Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
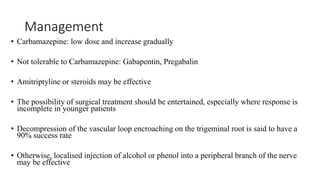
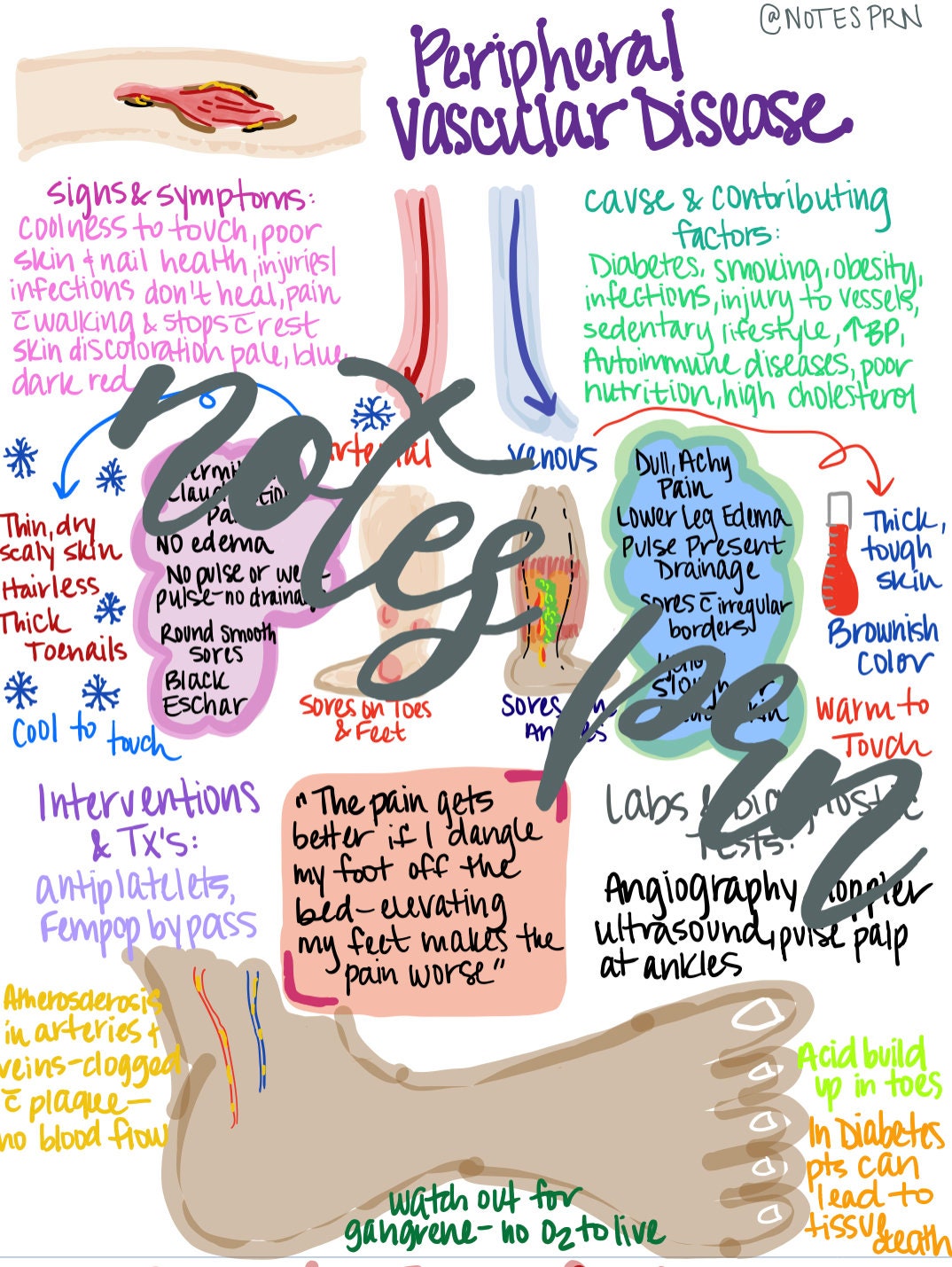
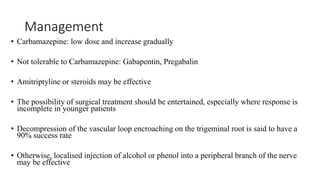
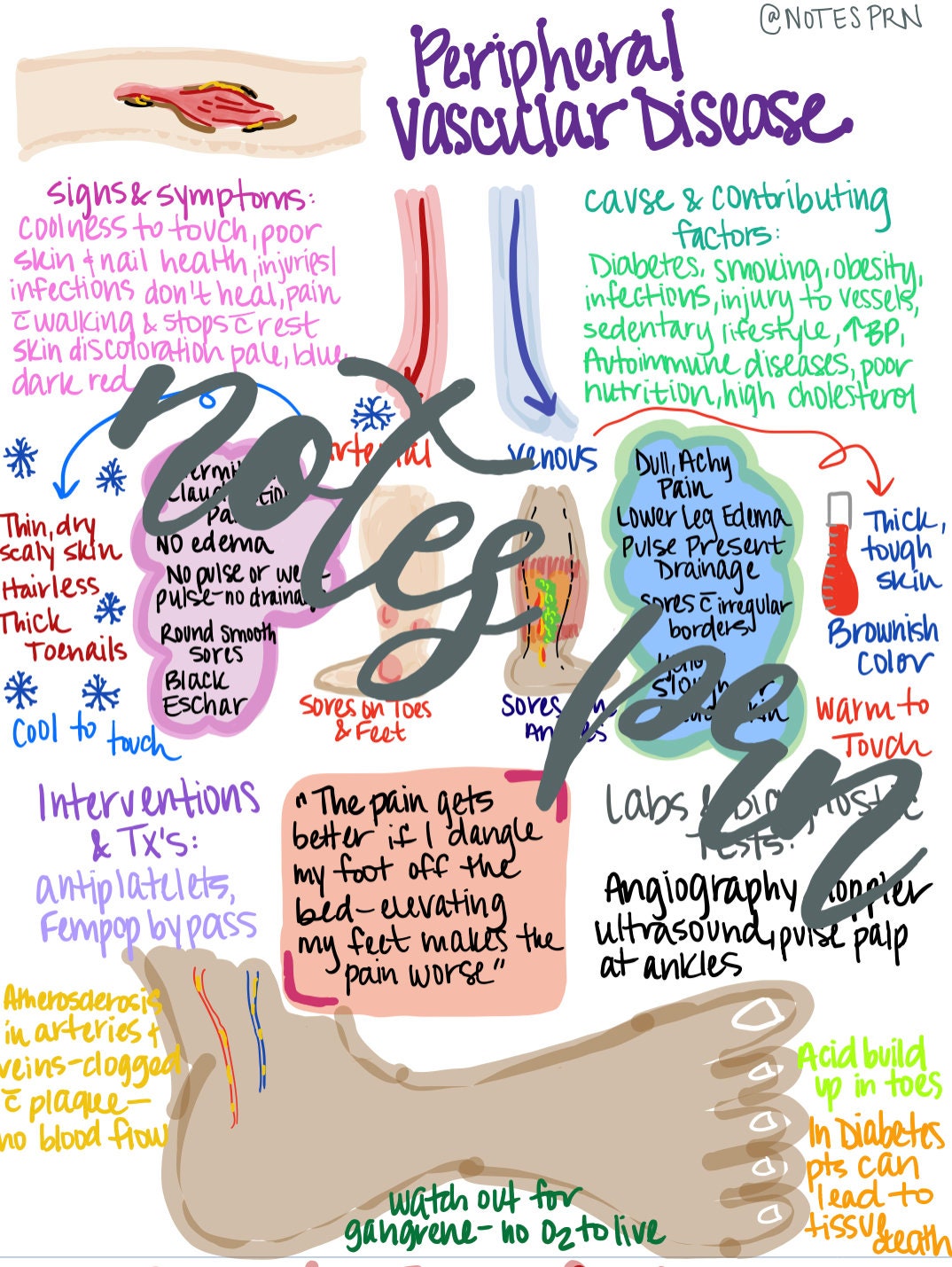
Gabapentin is a medication primarily used for nerve pain and seizures, but its effectiveness in treating peripheral vascular disease (PVD/PAD) is unclear. While some individuals may report trying gabapentin for PVD/PAD, the data suggests it is not a highly effective treatment option. Other conditions that have similar sleep-related leg symptoms include restless legs syndrome (RLS), periodic limb movements, peripheral artery disease (PAD), and neuropathy. RLS may also cause pain, but the discomfort is more continuous and is an unpleasant or uncomfortable deep sensation with a strong need to move the legs during periods of In patients with diabetic neuropathy who were prescribed gabapentin and pregabalin, there is an increased risk for heart failure, myocardial infarction, peripheral vascular disease, stroke, deep venous thrombosis, and pulmonary embolism with long-term use. Gabapentinoids can cause concentration-dependent peripheral edema of early onset. The primary mechanism of non-cardiogenic peripheral edema is vasodilatory edema secondary to altered myogenic tone, independent of Ca<sub>v</sub>1.2 blockade under the experimental conditions tested. Gabapentinoids are widely prescribed off-label for pain management in PAD patients. Effects of gabapentinoid on the outcomes of vascular surgery have not been explored. Preoperative use of gabapentinoids is associated with prolonged hospital stay. Surgeons should consider the association of gabapentinoids use with hospital stay. Patients prescribed gabapentin repeatedly were at a higher 5-year risk of peripheral vascular disease, heart failure, and myocardial infarction. Although other adverse cardiovascular events showed no significant associations in the 5-year follow-up, there was an increased trend in patients prescribed gabapentinoids. Patients prescribed gabapentin repeatedly were at a higher 5-year risk of peripheral vascular disease, heart failure, and myocardial infarction. Although other adverse cardiovascular events showed no significant associations in the 5-year follow-up, there was an increased trend in patients prescribed gabapentinoids. No studies have so far evaluated the role of gabapentin in patients with peripheral vascular disease and there is only a single case report documenting its use. 10 The aim of this study was to prospectively evaluate the clinical effects in terms of visual analogue pain scores in a pilot study of patients with CLI who were on high dose opioid Risk factor control, using diet and lifestyle modification, exercise, and pharmacological methods, improves symptoms and reduces associated cardiovascular events in these patients. Antiplatelet agents and anticoagulants may be used to reduce the incidence of acute events related to thrombosis. Once a patient is diagnosed with claudication due to peripheral artery disease (PAD), the approach to treatment needs to account for the severity of symptoms, the patient's daily activities and limitations, their age and medical comorbidities, location and extent of disease, and their socioeconomic circumstances . In patients with diabetic neuropathy who were prescribed gabapentin and pregabalin, there is an increased risk for heart failure, myocardial infarction, peripheral vascular disease, stroke, deep venous thrombosis, and pulmonary embolism with long-term use. Our findings suggest that increased risk fo ACC/AHA 2005 practice guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular These medications are used to reduce your risk of developing more serious peripheral vascular disease. They also help address any underlying issues caused by PAD, including