Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
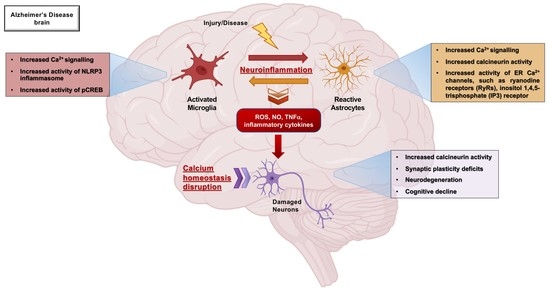
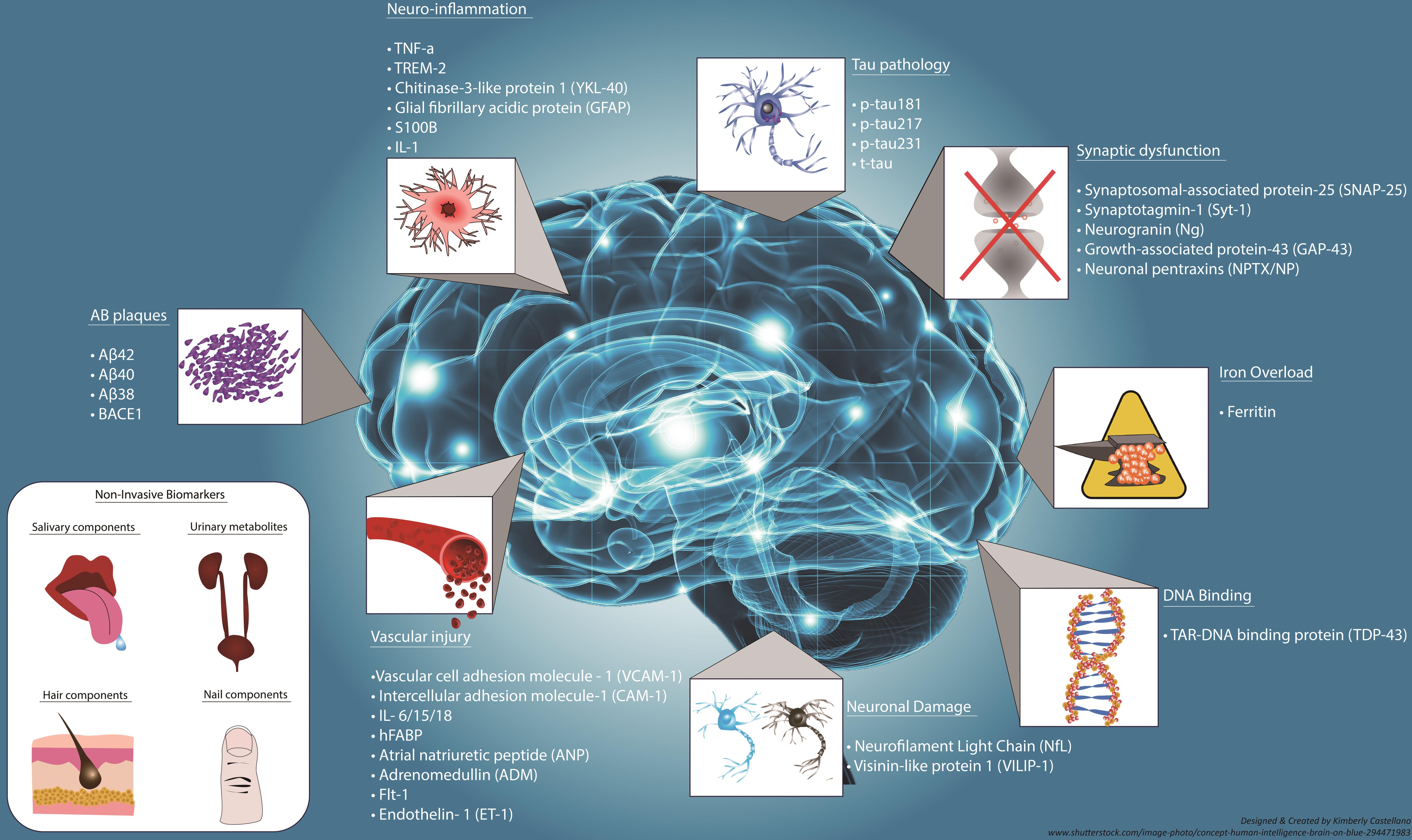
We would like to show you a description here but the site won’t allow us. Gabapentin use was significantly associated with decline in cognitive and functional status among older adults with initially normal cognition. Further studies are needed to examine the association. The remaining nine papers were solely reviews, of which two were described as systematic but predated PRISMA guidelines. Preliminary low-grade evidence based on case series and case reviews suggests possible benefit of gabapentin and pregabalin in patients with BPSD in Alzheimer's disease. Background: Gabapentin is increasingly prescribed to older adults, which raises concerns about its potential to cause neurocognitive changes. Therefore, we aimed to examine the association of gabapentin use with neurocognitive changes (i.e., cognitive decline, functional status decline, and motor function change) in older adults. Gabapentin has been administered to several geriatric patients with bipolar disorder and patients with dementia. It has also been reported to be successful in the treatment of a 13-year-old boy with behavioural dyscontrol, a finding that suggested a possible role for gabapentin in the treatment of other behavioural disorders. Especially in older adults, gabapentin and pregabalin are prescribed to treat behavioral and psychological symptoms of dementia (BPSD). A systematic review analyzing 24 relevant articles found that the use of gabapentinoid agents significantly decreased BPSD in patients with Alzheimer’s disease, suggesting a possible benefit. Gabapentin, an anticonvulsant that appears to have a unique mechanism of antiseizure activity, is another drug that has been considered for the treatment of agitation in dementia. From the eligible sample (≥age 65 years), we identified cognitively normal new-users of gabapentin and the visit they initiated gabapentin (i.e., index visit). Initiators were matched to randomly selected nonusers on year of UDS enrollment and visit number from enrollment to index. Cooney et al. reported seven patients who had behavioural problems subsequent to vascular dementia mixed with Alzheimer disease. A low dose of gabapentin was used (100–200 mg twice daily). There was improvement measured by nursing report. No adverse effects were reported 63. The authors describe the use of gabapentin in the treatment of 4 outpatients with dementia-associated agitation. On the basis of clinical case reports and the Overt Agitation Severity Scale, all 4 patients had reduced agitation with gabapentin. Three of 4 patients were successfully titrated to a full dose of 2,400mg/day. These findings suggest a possible role for gabapentin in the behavioral Objective: Previous studies have shown that gabapentin or pregabalin use is associated with cognitive decline. Herein, we aimed to evaluate the association between gabapentin or pregabalin use and the risk of dementia. Methods: In this retrospective, population-based matched cohort stu Our patient, a 77-year-old Czech woman with incipient vascular dementia, received gabapentin 400mg at bedtime for 6 months and showed convincing improvement. Gabapentin was very effective in treating nocturnal agitation. Keywords: gabapentin, sleep, nocturnal agitation. Gabapentin, commonly prescribed for chronic pain, particularly neuropathic pain, has both analgesic properties (Chincholkar, 2018) and potential neuroprotective benefits (Yan et al., 2019). Its role in the relationship between chronic pain and cognitive outcomes, including dementia, is of growing interest. Gabapentin has been increasingly prescribed to older adults for off-label indications, and accumulating evidence suggests potential for gabapentin misuse and related adverse events. However, the relation between gabapentin initiation and longer-term neurocognitive changes is not well understood. The National Alzheimer’s Coordinating Center (NACC) Database: an Alzheimer disease database. Alzheimer Dis Assoc Disord. 2004;18(4):270–277. [Google Scholar] 22. Morris JC, Weintraub S, Chui HC, et al. The Uniform Data Set (UDS): clinical and cognitive variables and descriptive data from Alzheimer Disease Centers. The researchers relied on a database maintained by the Quebec health insurance program. From it, they identified nearly 2,000 men and women over age 66 who had been diagnosed with Alzheimer's disease. They randomly selected more than 7,000 others without Alzheimer's who were matched for age and sex to those with the disease.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |