Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
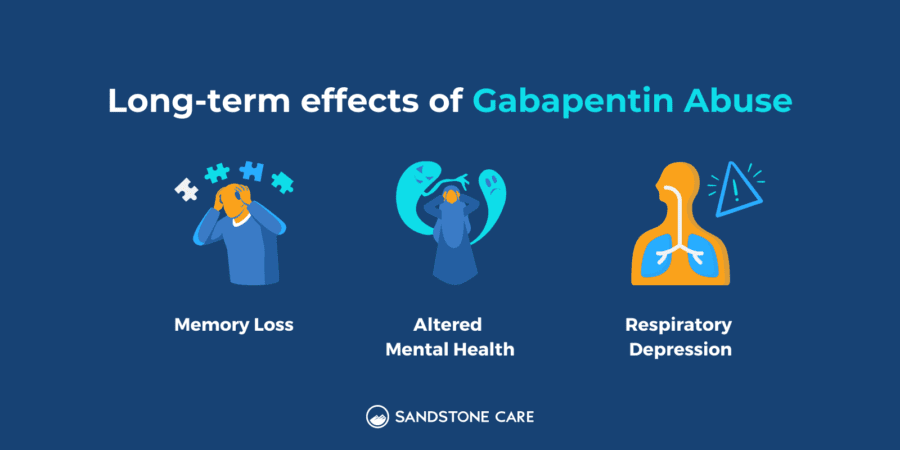
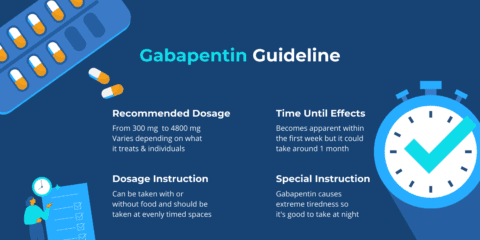
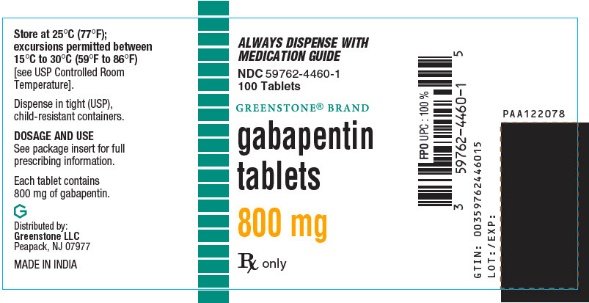
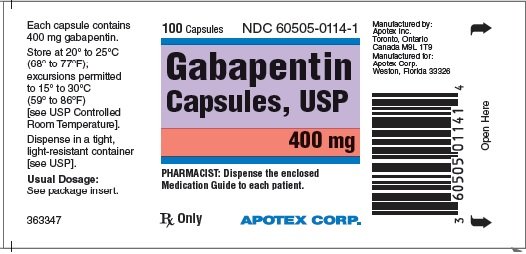
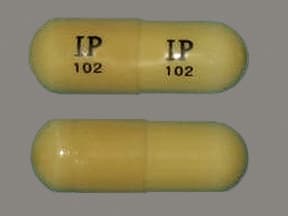
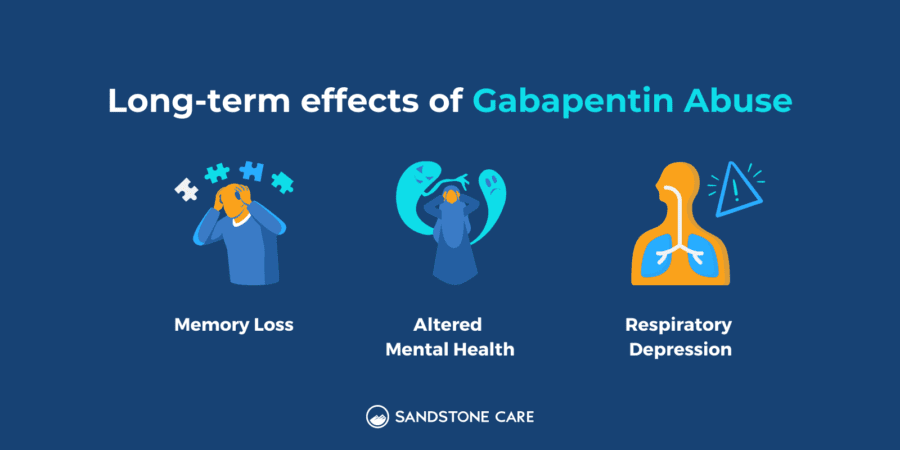
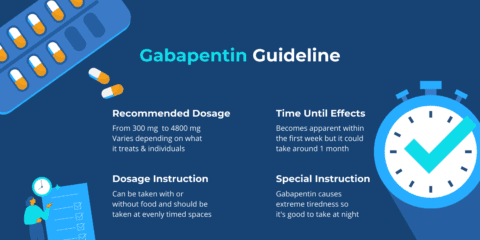
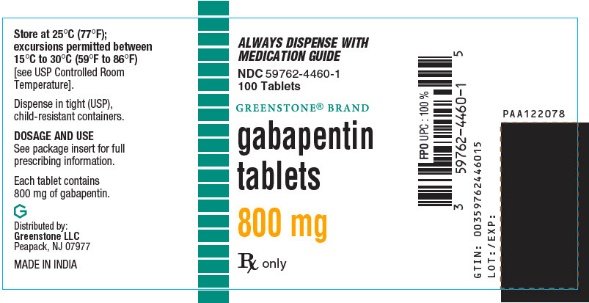
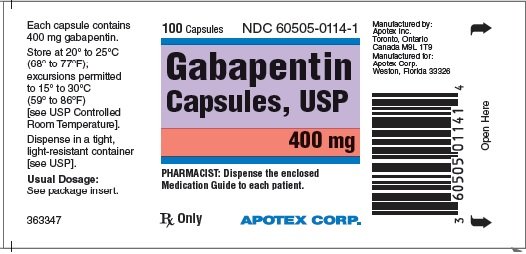
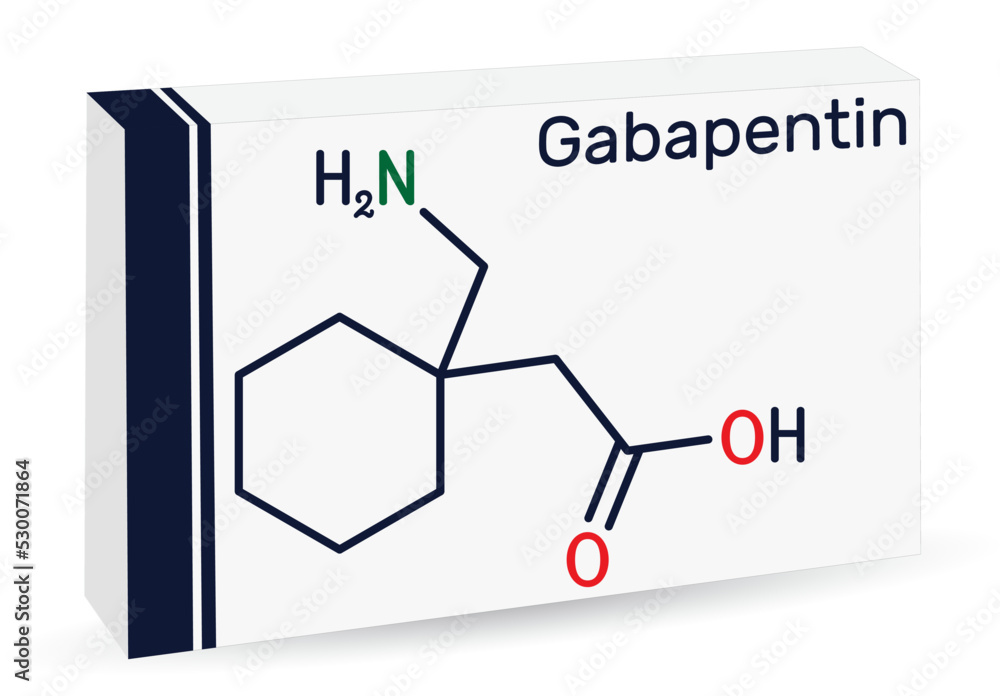
Objective: Gabapentin (GBP) is an anticonvulsant medication that is also used to treat restless legs syndrome (RLS) and posttherapeutic neuralgia. GBP is commonly prescribed off-label for psychiatric disorders despite the lack of strong evidence. G abapentin was originally approved by the US Food and Drug Administration (FDA) for the treatment of partial seizures in 1993, 1,2 with subsequent approval for postherpetic neuralgia in 2002. 3–5 Within a decade of initial FDA approval, gabapentin’s second most common use became off-label prescription for psychiatric disorders. 6 But since it’s been available, gabapentin has also been used off-label in psychiatry to treat patients with treatment-resistant mood and anxiety disorders as well as alcohol-withdrawal and post Gabapentin, known by its brand name Neurontin, has been turning heads in the psychiatric community for its potential to address a wide range of mental health issues. But how did this anticonvulsant drug find its way into the realm of mental health treatment? Gabapentin, also known as Gralise and Neurontin, is an anticonvulsant medication typically used in the treatment of epilepsy, along with various other physical and mental health treatments. Always use this medication exactly as prescribed and consult with your doctor prior to starting any other medications (prescribed or over the counter) while High concomitant use of CNS-D drugs and off-label gabapentin for psychiatric diagnoses underlines the need for improved communication about safety. In this nationally representative sample, <1% of outpatient gabapentin use was for approved indications. Objective: Gabapentin is commonly used off-label in the treatment of psychiatric disorders with success, failure, and controversy. A systematic review of the literature was performed to elucidate the evidence for clinical benefit of gabapentin in psychiatric disorders. Preclinical data suggest the potential anxiolytic effect of gabapentin ().Recently, Beauclair et al. reported reduction in anxiety symptoms and syndromes in 18 patients with primary psychotic disorders and in one patient with generalized anxiety disorder treated adjunctively with gabapentin, 200–1800 mg/day. We conducted a systematic review and meta-analysis of the evidence for three of their common psychiatric uses: bipolar disorder, anxiety, and insomnia. Fifty-five double-blind randomised Objective: This article reviews evidence-based psychiatric uses of gabapentin, along with associated risks. Method of Research: An extensive literature review was conducted, primarily of articles searchable in PubMed, relating to psychiatric uses, safety, and adverse effects of gabapentin. evidence suggests that gabapentin’s use in psychiatry has de-creased over time, despite renewed interest in its potential for alcohol use disorder, posttraumatic stress disorder (PTSD), and obsessive-compulsive disorder (OCD) (912). Apart from its use in bipolar disorder, gabapentin has been used in patients with anxiety, panic disorder, social phobia, aggressive behavior, and posttraumatic stress disorder (PTSD). 15–21 Gabapentin has also been used in treating obsessive-compulsive disorder. 15,22,23 Other areas of clinical use have been in the treatment of substance abuse Gabapentin is commonly used off-label in the treatment of psychiatric disorders with success, failure, and controversy. A systematic review of the literature was performed to elucidate the evidence for clinical benefit of gabapentin in psychiatric disorders. The rise in gabapentin prescribing is multifactorial but thought to be due in part to efforts by the pharmaceutical industry to promote the use of the medication for off-label uses. (In 2004, the manufacturer of Neurontin, Pfizer, pleaded guilty to multiple counts of illegally promoting the off-label use of gabapentin, resulting in nearly $430 While gabapentin is frequently used in practice for a wide array of psychiatric diagnoses, its use is evidence-based for only a few indications. Multiple RCTs have shown gabapentin to be ineffective for bipolar disorder. There is insufficient evidence to recommend the use of gabapentin for MDD, GAD, PTSD, or OCD. This study examined off-label use of gabapentin for psychiatric indications and its concomitant use with CNS-D prescription drugs in a nationally representative sample of ambulatory care office visits. Less than 1% of outpatient gabapentin use was for FDA-approved indications. GBP has shown to be safe and effective in the treatment of alcohol dependence. However, the literature suggests that GBP is effective as an adjunctive medication rather than a monotherapy. More clinical trials with larger patient populations are needed to support gabapentin’s off-label use in psychiatric disorders and substance use disorders. gabapentin treatment mania or hypomania occurred, ad-verse events, maximum and maintenance gabapentin dose and duration of treatment, indications for treatment with gabapentin, whether or not gabapentin was discon-tinued, reason for discontinuation of gabapentin, family history of psychiatric disorders, age at onset of illness, The next step was to read all of this article’s references. 2-6 Surprisingly, all 5 references focused on the relationship of gabapentin with the use of opioids or in the treatment of pain, with no mention of the common off-label use of gabapentin in various psychiatric disorders such as anxiety and insomnia. Hence, I embarked on a literature Abstract. Objective: This article reviews evidence-based psychiatric uses of gabapentin, along with associated risks. Method of Research: An extensive literature review was conducted, primarily of articles searchable in PubMed, relating to psychiatric uses, safety, and adverse effects of gabapentin.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |