Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 | |
 |  |
 |  |
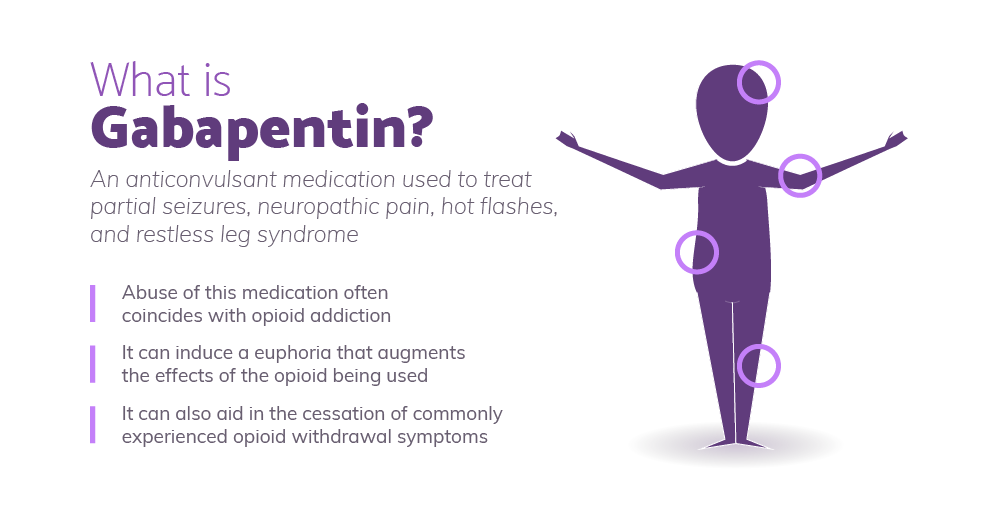 |  |
Citation: Ahmed S, Bachu R, Kotapati P, Adnan M, Ahmed R, Farooq U, Saeed H, Khan AM, Zubair A, Qamar I and Begum G (2019) Use of Gabapentin in the Treatment of Substance Use and Psychiatric Disorders: A Systematic Review. Front. Psychiatry 10:228. doi: 10.3389/fpsyt.2019.00228. Received: 20 November 2018; Accepted: 27 March 2019; Published: 07 Gabapentin is commonly used off-label in the treatment of psychiatric disorders with success, failure, and controversy. A systematic review of the literature was performed to elucidate the evidence for clinical benefit of gabapentin in psychiatric disorders. But since it’s been available, gabapentin has also been used off-label in psychiatry to treat patients with treatment-resistant mood and anxiety disorders as well as alcohol-withdrawal and Study selection and data extraction: The resulting 988 abstracts were read by 2 reviewers; references were excluded if gabapentin was not a study compound or psychiatric symptoms were not studied. The resulting references were subsequently read, reviewed, and analyzed; 219 pertinent to gabapentin use in psychiatric disorders were retained. Gabapentin was not found to be effective over placebo in a comprehensive network meta-analysis of pharmacologic treatments in acute mania . Systematic reviews of gabapentin treatment in psychiatric and/or substance use disorders showed inconclusive evidence for efficacy in BD, but possible efficacy for some anxiety disorders [9, 10]. These Method of research: An extensive literature review was conducted, primarily of articles searchable in PubMed, relating to psychiatric uses, safety, and adverse effects of gabapentin. Results: Evidence supports gabapentin as a treatment for alcohol withdrawal and alcohol use disorder. There is sufficient evidence to consider gabapentin as a The next step was to read all of this article’s references. 2-6 Surprisingly, all 5 references focused on the relationship of gabapentin with the use of opioids or in the treatment of pain, with no mention of the common off-label use of gabapentin in various psychiatric disorders such as anxiety and insomnia. Hence, I embarked on a literature This study examined off-label use of gabapentin for psychiatric indications and its concomitant use with CNS-D prescription drugs in a nationally representative sample of ambulatory care office visits. Less than 1% of outpatient gabapentin use was for FDA-approved indications. There are actions psychiatrists can take to reduce the use of gabapentin: Educate patients: Engaging in open and honest discussions with patients about the risks and benefits of gabapentin is essential. Patients should be made aware of the potential for abuse, dependence, and overdose. Objective: Gabapentin is commonly used off-label in the treatment of psychiatric disorders with success, failure, and controversy. A systematic review of the literature was performed to elucidate the evidence for clinical benefit of gabapentin in psychiatric disorders. GBP has shown to be safe and effective in the treatment of alcohol dependence. However, the literature suggests that GBP is effective as an adjunctive medication rather than a monotherapy. More clinical trials with larger patient populations are needed to support gabapentin's off-label use in psychiatric disorders and substance use disorders. I just started using 300 mg gabapentin (100 mg in morning and 200 mg) in evening). She went to a hospital for seniors with psych. issues and the doctor thre Preclinical data suggest the potential anxiolytic effect of gabapentin ().Recently, Beauclair et al. reported reduction in anxiety symptoms and syndromes in 18 patients with primary psychotic disorders and in one patient with generalized anxiety disorder treated adjunctively with gabapentin, 200–1800 mg/day. High concomitant use of CNS-D drugs and off-label gabapentin for psychiatric diagnoses underlines the need for improved communication about safety. In this nationally representative sample, <1% of outpatient gabapentin use was for approved indications. evidence suggests that gabapentin’s use in psychiatry has de-creased over time, despite renewed interest in its potential for alcohol use disorder, posttraumatic stress disorder (PTSD), and obsessive-compulsive disorder (OCD) (912). Objective: Gabapentin (GBP) is an anticonvulsant medication that is also used to treat restless legs syndrome (RLS) and posttherapeutic neuralgia. GBP is commonly prescribed off-label for psychiatric disorders despite the lack of strong evidence. We conducted a systematic review and meta-analysis of the evidence for three of their common psychiatric uses: bipolar disorder, anxiety, and insomnia. Fifty-five double-blind randomised While gabapentin is frequently used in practice for a wide array of psychiatric diagnoses, its use is evidence-based for only a few indications. Multiple RCTs have shown gabapentin to be ineffective for bipolar disorder. There is insufficient evidence to recommend the use of gabapentin for MDD, GAD, PTSD, or OCD. It is important to note that the use of gabapentin for psychiatric symptoms is not supported by extensive research evidence, and its effectiveness for these purposes is still under investigation. Additionally, gabapentin carries its own set of potential side effects, including dizziness, drowsiness, and difficulty concentrating. Objective: This article reviews evidence-based psychiatric uses of gabapentin, along with associated risks. Method of Research: An extensive literature review was conducted, primarily of articles searchable in PubMed, relating to psychiatric uses, safety, and adverse effects of gabapentin. Results: Evidence supports gabapentin as a treatment for alcohol withdrawal and alcohol use disorder
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 | |
 |  |
 |  |
 |  |