high blood pressure There were significant associations between short-term (3 month) gabapentin use and heart failure, myocardial infarction, peripheral vascular disease, deep venous thrombosis, and pulmonary embolism. Short-term (3 month) pregabalin use was associated with deep venous thrombosis, peripheral vascular disease. Gabapentin and pregabalin can cause fluid retention, which is hypothesized to be associated with cardiovascular diseases. However, whether long-term use of gabapentin and pregabalin is In patients prescribed pregabalin, the highest risk was observed for deep venous thrombosis (HR: 1.57, 95% CI 1.31–1.88), followed by peripheral vascular disease (HR: 1.35, 95% CI 1.22–1.49), myocardial infarction (HR: 1.29, 95% CI 1.13–1.47), pulmonary embolism (HR: 1.28, 95% CI 1.04– 1.59), stroke (HR: 1.26, 95% CI 1.12–1.42), and heart failur Pre-emptive analgesic strategies may reduce the emergence of chronic pain states in patients with severe peripheral vascular disease. Gabapentin (GBP), a GABA analogue, is primarily used as an anticonvulsant for the treatment of partial seizures and neuropathic pain. Whereas a majority of the side effects are associated with the nervous system, emerging evidence suggests there is a high risk of heart diseases in patients taking GBP. Gabapentin and pregabalin are common treatments to manage fibromyalgia-related pain. Our recent study showed the risk of adverse cardiovascular events increased in diabetic neuropathy patients who were prescribed gabapentin or pregabalin. Peripheral vascular disease is also called peripheral arterial disease (PAD). What causes peripheral vascular disease? The most common cause of PVD is atherosclerosis. This is the buildup of plaque inside the artery wall. Plaque reduces the amount of blood flow to the limbs. It decreases the oxygen and nutrients sent to the tissue.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |