Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
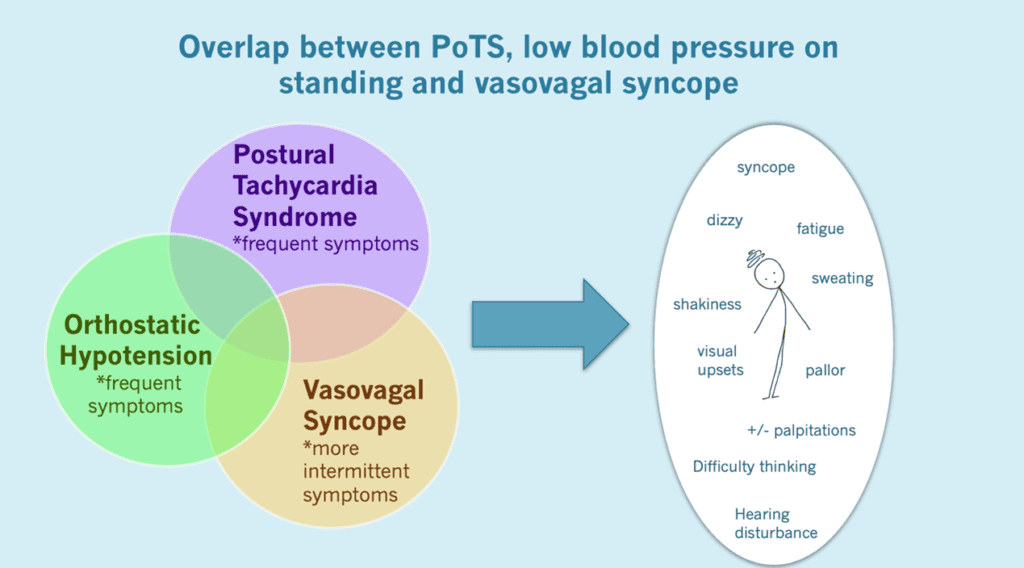
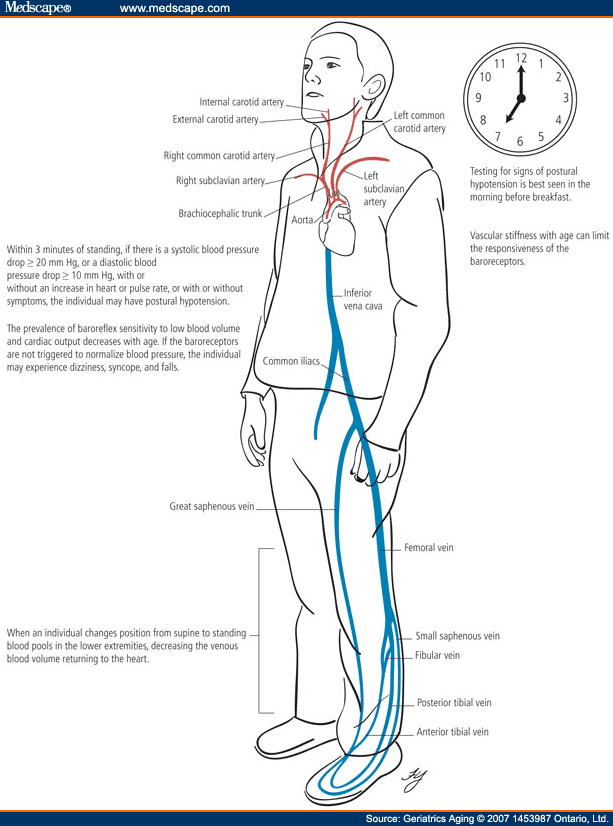
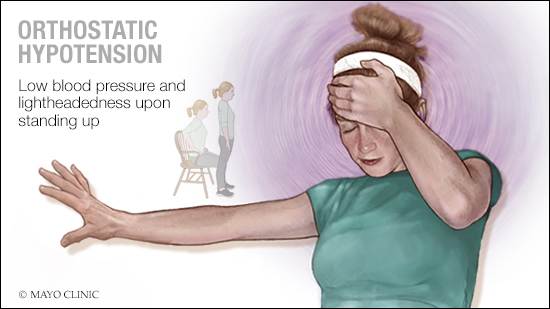
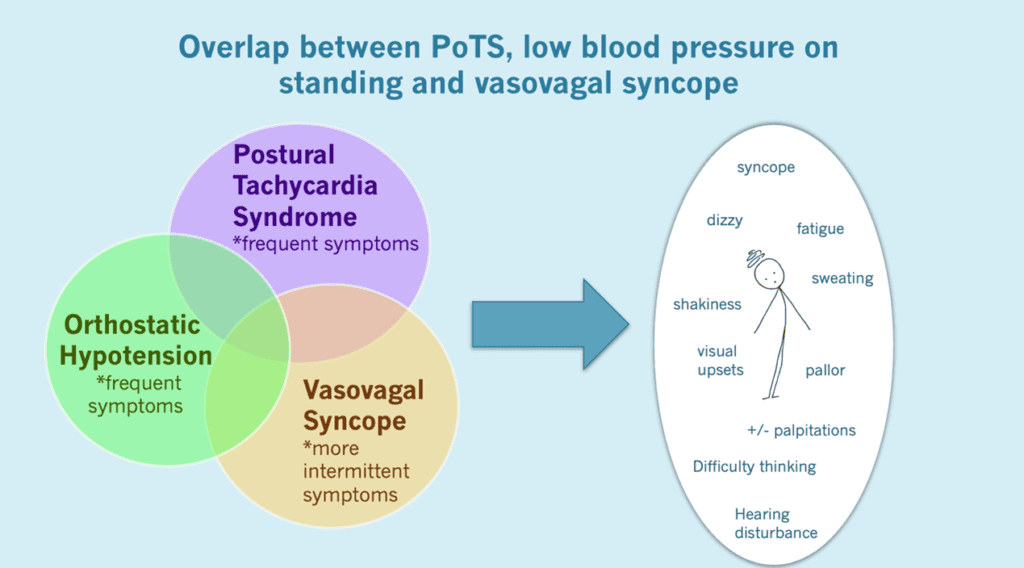
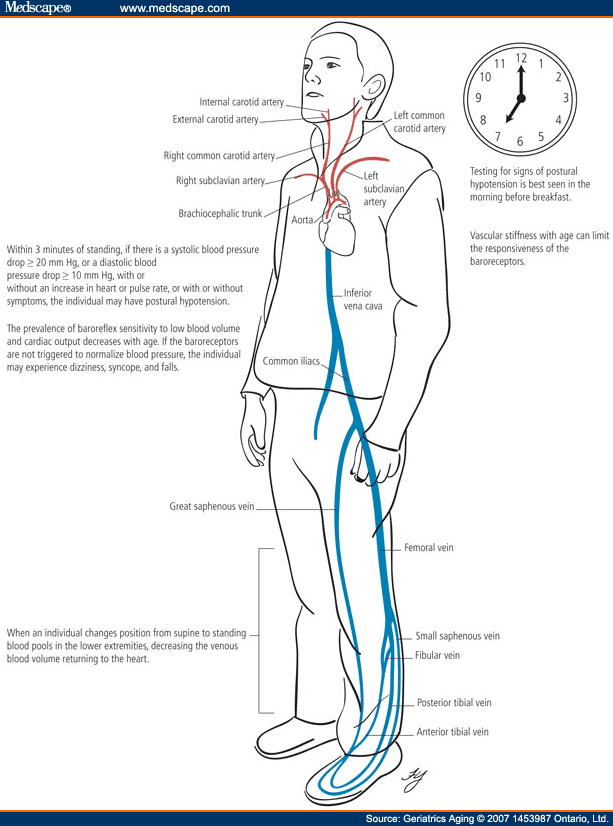
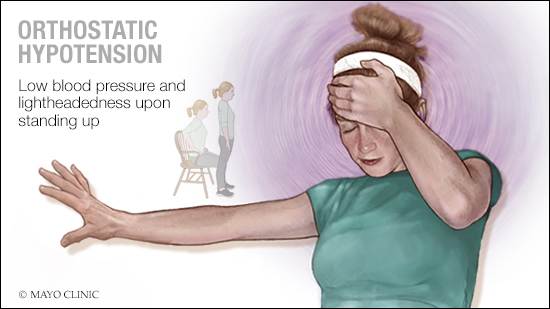
Several cardiovascular and psychoactive medications may alter the blood pressure response to standing, leading to drug-related orthostatic hypotension. This narrative review provides an overview on cardiovascular and non-cardiovascular medications potentially impairing orthostatic blood pressure. Chronic orthostatic hypotension (OH) is a common, often underdiagnosed, disorder, defined by an excessive fall in blood pressure (BP) with standing. OH can be associated with postural lightheadedness, dizziness, fatigue, coat hanger pain, and, in extreme situations, syncope, falls, and injuries. Rare but serious gabapentin side effects include mood changes in children. It can also cause suicidal thoughts or behaviors in children and adults. If you or your child experience changes in behavior or mood while taking gabapentin, contact your prescriber immediately. Orthostatic hypotension may result from neurogenic and nonneurogenic causes. Neurogenic orthostatic hypotension can be due to neuropathy (eg, diabetic or autoimmune neuropathies) or to central lesions (eg, Parkinson disease or multiple system atrophy). The underlying cause of orthostatic hypotension varies widely, including but not limited to: 1. Neurological Disorders. Conditions like Parkinson’s disease, Lewy body dementia, and multiple system atrophy impair the autonomic nervous system, leading to neurogenic orthostatic hypotension. Orthostatic hypotension is a condition described by a significant reduction in blood pressure that typically occurs upon standing or assuming an upright posture. It may be asymptomatic or symptomatic and can be due to impaired autonomic reflexes or intravascular volume depletion. Drug-induced orthostatic hypotension is an important clinical problem. When symptomatic, it is poorly tolerated by the patient, and can be a cause for discontinuing treatment. It may have more serious consequences if it leads to syncope, falls and injury, or to sustained loss of perfusion of vital o We present a 13-year-old female who experienced intraoperative hypotension which was eventually attributed to the preoperative ad-ministration of gabapentin. The perioperative use of gabapentin is discussed, its adverse effect profile re-viewed, and its potential role in perioperative blood pres-sure changes presented. The depressor effect of gabapentin in the NTS recovered gradually over 90 min after L-NAME treatment (-8 ± 2 versus -20 ± 3 mmHg and -13 ± 3 versus -36 ± 8 bpm; Figure 2B). These results indicated that gabapentin may have induced NOS to induce hypotension and bradycardia in the NTS of the SHR rats. Figure 2. carry cumulative risk, suggesting that individuals with polypharmacy could benefit from pos-tural BP monitoring. Author summary Why was this study done? • Orthostatic hypotension (OH) is a common side effect of drugs. It causes a reduction in blood pressure (BP) on standing, which results in reduced cerebral blood flow that is Figure. Spectrum of orthostatic hypotension (OH). Clinical development of OH requires the presence of autonomic impairment (due to aging, diabetes, and primary autonomic neuropathies) often in combination with aggravating factors that overwhelm or impair compensatory autonomic responses (volume depletion, infections, deconditioning, and medications). Hypotension and orthostatic hypotension may contribute to fall risk, but evidence is inconsistent. There is no strong evidence indicating a specific class is preferred over others due to lower fall risk. However, with the possibility of orthostatic hypotension contributing to falls and strong evidence of Measuring heart rate with each position change can help detect baroreflex dysfunction. 2, 22, 24, 27 The compensatory rise in heart rate is maintained in nonneurogenic orthostatic hypotension Orthostatic hypotension treatments vary by what’s causing it. Treatments may include: Treating a condition or disease that’s causing orthostatic hypotension. Changing the dose of a medication that causes orthostatic hypotension or switching to a different drug. Sitting up in bed if you’re on bed rest. Wearing elastic stockings on your legs. Orthostatic hypotension is a frequent cause of falls and syncope, impairing quality of life. It is an independent risk factor of mortality and a common cause of hospitalizations, which exponentially increases in the geriatric population. We present a management plan based on a systematic literature review and understanding of the underlying pathophysiology and relevant clinical pharmacology Some antidepressants, such as tricyclic antidepressants (TCAs), trazodone, and monoamine oxidase inhibitors (MAOIs), can cause orthostatic hypotension. That’s because they can relax blood vessels or interfere with blood pressure regulation. Orthostatic hypotension (OH) is a common side effect of drugs. It causes a reduction in blood pressure (BP) on standing, which results in reduced cerebral blood flow that is linked to falls, strokes, cognitive impairment, and increased mortality. Over 250 medications are associated with OH. Data on chronic opioid treatment are limited, but hypotension, orthostatic hypotension, and syncope are commonly reported among potential adverse effects of most opioid analgesics, such as morphine, buprenorphine, fentanyl, oxycodone, and tapentadol [55•]. Yet, the mechanism underlying opioid-mediated hypotension still remains a matter of debate. Syncope is a frequent cause of emergency department visits 22 and about half of these result in hospital admission. 23 About 24%-31% of patients presenting with syncope in the emergency setting have orthostatic hypotension. 24, 25 Orthostatic hypotension should be considered in the differential diagnosis of patients hospitalized for syncope Orthostatic hypotension is reported as a side effect among people who take Gabapentin (gabapentin), especially for people who are male, 60+ old, have been taking the drug for < 1 month also take Aspirin, and have High blood pressure.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |