Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
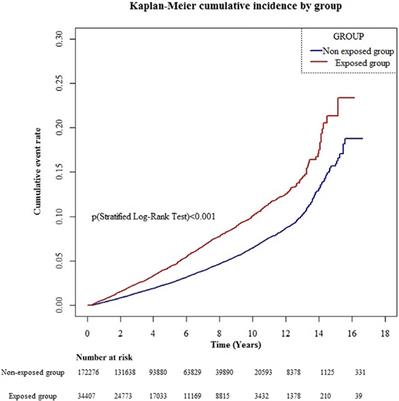 |  |
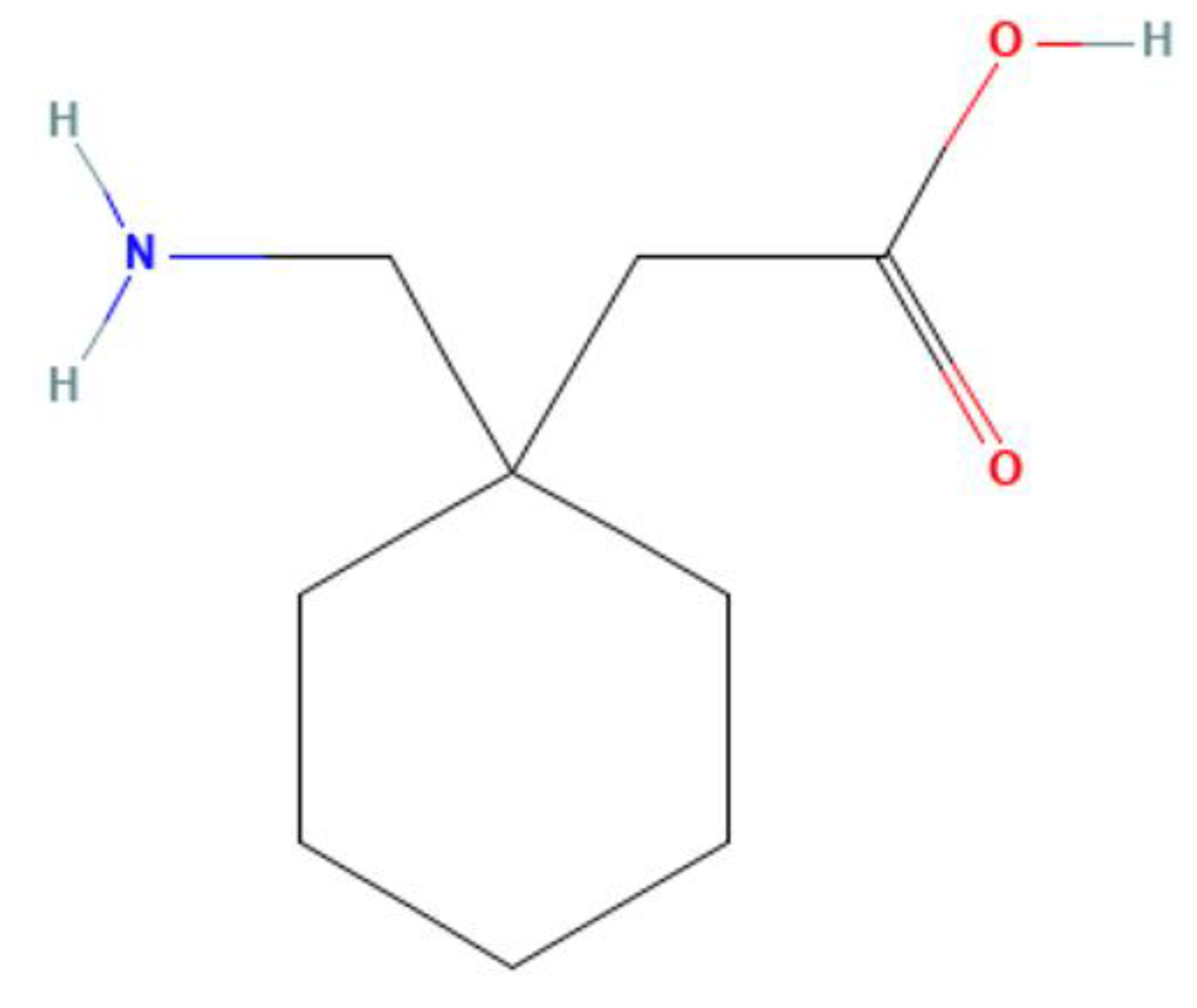
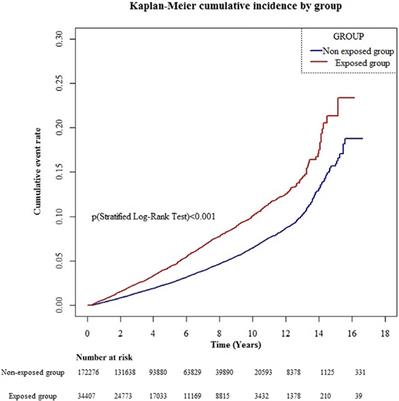
During that time, 800 of them developed dementia. When the researchers examined medication use, they found that people who used anticholinergic drugs were more likely to have developed dementia than those who didn't use them. Moreover, dementia risk increased along with the cumulative dose. We would like to show you a description here but the site won’t allow us. Especially in older adults, gabapentin is prescribed to treat behavioral and psychological symptoms of dementia (BPSD) (Kim et al., 2008). Several studies have reported that gabapentin has a deleterious effect on cognition (Leach et al., 1997; Meador et al., 1999; Shem et al., 2018). Most of the data to guide gabapentin use and dosing in older adults is from pharmacokinetic studies or case reports[1,2] While gabapentin is approved to prevent seizures, most patients take gabapentin for reasons of neuropathic pain (71%) or psychiatric disorders, with bipolar being most common (15%), with an average dose of 975 mg per day The HR (95% CI) of dementia for gabapentin or pregabalin exposure was 1.45 (1.36–1.55) compared to non-exposure group, after adjustment for diabetes mellitus, hypertension, stroke, hyperlipidemia, depression, and head injury. Conclusion: Patients treated with gabapentin or pregabalin had an increased risk of dementia. Therefore, these drugs should be used with caution, particularly in susceptible individuals. Dementia is one of the most prevalent neurodegenerative disorders worldwide. And since treatment options for dementia are limited, prevention is key. Dementia risk is tied to common things like diabetes, high blood pressure, and physical inactivity. But some common medications are associated with dementia risk, too. Here are four common drug classes linked to dementia, and what the research says about your risk. 1. Gabapentin has been administered to several geriatric patients with bipolar disorder and patients with dementia. It has also been reported to be successful in the treatment of a 13-year-old boy with behavioural dyscontrol, a finding that suggested a possible role for gabapentin in the treatment of other behavioural disorders. The adjusted odds ratio for dementia risk associated with gabapentin use was 0.91 (95 % C.I. 0.83–1.01), indicating no substantial increase in risk. Conclusion. The adjusted odds ratio for dementia risk associated with gabapentin use was 0.91 (95 % C.I. 0.83-1.01), indicating no substantial increase in risk. Conclusion: Long-term Gabapentin therapy for chronic pain is not associated with a differential risk of dementia across dosage levels, irrespective of age or gender. The short answer is: yes, emerging evidence suggests that gabapentin, and its close relative pregabalin, may indeed increase the risk of developing dementia, particularly with long-term use and higher cumulative doses. While it’s not a definitive “cause,” studies are highlighting a concerning correlation that warrants further 2.3 Gabapentin use determination. Medication use in the UDS is operationalized via an interview that asks participants to report all medications, including prescriptions and over-the-counter medications, they have used in the 2 weeks preceding their annual study visit. Gabapentin use was defined as any reported use of gabapentin. Gabapentin has been increasingly prescribed to older adults for off-label indications, and accumulating evidence suggests potential for gabapentin misuse and related adverse events. However, the relation between gabapentin initiation and longer-term neurocognitive changes is not well understood. The evidence of gabapentin and dementia is mixed, with two studies looking at hundreds of thousands of people and coming to completely different conclusions. Our study aims to assess whether gabapentin use in chronic pain patients either increases dementia risk or offers protective benefits, using a population-based nested case-control approach. Gabapentin use was significantly associated with decline in cognitive and functional status among older adults with initially normal cognition. Further studies are needed to examine the association. Background: Gabapentin is increasingly prescribed to older adults, which raises concerns about its potential to cause neurocognitive changes. Therefore, we aimed to examine the association of gabapentin use with neurocognitive changes (i.e., cognitive decline, functional status decline, and motor function change) in older adults. However, several case reports in which gabapentin was used for agitation in dementia with Lewy bodies question its appropriateness for all types of dementia-related agitation [14–16]. Indeed, paradoxical gabapentin-induced exacerbation of psychosis in a patient with schizophrenia has already been described [ 17 ]. Objective: Previous studies have shown that gabapentin or pregabalin use is associated with cognitive decline. Herein, we aimed to evaluate the association between gabapentin or pregabalin use and the risk of dementia. Methods: In this retrospective, population-based matched cohort stu We found that the prevalence of concurrent use of gabapentin with antidepressants and antipsychotics was higher in older adults with dementia compared to those with normal cognition.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |