Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
/lung-pain-symptoms-causes-and-diagnosis-2249389_2-5b854d75c9e77c005076c14a-5b85d1ddc9e77c002c6e365f.png) | 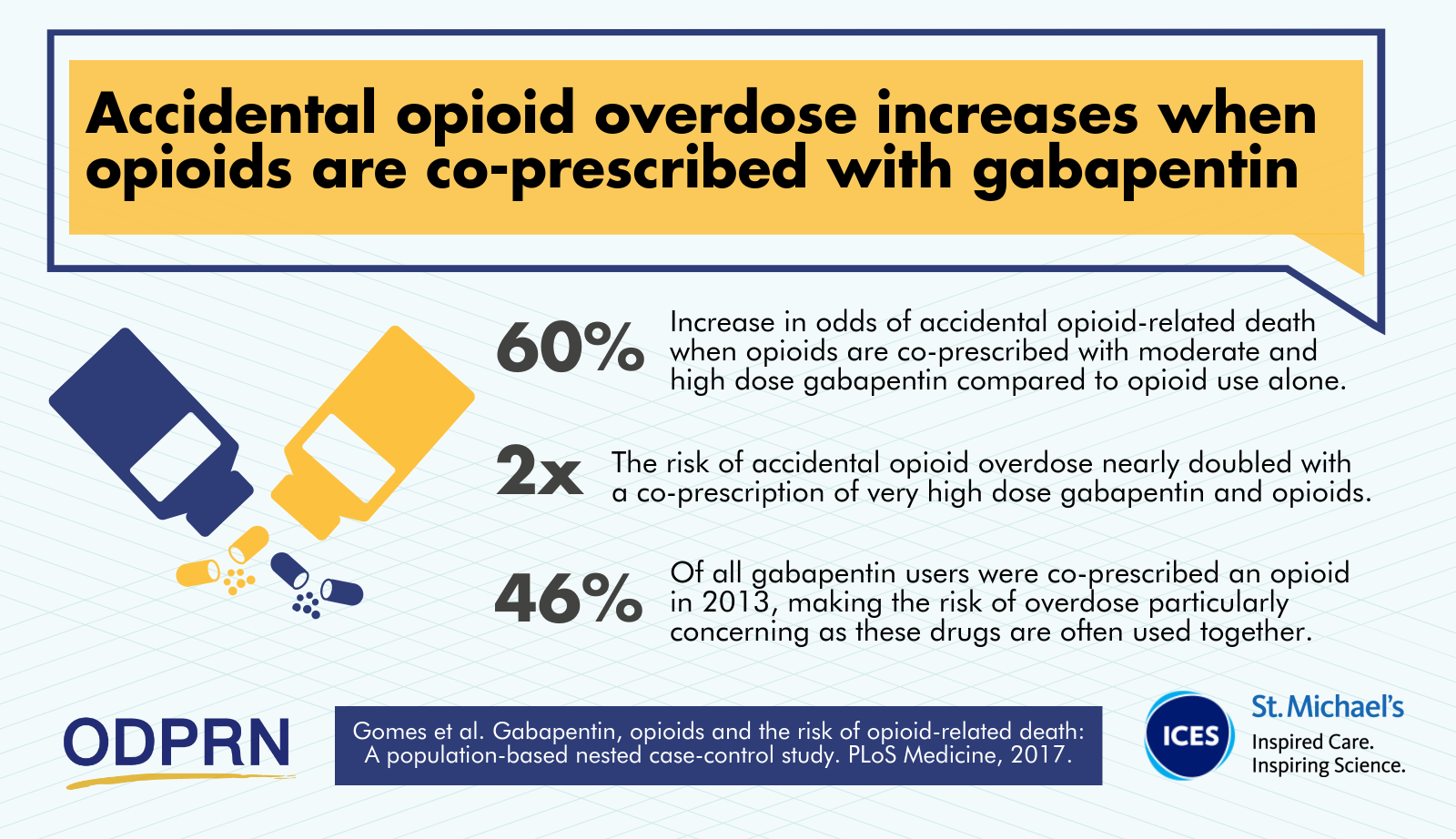 |
 | |
 |  |
 | |
 |  |
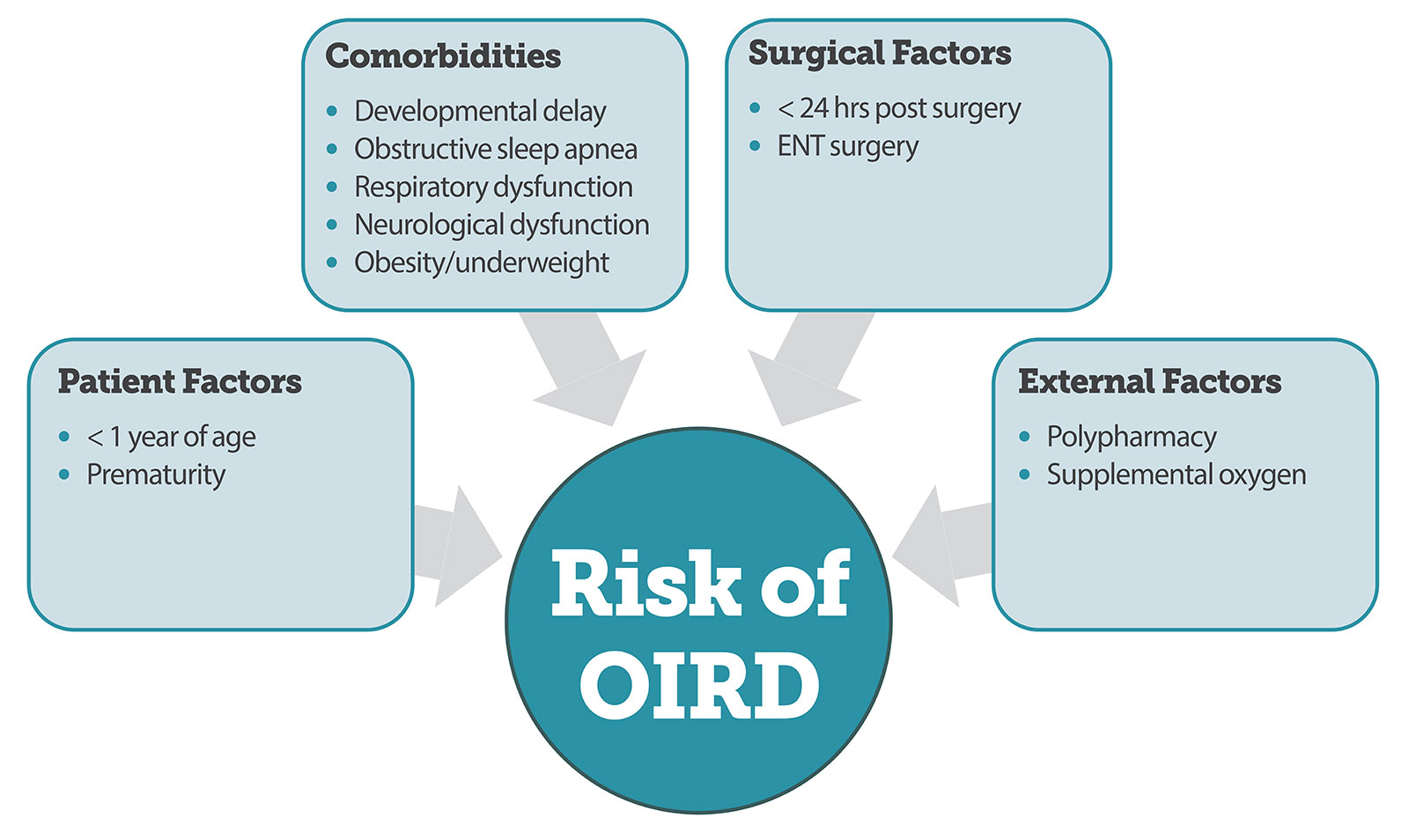
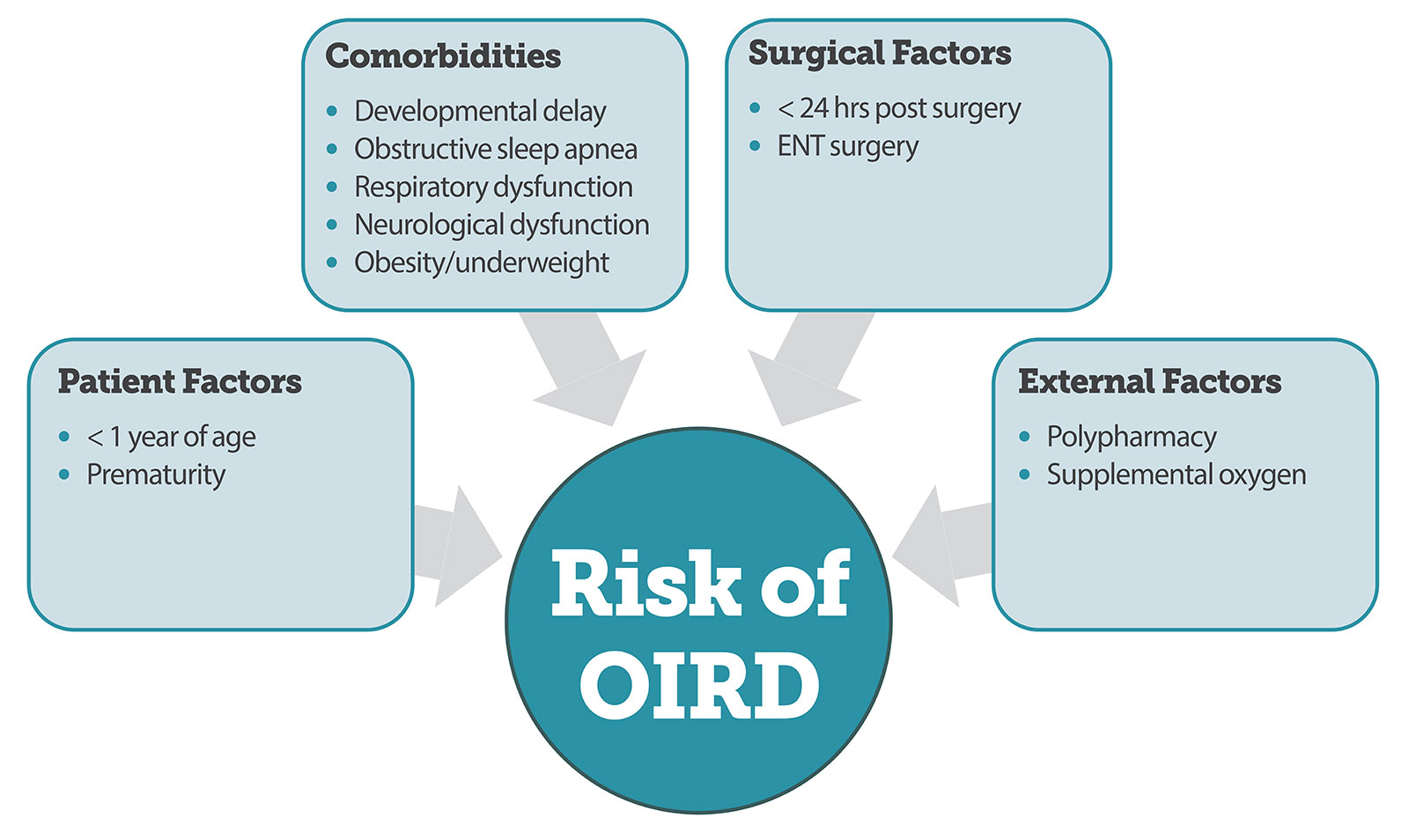
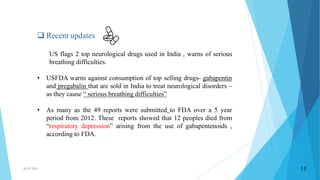
On December 19, 2019, FDA issued a warning to inform healthcare providers and patients of an increased risk of breathing problems clinically referred to as respiratory depression when using gabapentin or pregabalin. In a recent Drug Safety Update, the Medicines and Healthcare products Regulatory Agency (MHRA) warned about a rare risk of severe respiratory depression with gabapentin, with or without concomitant use of opioids.1 In England, 6.5 million prescriptions for gabapentin were dispensed in 2016.2 A European review of gabapentin was triggered by reports of patients developing respiratory depression Understanding Gabapentin-Induced Respiratory Depression How Gabapentin Affects Breathing. Gabapentin and its close relative, pregabalin, are known as gabapentinoids. While not opioids, these drugs can depress the central nervous system, which includes the area of the brain that controls breathing. There was an increased risk of respiratory depression in the gabapentinoid group, specifically in patients who had surgery within the previous 24 hours. Keywords: naloxone, opioid analgesics, respiratory depression, gabapentin, pregabalin, POSS. Introduction etrospectively reviewed the electronic health records of 8567 patients who underwent major laparoscopic procedures (lasting ≥90 minutes) from January 1, 2010, to July 31, 2014. We assessed potential associations among patient and perioperative variables and episodes of respiratory depression during phase-I recovery. Multivariable and propensity score–matched analyses were performed to Although these drugs, which include gabapentin (Neurontin) and pregabalin (Lyrica), are still believed to be far safer than opioids for long-term use, the U.S. Food and Drug Administration is now warning that they may cause “respiratory depression.” That means your breathing could become so slow and shallow that you end up with too much The US FDA is warning of a risk of serious, life-threatening or fatal respiratory depression during treatment with gabapentinoids including gabapentin (Gralise, Horizant, Neurontin) or pregabalin (Lyrica, Lyrica CR Footnote 1) for seizures or nerve pain in patients with respiratory risk factors. Risk factors include older age, chronic Although gabapentin is widely perceived as safe [5,6], drug-induced respiratory depression has been described when gabapentin is used alone or in combination with other medications [7–10]. Indeed, the product monograph was amended in 2014 to warn about possible respiratory depression when combined with opioids . Potential risk factors for Between 2012 and 2016, the estimated number of patients who filled a gabapentin prescription increased from 8.3 million to 13.1 million annually, and the number of patients who filled a pregabalin In 2019 the FDA issued a warning about the potential risks of respiratory depression in patients taking gabapentin or pregabalin in combination with central nervous system (CNS) depressants such as opioids, antidepressants, and benzodiazepines. The FDA also warned the medication could increase breathing difficulties in patients with underlying The agency is warning that serious breathing difficulties may occur in patients using gabapentin (Neurontin, Gralise, Horizant) or pregabalin (Lyrica, Lyrica CR) who have respiratory risk factors. Among those factors are use of opioid pain medicines and other drugs that depress the central nervous system (CNS), as well as conditions such as In this study, when compared to patients not exposed to preoperative gabapentin, the risk of respiratory depression was increased 60 percent for patients using regional anesthesia (odds ratio [OR Safety reports of gabapentin and pregabalin should be obtained from concerned manufacturers and reviewed for respiratory depression effects. There should be strict prescription monitoring and drug use evaluation studies. Concurrent use of gabapentin and pregabalin with other respiratory depressants such as opioids should be strictly monitored. Gabapentin has been associated with a rare risk of severe respiratory depression even without concomitant opioid medicines. Patients with compromised respiratory function, respiratory or neurological disease, renal impairment, and concomitant use of central nervous system (CNS) depressants might be at higher risk of experiencing severe The agency said it received 49 case reports of serious breathing problems in patients taking gabapentinoids, including 12 people who died from respiratory depression. It’s advising doctors, caregivers and patients taking gabapentinoids to be alert for signs of confusion, disorientation, dizziness, sleepiness, slow or shallow breathing The FDA issued a warning in December 2019 that serious breathing difficulties may occur in patients using gabapentin (Neurontin, Gralise, Horizant) or pregabalin (Lyrica, Lyrica CR) who have respiratory risk factors.¹ The risk factors include the use of opioid analgesics and other drugs that depress the central nervous system (CNS) and Gabapentin and pregabalin are FDA-approved for a variety of conditions, including of respiratory depression. CNS depressants include opioids, anti-anxiety medicines, Health care professionals should start gabapentinoids at the lowest dose and monitor patients for symptoms of respiratory depression and sedation when co-prescribing with an opioid or other CNS In the UK, there have been 50 Yellow Card reports of respiratory depression or dyspnoea associated with gabapentin between 19 February 1996 and 1 September 2017. Of these cases, 17 report opioids The FDA has required new warnings in the labels of gabapentin (Neurontin, and others) and pregabalin (Lyrica, Lyrica CR, and generics) about the risk of life-threatening or fatal respiratory depression in patients with respiratory risk factors.1 Respiratory risk factors include chronic obstructive pulmonary disease (COPD) and concurrent use of opioids or other CNS depressants.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
/lung-pain-symptoms-causes-and-diagnosis-2249389_2-5b854d75c9e77c005076c14a-5b85d1ddc9e77c002c6e365f.png) | 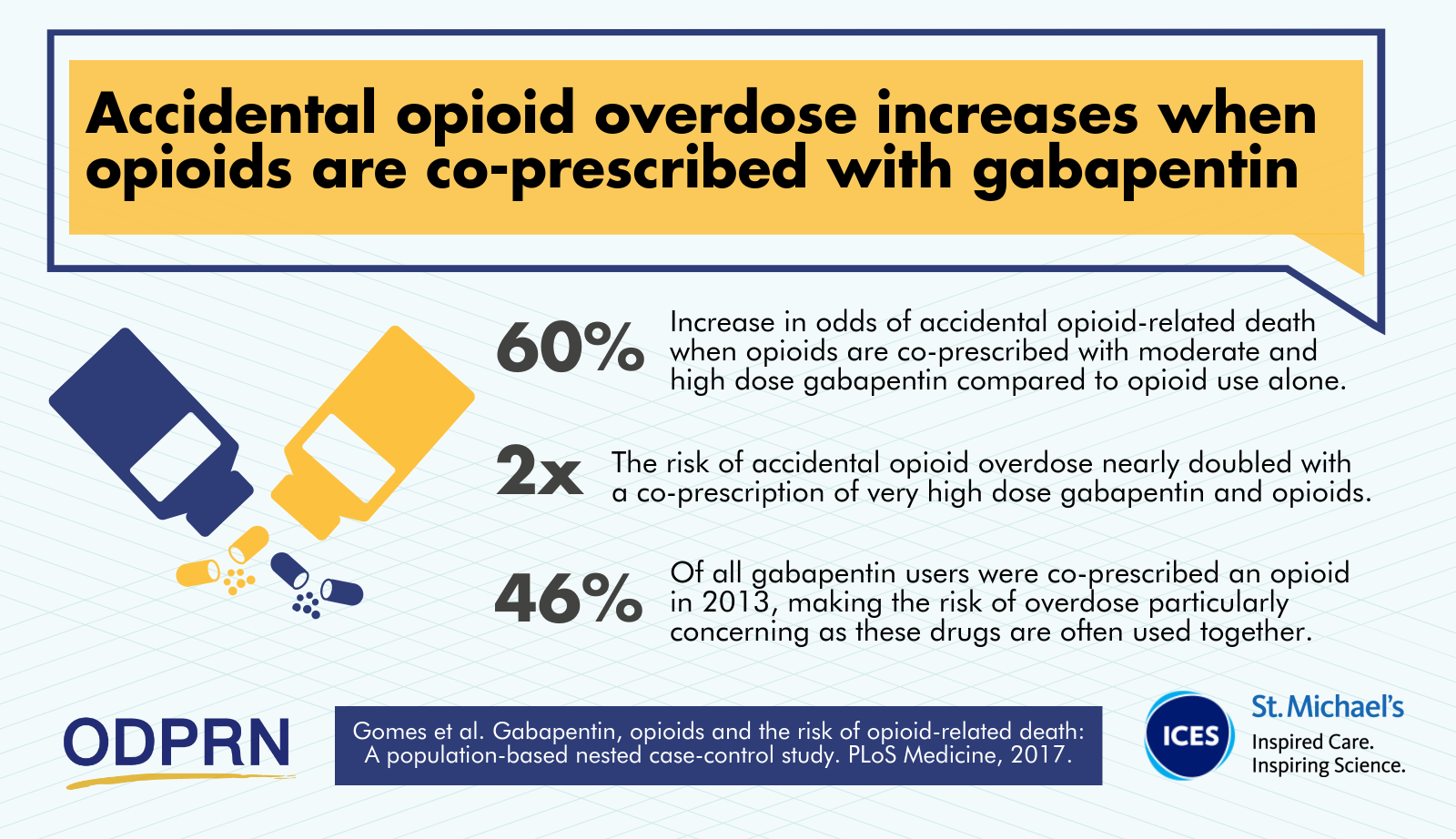 |
 | |
 |  |
 | |
 |  |