Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
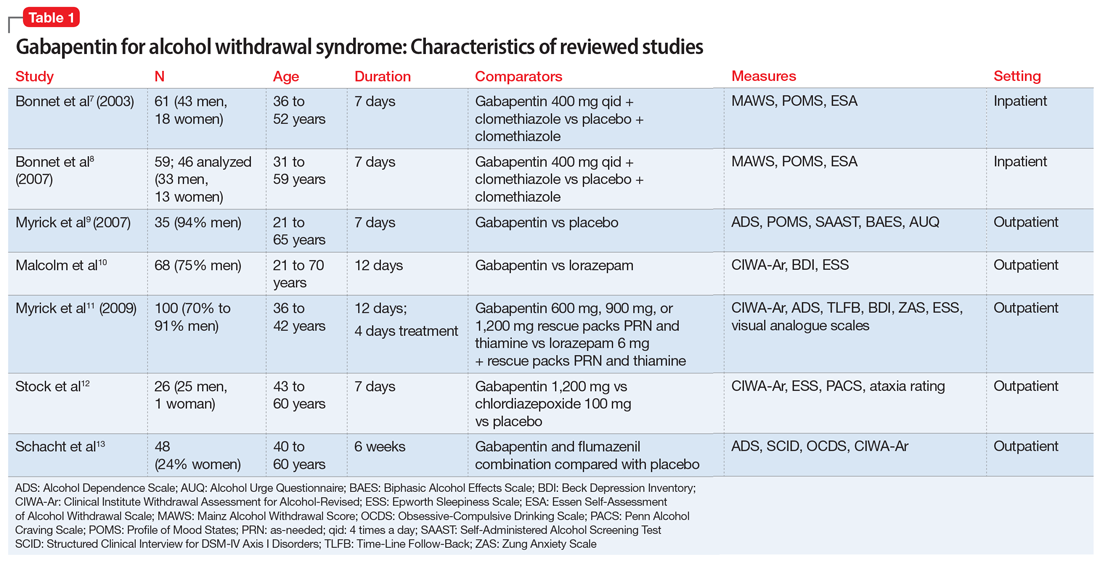
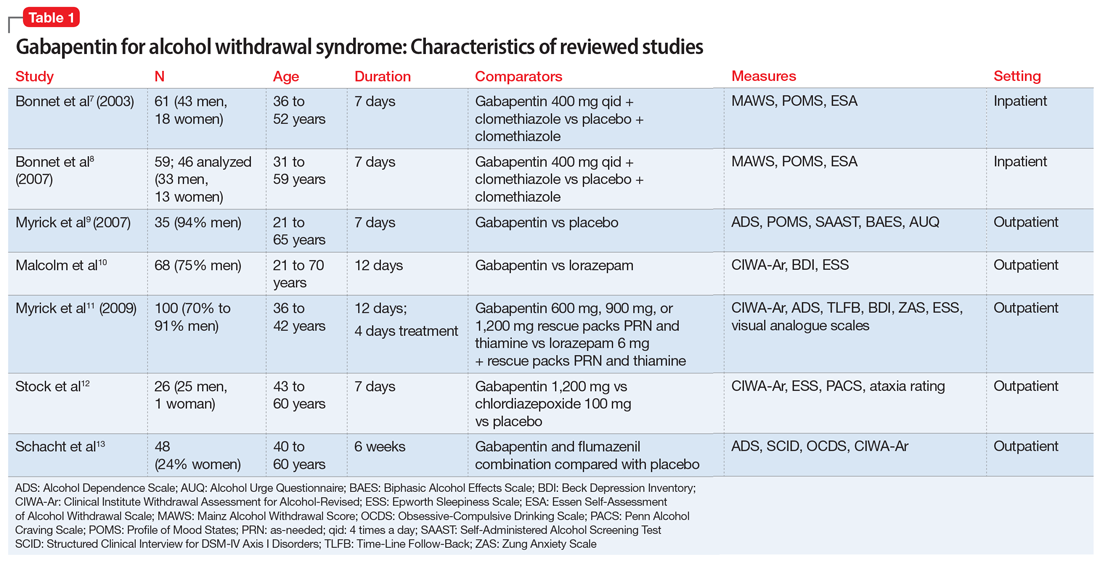
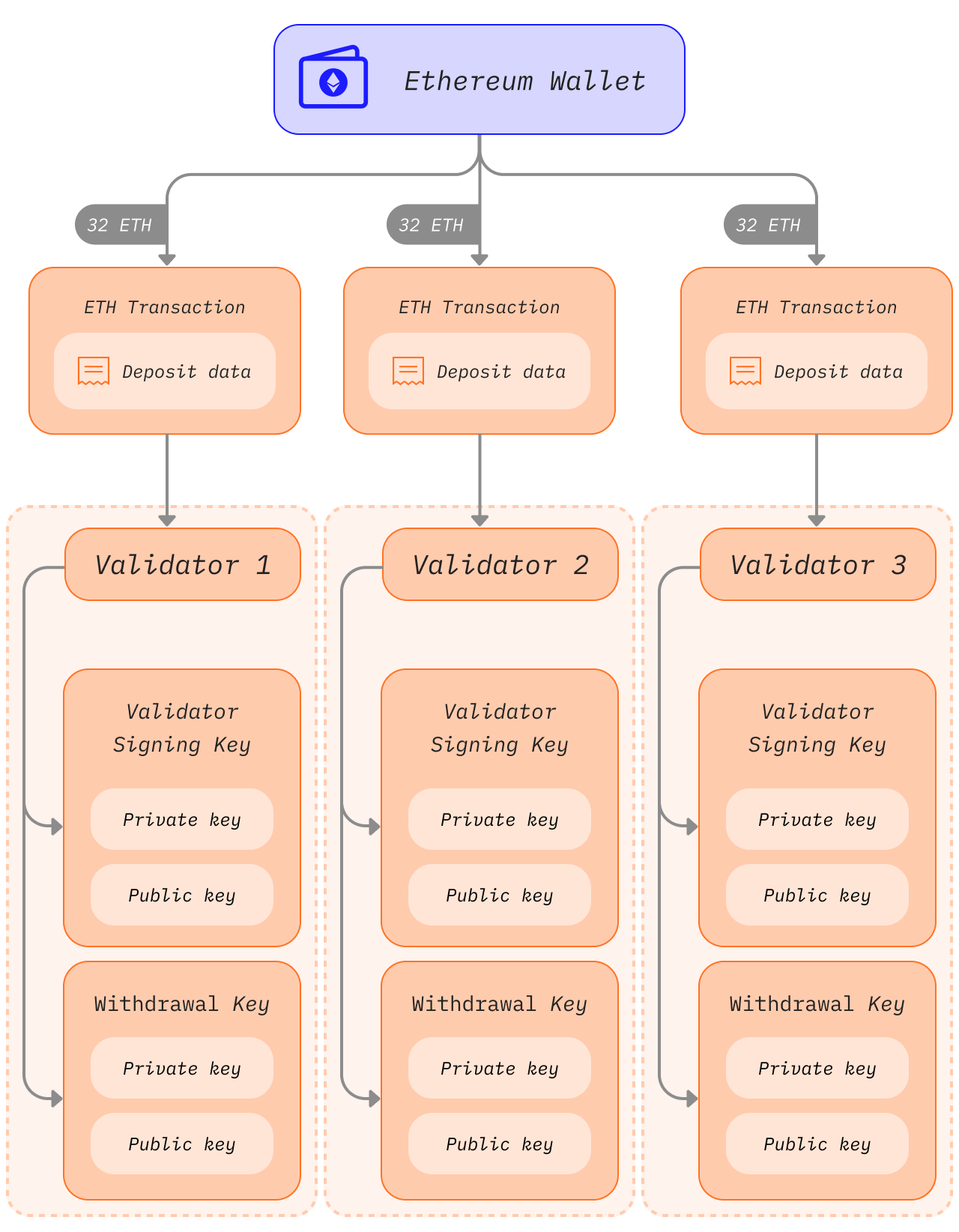
Objective: The current meta-analysis synthesizes previous findings on the effect of gabapentin on alcohol withdrawal and craving. Data sources: Using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) methodology, a search for relevant English-language literature published between January 1999 and February 2019 was conducted using PubMed and Google Scholar with the Past reports have suggested that some withdrawal symptoms can present after 1-2 days upon abrupt discontinuation of gabapentin after chronic use within young to middle-aged patients. These symptoms mimic that of alcohol and benzodiazepine withdrawal purportedly due to a similar mechanism of action. Medicines associated with dependence include benzodiazepines, Z-drugs (such as zopiclone and zolpidem), opioids, gabapentin and pregabalin. Antidepressants, although historically not classified as dependence-forming medicines, can nevertheless cause withdrawal symptoms when they are stopped. Evidence supports gabapentin as a treatment for alcohol withdrawal and alcohol use disorder. There is sufficient evidence to consider gabapentin as a third-line treatment for social anxiety disorder and severe panic disorder. Gabapentin withdrawal: case report in an older adult and review of the literature J Am Geriatr Soc. 2013 Sep;61(9):1635-7. doi: 10.1111/jgs.12427. A patient developed apparent withdrawal symptoms beginning two days after gabapentin therapy was discontinued. The symptoms were unresponsive to treatment with benzodiazepines but completely resolved with the reinitiation of gabapentin therapy. Gabapentin, or Neurontin, is a prescription drug used primarily to treat epilepsy patients. There are also cases in which this drug, categorized as an anticonvulsant medicine, is administered as an initial treatment to provide relief for patients suffering from health conditions like neuropathic pain, such as diabetic neuropathy, central neuropathic pain, and post-herpetic neuralgia. Specific to opioids, small clinical studies have shown that individuals receiving gabapentin reported decreased symptoms of withdrawal; gabapentin works well in combination with methadone for opioid detoxification; and patients treated with gabapentin report decreased probability of positive urine tests for opioids over time compared to placebo Using electronic records from a large inpatient psychiatric facility, a retrospective study of 172 patients presenting with benzodiazepine withdrawal was conducted to determine if the coincidental use of gabapentin for other medical conditions was associated with better outcomes of benzodiazepine withdrawal (N=57 gabapentin, N=115 no gabapentin). The prestudy high-alcohol withdrawal group had positive gabapentin effects on no heavy drinking days (P < .02; NNT, 3.1) and total abstinence (P = .003; NNT, 2.7) compared with placebo, while within the low-alcohol withdrawal group, there were no significant differences. Gabapentin: Gabapentin is indicated for postherpetic neuralgia and serves as adjunctive therapy for managing partial seizures (with or without secondary generalization) in adults and pediatric patients aged 3 or older. Gabapentin (GBP) attenuates THC withdrawal-depressed progressive-ratio (PR) performance. Mice were trained on a PR 2 schedule of reinforcement. (A) Acute GBP (10 and 50 mg/kg, i.p.) dose-dependently increased break point (* p < .05 vs. 0 mg/kg). Since its market release, gabapentin has been presumed to have no abuse potential and subsequently has been prescribed widely off-label, despite increasing reports of gabapentin misuse. This review estimates and describes the prevalence and effects of, motivations behind, and risk factors for gabapentin misuse, abuse, and diversion. Gabapentin has been widely used to manage post-herpetic neuralgia, peripheral neuropathy, seizure disorders, alcohol use disorder (AUD), alcohol withdrawal, and insomnia. Although usually well tolerated, gabapentin has been reported to cause severe physiologic dependence and withdrawal. Gabapentin (GBP) has gained wide acceptance in the treatment of pain, migraine, bipolar illness, and epilepsy. It has a relatively benign side effect profile, lacks significant drug interactions, is not liver metabolized, and is renally excreted. Herein three cases are presented that demonstrate wit On average, the patients were taking more than 3000 mg/d (600-8000 mg/d). Two surveys reported that the misuse of gabapentin was 1.1% in the general population and 22% in drug abuse treatment centers. Withdrawal, when reported, occurred within 12 hours to 7 days of discontinuation of the medication. Relative to placebo, gabapentin significantly reduced cannabis use as measured both by urine toxicology (p=0.001) and by the Timeline Followback Interview (p=0.004), and significantly decreased withdrawal symptoms as measured by the Marijuana Withdrawal Checklist (p<0.001). Gabapentin was also associated with significantly greater improvement We aimed to evaluate the effectiveness of gabapentin as a benzodiazepine-sparing agent in patients undergoing alcohol withdrawal treatment in all the hospitals of a large tertiary healthcare system. Nevertheless, from a mechanistic point of view, there is rationale to support the use of gabapentin during acute alcohol withdrawal. Gabapentin has been found to potentiate CNS GABA in humans (Petroff et al., 1996), inhibit glutamate synthesis, modulate calcium current, inhibit sodium channels, and reduce norepinephrine and dopamine release A 2014 systematic review of anticonvulsants for alcohol dependence found gabapentin was not effective, though very few people were taking gabapentinoids, so conclusions were not possible. 22 In a 2020 small double-blind, placebo-controlled RCT over 16 weeks, gabapentin 1200 mg daily effectively promoted abstinence and prevented return to heavy
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |