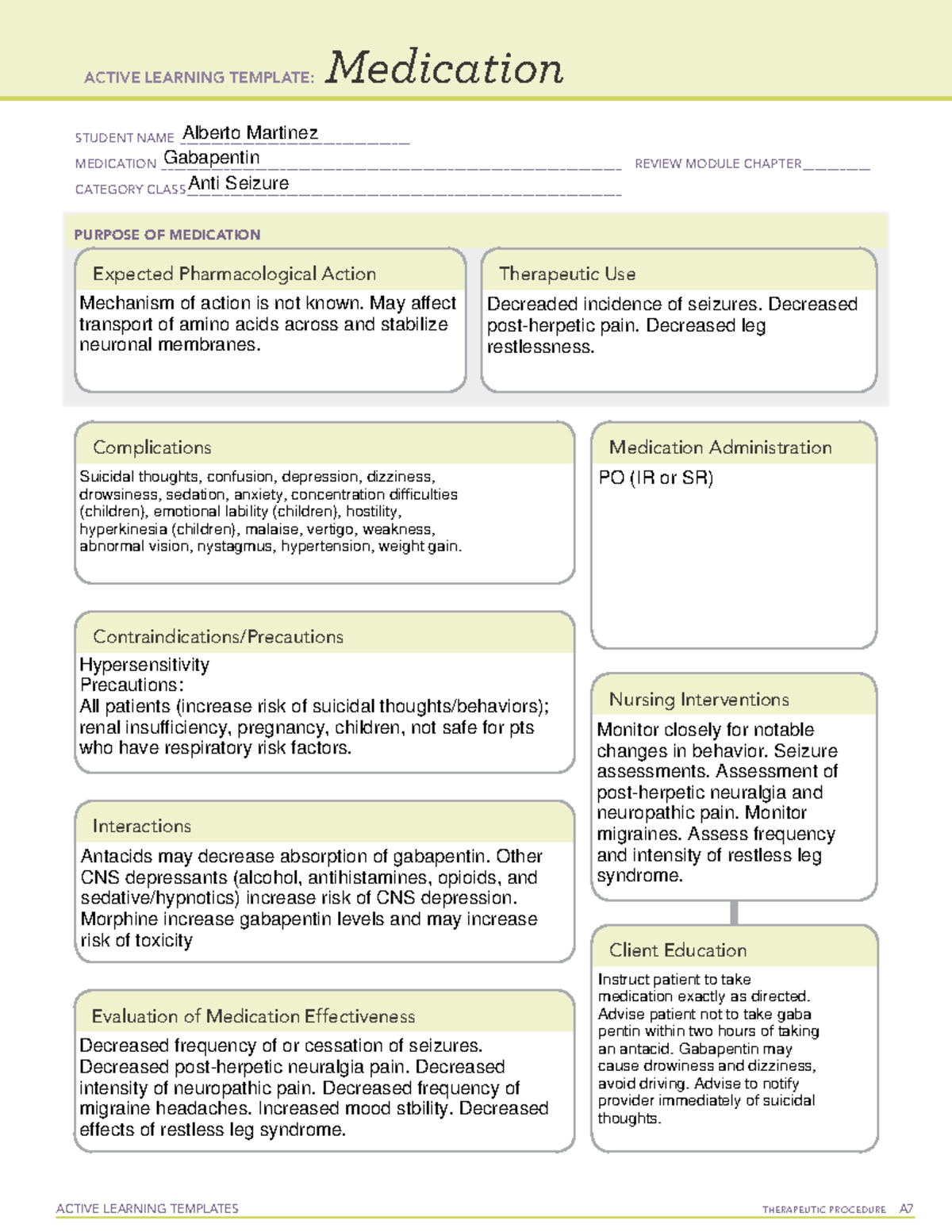
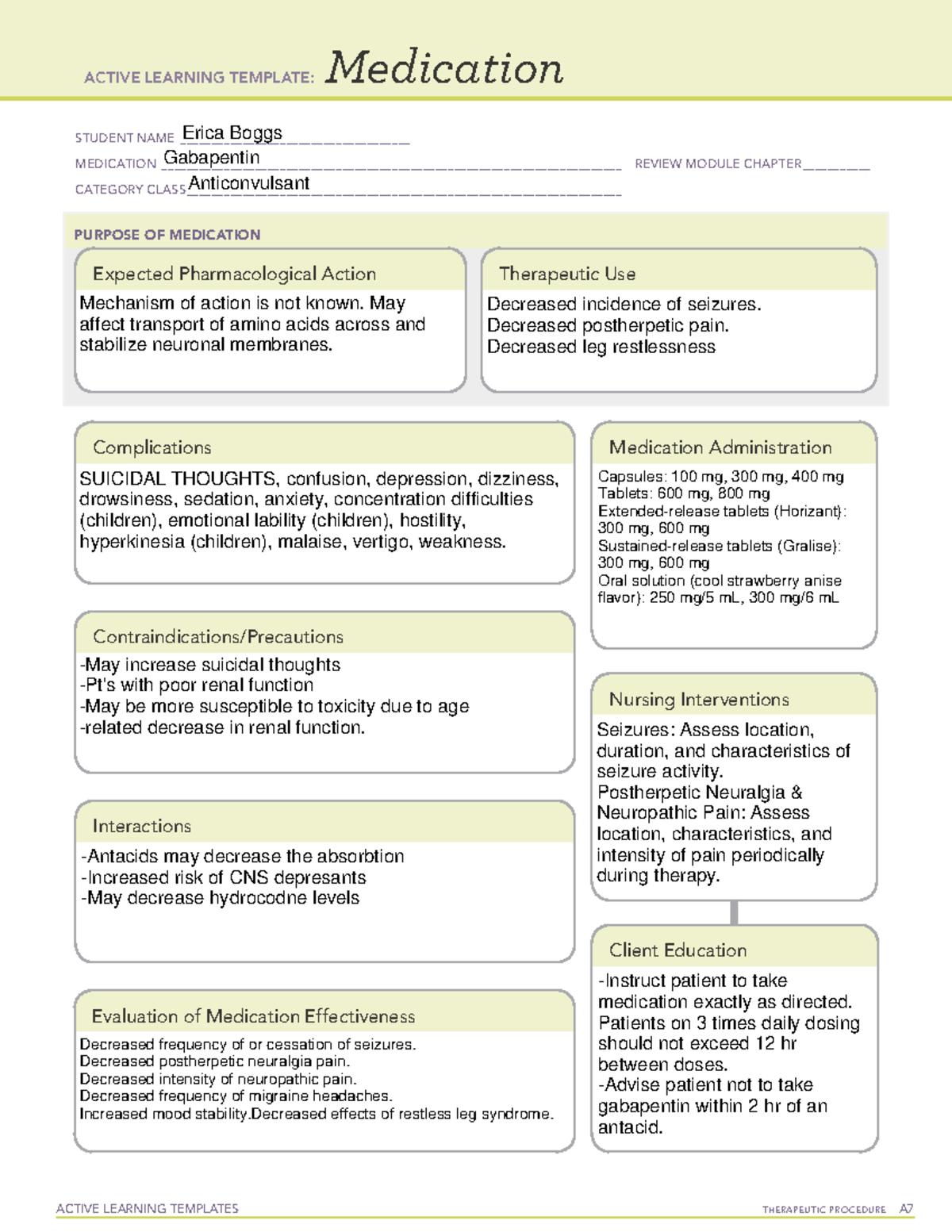
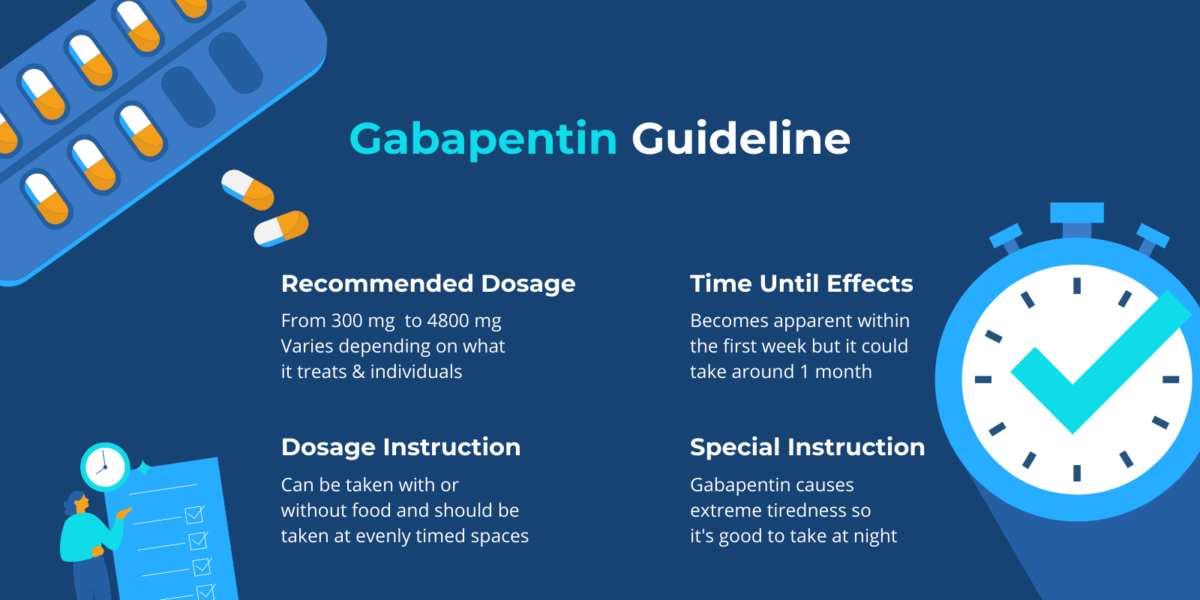
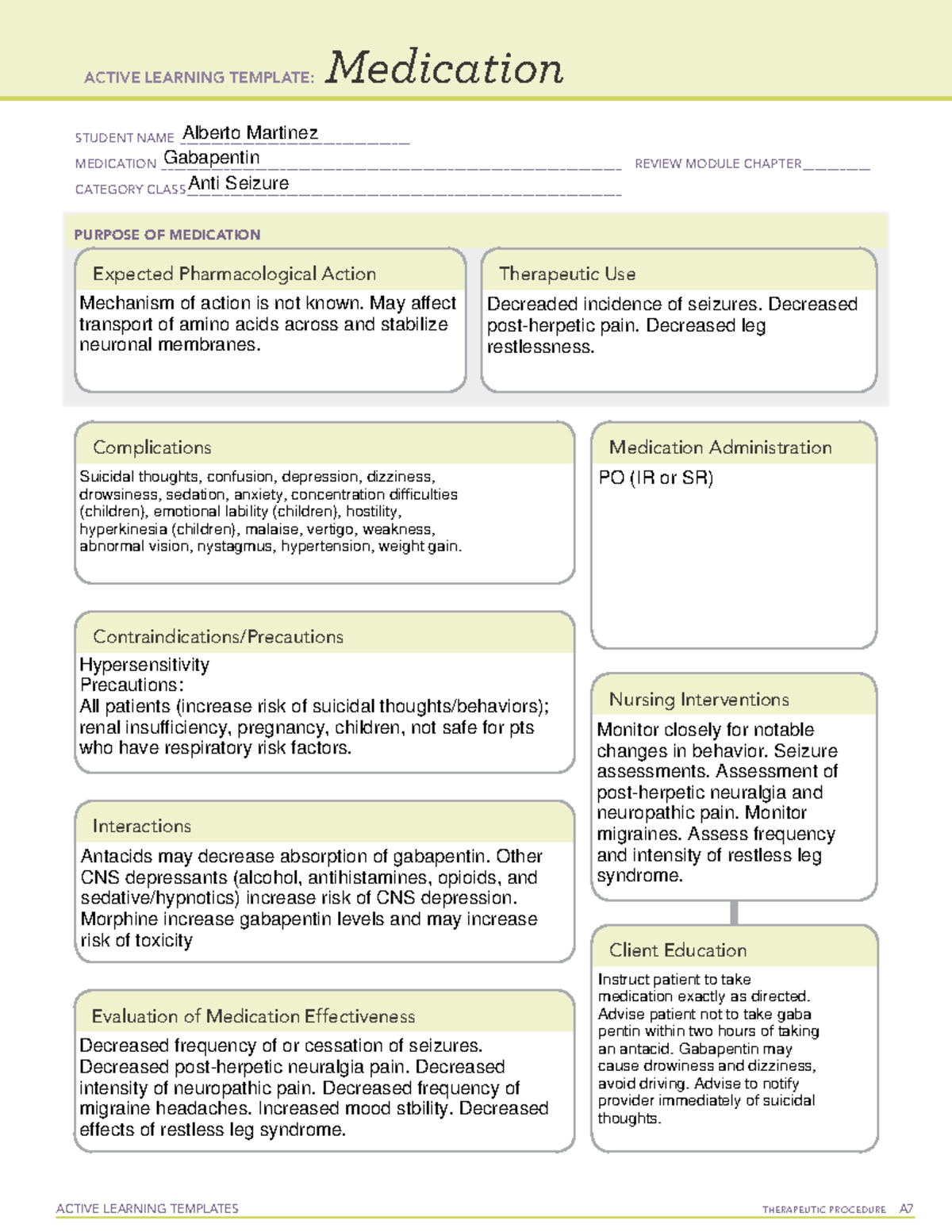
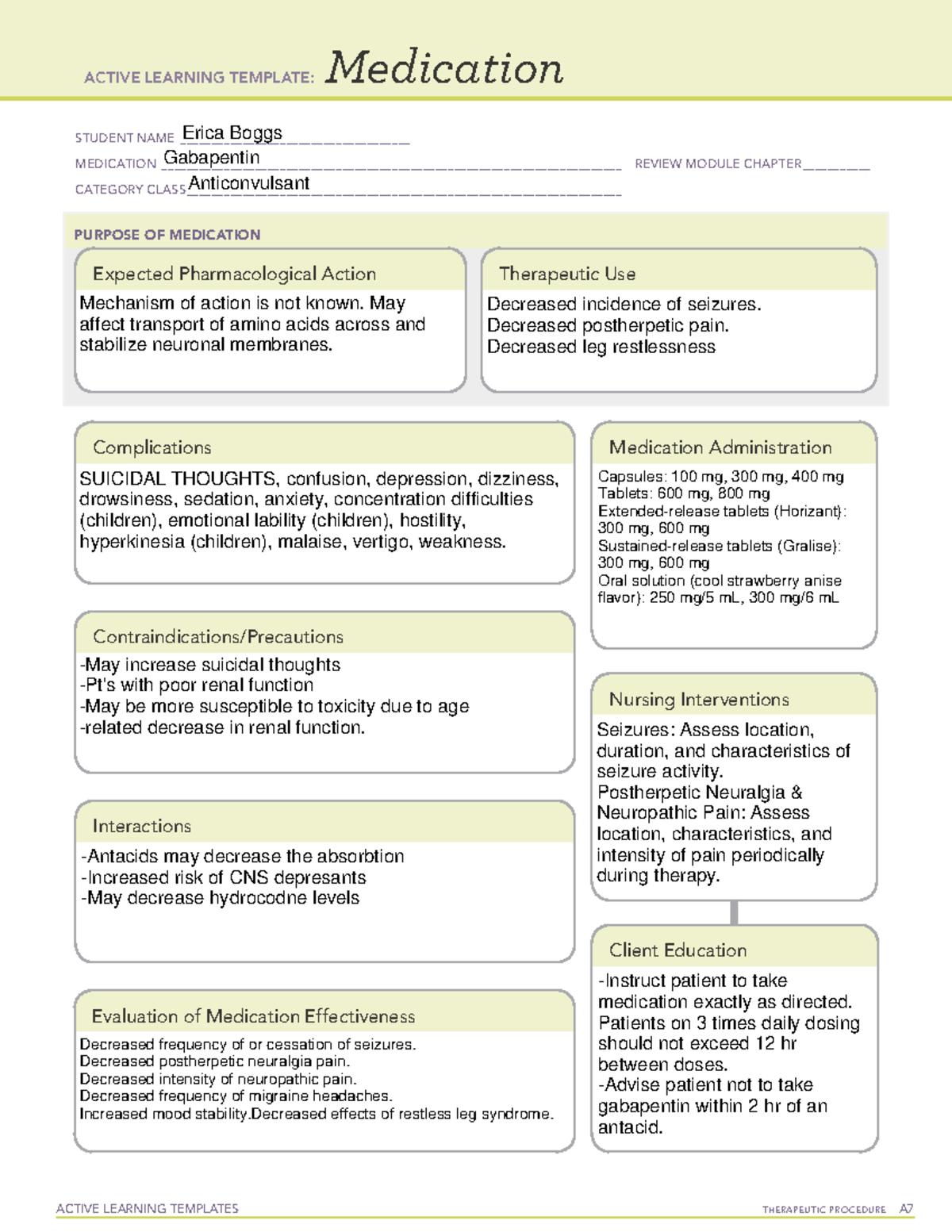
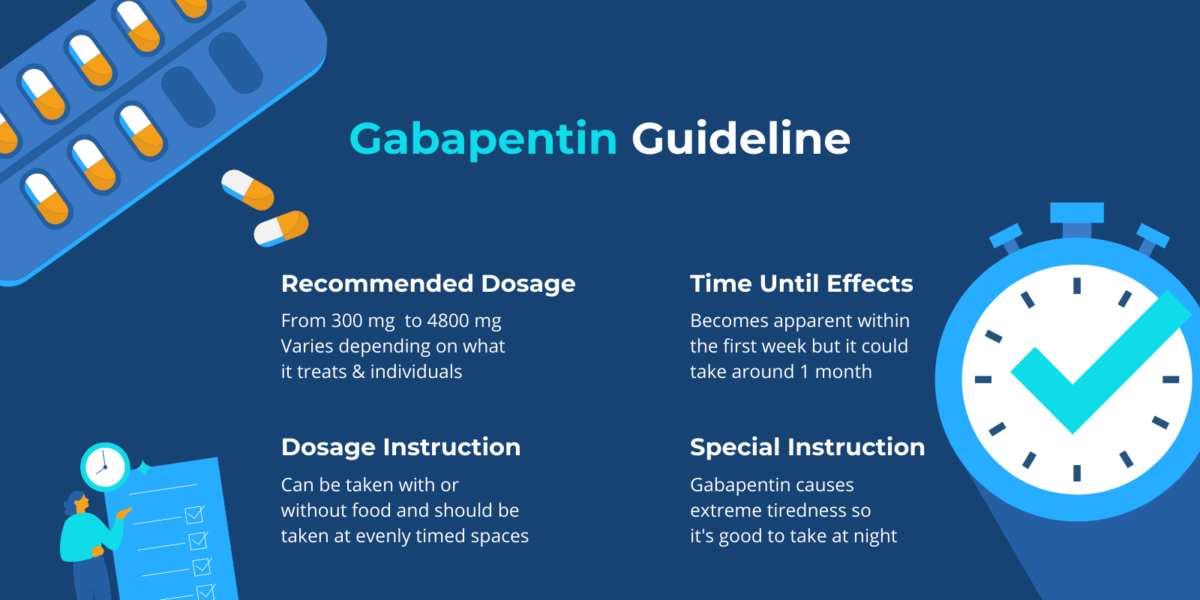
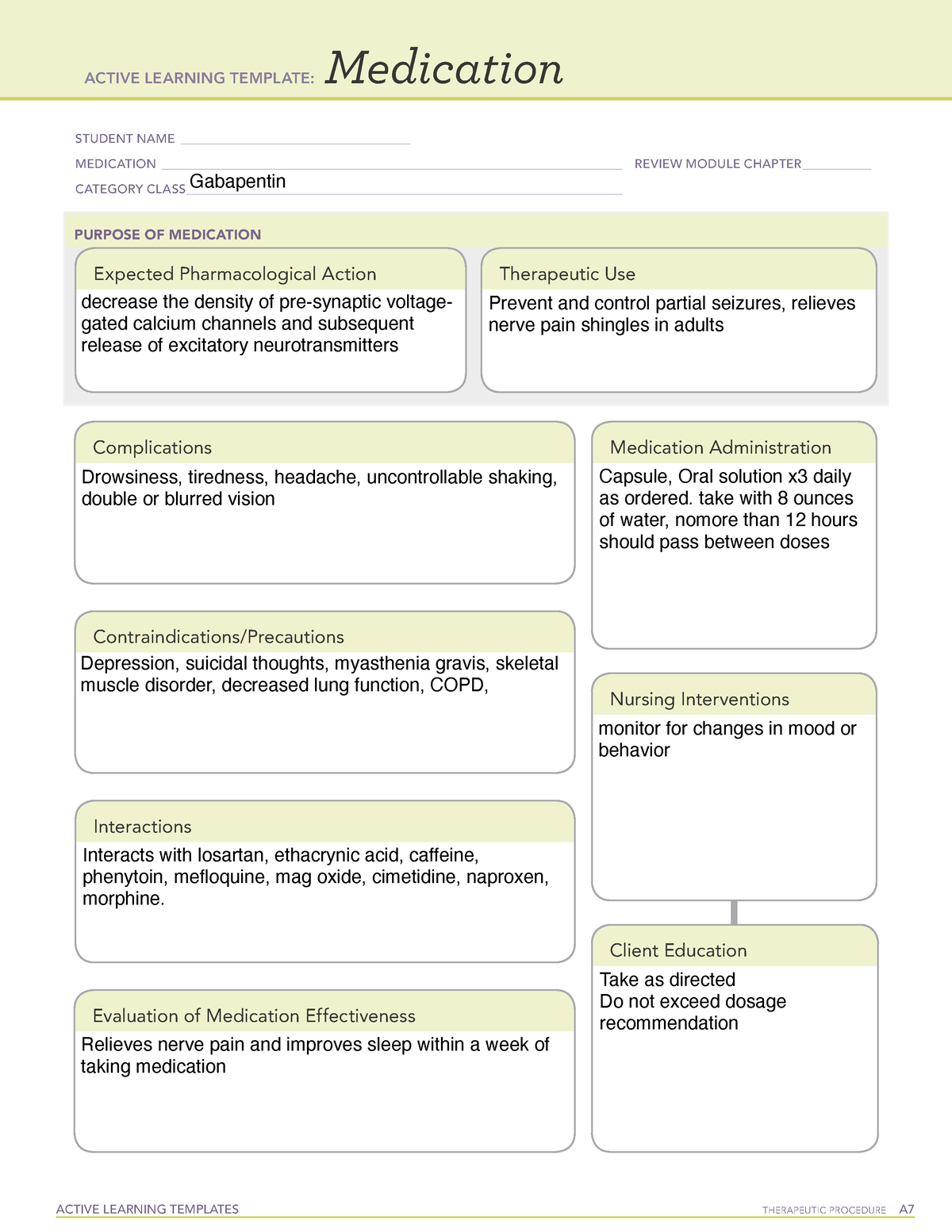
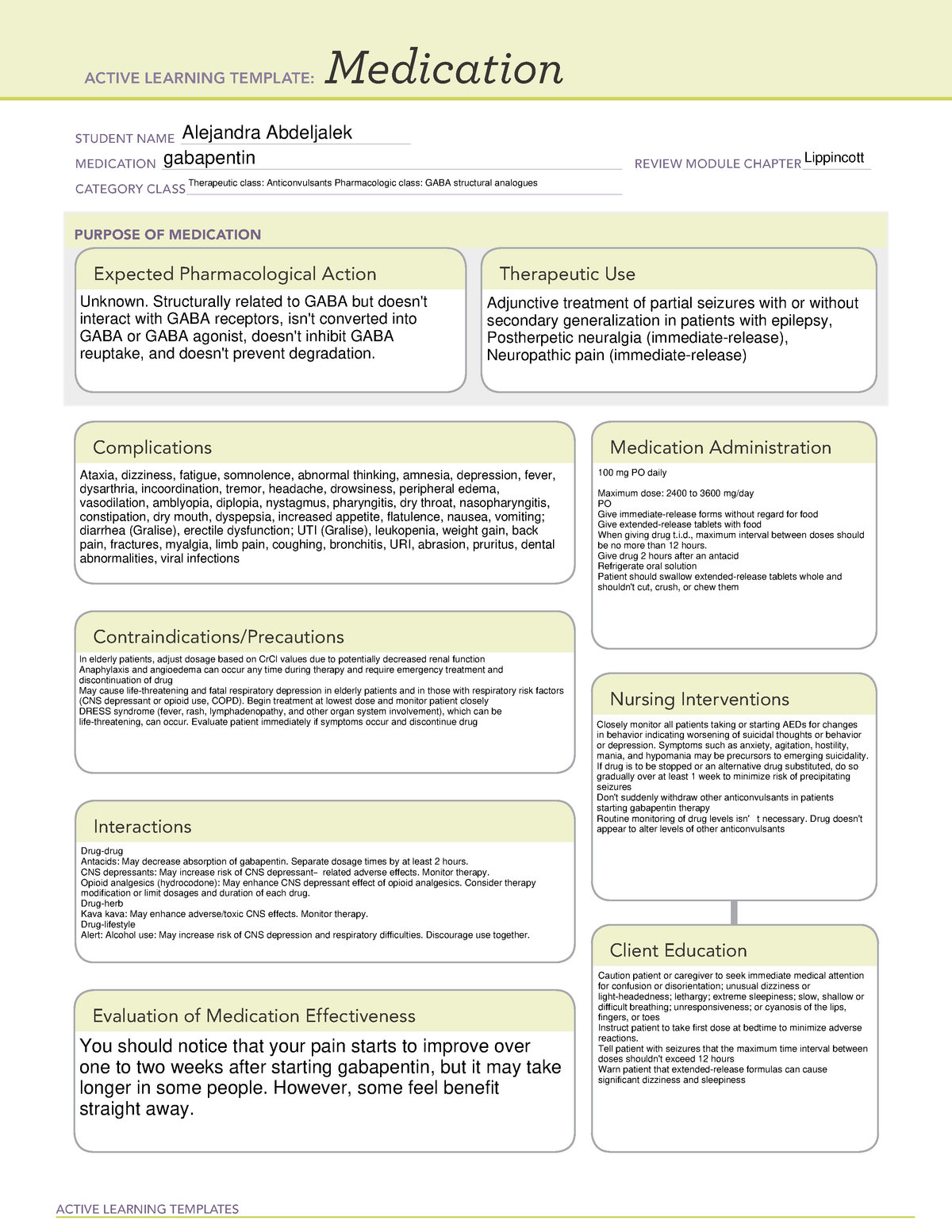
In the 2012 AASM CPG on RLS treatment, the dopamine agonists (pramipexole and ropinirole) were considered STANDARD treatments. 1 Levodopa with a dopa decarboxylase inhibitor, opioids, gabapentin enacarbil, and cabergoline (with caveats) were considered GUIDELINE level recommendations. Several treatments were considered at an OPTIONAL level of Tricyclic antidepressants, dual reuptake inhibitors of serotonin and norepinephrine, calcium channel α 2 -δ ligands (ie, gabapentin and pregabalin), and topical lidocaine were recommended as first-line treatment options on the basis of the results of randomized clinical trials. For subjective sleep measures, clinicians should consider prescribing cabergoline or gabapentin en-acarbil (Level A), or ropinirole, pramipexole, rotigotine, or pregabalin (Level B). For patients failing other treatments for RLS symptoms, clinicians may consider prescribing prolonged-release oxy-codone/naloxone where available (Level C). given careful consideration before being prescribed pregabalin and gabapentin. Treatment should be reviewed regularly. NICE Clinical guideline 173 states “Offer a choice of amitriptyline, duloxetine, gabapentin or pregabalin as initial treatment for neuropathic pain (except trigeminal neuralgia)”. Pregabalin Analgesic Tapering Guidelines for adult patients with persistent pain patients taking strong opioids and/or gabapentinoids. Prescribing of gabapentinoids for neuropathic pain should be reviewed in line with the criteria set out in NICE4 and should be gradually discontinued if ineffective. In contrast, new evidence supporting three alpha-2-delta ligand calcium channel blockers — gabapentin enacarbil, gabapentin, and pregabalin — led the task force to support them as strong recommendations for RLS treatment. Treatment is focused on symptom control and includes topical lidocaine or capsaicin and oral gabapentin, pregabalin, or tricyclic antidepressants. although such prescriptions should follow ant. Treatment should be considered if RLS symptoms interfere with sleep or daytime function to an important degree. Before determining the best treatment, it is important to fi. The National Institute of Clinical Excellence (NICE) guidelines on the management of neuropathic pain recommend gabapentin, pregabalin, amitriptyline or duloxetine as the initial choice of treatment for neuropathic pain with the exception of trigeminal neuralgia. 1 The guideline development group found that gabapentin was the most cost Multidisciplinary conservative care and nonopioid medications (tricyclic antidepressants, serotonin norepinephrine reuptake inhibitors, gabapentanoids, topicals, and transdermal substances) are recommended as firstline therapy; combination therapy (firstline medications) and tramadol and tapentadol are recommended as secondline; serotonin-specif The three systematic reviews summarized in this report examined the efficacy and safety of treatments for patients with any type of neuropathic pain, 8 painful diabetic neuropathy, 9 or fibromyalgia. 10 All the reviews included gabapentin, pregabalin, TCAs, and SNRIs. Most patients who undergo surgical procedures experience acute postoperative pain, but evidence suggests that less than half report adequate postoperative pain relief. Many preoperative, intraoperative, and postoperative interventions and management strategies are available for reducing and managing postoperative pain. The American Pain Society, with input from the American Society of Several other medications have been used in clinical practice to manage muscle cramps, including the anticonvulsants gabapentin (Neurontin), carbamazepine (Tegretol), and oxcarbazepine (Trileptal). It is recommended to start treatment 1 to 2 hours before usual onset of symptoms. Treatment should commence at 300 mg of gabapentin (100 mg in patients older than 65 years) or 75 mg of pregabalin daily (50 mg in patients older than 65 years) and be increased every few days as needed. Guidelines by several professional societies (ASA, ASRA, APS) advocate for perioperative administration of gabapentin as a component of multimodal analgesia. However, recent publications challenge the routine use of gabapentin in the perioperative setting due to a potentially unfavorable ratio of benefit vs. adverse side effects. Gabapentin for Adults with Neuropathic Pain: A Review of the Clinical Evidence and Guidelines [Internet]. Characteristics of evidence-based guidelines. Recommendations from evidence-based guidelines. Copyright © 2014 Canadian Agency for Drugs and Technologies in Health. The 2019 American College of Rheumatology/Arthritis Foundation guidelines reviewed the effectiveness of pharmacologic and nonpharmacologic treatments for OA in the knee, hip, and hand. Graded treatment recommendations can be found in treatment topics for specific chronic pain conditions (eg, chronic back pain, postherpetic neuralgia, fibromyalgia). The general approach to the management of chronic non-cancer pain and nonpharmacologic therapies for chronic pain are discussed separately. Nonpharmacologic treatment options and teratogenicity. Gabapentin (Neurontin) is minimally effective at high doses, and adverse effects are common. This VA/DoD guideline on management of Patients already taking Pregabalin or Gabapentin should be observed for signs of abuse/dependence including drug seeking behaviour, dose escalation or development of tolerance.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |