Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 | |
 |  |
 |  |
 |  |
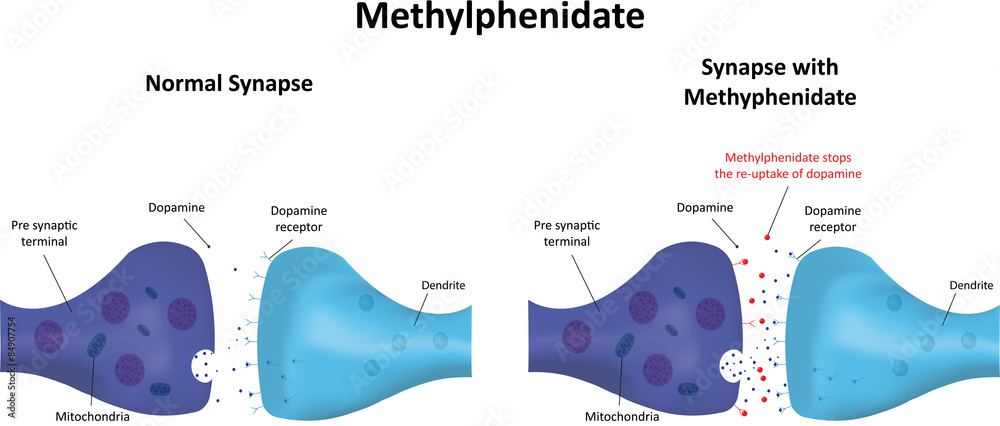
Sudden cessation of baclofen or phenibut after chronic use can manifest a life-threatening withdrawal syndrome that requires aggressive treatment. This topic will discuss the evaluation and management of baclofen and phenibut poisoning and withdrawal. A summary table to facilitate emergency management is provided . The therapeutic use of As an example, in a meta-analyses of treatment for alcohol use disorder, treatment with oral naltrexone 50 mg, as compared with placebo, was associated with decreased return to any drinking (16 trials, n = 2347; relative risk 0.93, 95% CI 0.87-0.99), decreased return to heavy drinking (23 trials, n = 3170; relative risk 0.81, 95% CI 0.72-0.9 The ambulatory management of mild alcohol withdrawal, the initial diagnosis and treatment of alcohol use disorder, and specific conditions due to alcohol-related organ damage (eg, cirrhosis, pancreatitis) are discussed separately. These medications can cause lethargy or agitation in overdose, increase risk of death combined with opioids, and manifest a withdrawal syndrome. This topic will discuss the evaluation and management of gabapentinoid poisoning and withdrawal. Evidence supports gabapentin as a treatment for alcohol withdrawal and alcohol use disorder. There is sufficient evidence to consider gabapentin as a third-line treatment for social anxiety disorder and severe panic disorder. Withdrawal effects are more likely where someone is on high dose gabapentinoid or has been taken for more than 6 weeks. Where a gabapentinoid has to be discontinued due to medical reasons it is recommended this should be done gradually over a minimum of 1 week independent of the indication3. The goals of medically supervised withdrawal are to alleviate withdrawal symptoms, prevent worsening symptoms, and to prepare the individual for transition to the maintenance phase of treatment (ie, treatment of alcohol use disorder). Gabapentin and pregabalin are commonly prescribed medications for the treatment of seizure disorders, neuropathic pain (eg, postherpetic neuralgia), fibromyalgia, anxiety, post-traumatic stress disorder, and restless leg syndrome. Gabapentinoids are commonly ingested in self-harm attempts and often misused for their sedative and euphoric The epidemiology, pathogenesis, clinical manifestations, course, assessment, diagnosis, and treatment of cannabis withdrawal are reviewed here. Other aspects of cannabis use are discussed separately. (See "Cannabis use disorder: Clinical features, screening, diagnosis, and treatment".) Gabapentin withdrawal can begin within 12 hours and last up to 7 days. As of 2023, the U.S. Drug Enforcement Administration (DEA) has not classified gabapentin as a controlled substance because experts have always believed it showed little potential for abuse or dependence. We report on the use of the anticonvulsant gabapentin in the treatment of alcohol withdrawal in six patients. Patients were initially assessed for need of emergent inpatient detoxification on the basis of evidence from an intensive history and physical examination. Graded treatment recommendations can be found in treatment topics for specific chronic pain conditions (eg, chronic back pain, postherpetic neuralgia, fibromyalgia). The general approach to the management of chronic non-cancer pain and nonpharmacologic therapies for chronic pain are discussed separately. Gabapentin and pregabalin are commonly prescribed medications for the treatment of seizure disorders, neuropathic pain (eg, postherpetic neuralgia), fibromyalgia, anxiety, post-traumatic stress disorder, and restless leg syndrome. Gabapentinoids are commonly ingested in self-harm attempts and often misused for their sedative and euphoric We hypothesized that patients treated with fixed-dose gabapentin taper would experience shorter clinically significant alcohol withdrawal with equivalent safety compared with those treated with CIWA-triggered benzodiazepines. UpToDate The treatment approach to PLMD is similar to that of RLS, although supported by considerably less data. (See 'Periodic limb movement disorder' below.) The selection of therapy depends upon a number of factors, including disease severity, patient age, comorbidities (eg, pain, depression, anxiety, history of impulse control disorders), drug side Gabapentin’s anxiolytic and sedative properties along with its overall safety profile suggest that it may be a viable adjuvant to lorazepam in the management of acute alcohol withdrawal. This case highlights the need for patient-centered slow tapers in patients with severe gabapentin dependence and withdrawal. We present a 32-year-old female effectively treated for AUD with 1,200 mg daily dose of gabapentin, who developed gabapentin dependence and severe withdrawal. Graded treatment recommendations can be found in treatment topics for specific chronic pain conditions (eg, chronic back pain, postherpetic neuralgia, fibromyalgia). The general approach to the management of chronic non-cancer pain and nonpharmacologic therapies for chronic pain are discussed separately. The evaluation and management of benzodiazepine and other substance use disorders (see "Benzodiazepine use disorder" and "Substance use disorders: Clinical assessment" and "Substance use disorder in adolescents: Treatment overview") Withdrawal syndromes from other agents with sedative properties (see "Management of moderate and severe alcohol
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 | |
 |  |
 |  |
 |  |