Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
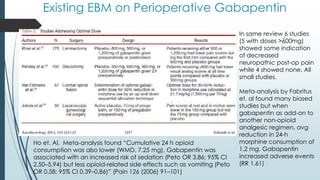
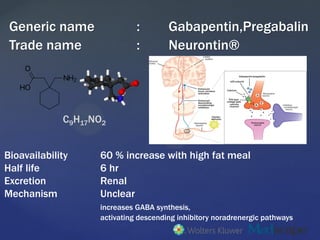
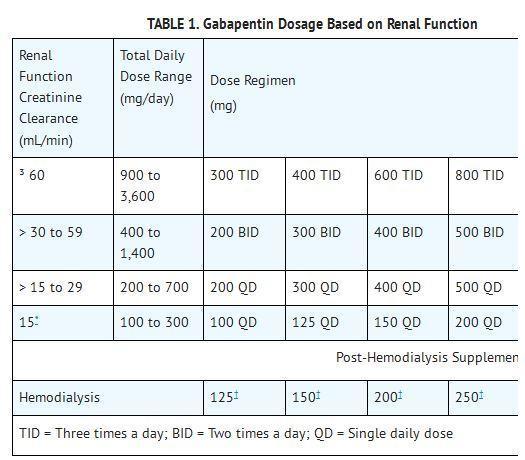
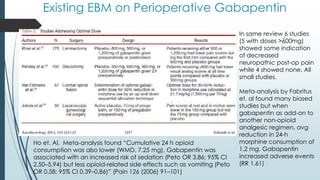
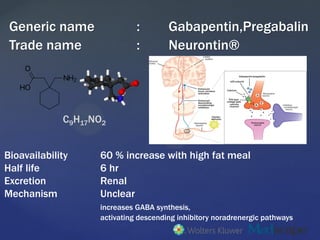
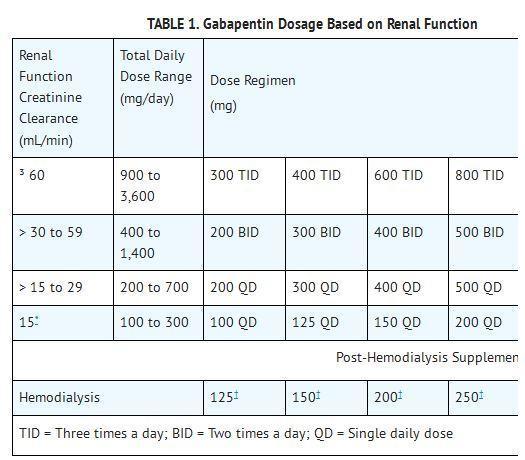
Gabapentin exposure was reported to have been proportional to the dose of gabapentin enacarbil administered, with no prolongation of QT interval observed at any of the dose levels. At all 4 doses, gabapentin enacarbil was reported to have been generally well-tolerated. of drug-induced QT prolongation GRAHAM PARSONS Many drugs are associated with QT prolongation and certain patient factors can increase this effect, leading to a significant risk of arrhythmias. This article describes the drug and patient factors that can lead to QT prolongation and discusses how the risks can be reduced. P R Q S T Figure 1. Drugs associated with QT Prolongation, QTc prolongation including Antipsychotics, antiarrhythmics, antidepressants, and antihistamines With regards to drugs, the risk of QT prolongation and TdP varies markedly across the list but tends to be rather similar within a drug class. While the risk of TdP is well-defined for many of these agents, many are classified as QT-prolonging solely based on their drug class or presumed pharmacodynamic effects. A QT–concentration relationship was reported with moxifloxacin. Gabapentin exposures were dose-proportional with gabapentin enacarbil doses of 1200 and 6000 mg. The most commonly reported adverse events with gabapentin enacarbil 6000 mg were dizziness and somnolence (60.0% and 54.0%, respectively). The upper limit of the normal reference QTc intervals for males is 450 ms and that for females is 460 ms. There is considerable intra-individual variability of the QTc up to 76–102 ms over the course of 24 h. QTc intervals longer than 500 ms are a major risk factor for the development of TdP. MECHANISM OF CORRECTED QT PROLONGATION In addition, the potential role of antiepileptic drugs has been suggested. While the preponderance of clinical data would suggest that use of most antiepileptic drugs does not pose excessive additional risk of QT prolongation, available data also do not provide sufficient evidence that these drugs are entirely free of risk in all patients. that for every 10 ms increase in QTc there is a 5% increase in the risk of arrhythmic events.7 Drug induced QT prolongation is often dose related. For example, citalopram 20 mg daily has been shown to cause a mean change in baseline QTc of 7.5 ms; this increases to 16.7 ms with citalopram 60 mg daily.1 Long qt syndrome is reported as a side effect among people who take Gabapentin (gabapentin), especially for people who are female, 60+ old, also take Aspirin, and have High blood pressure. Considering that not all agents that prolong the QT interval increase TDR, drugs can be distinguished into the following groups depending on their simultaneous effects on the QT corrected using the Bazzet’s formula (QTc) interval and on TDR: (1) drugs inducing both QTc prolongation and increased TDR, characterized by a high torsadogenic Pregabalin use has been associated with QTc prolongation in patients taking other QTc–prolonging agents, although the relative contributions of pregabalin to QTc prolongation may be minimal. Pregabalin and gabapentin have been associated with a dose-related increased risk of atrial fibrillation. the degree by which a drug changes the QTc interval from baseline is also important . an increase in baseline QTc of around 5 ms or less is not considered significant and this is the threshold for regulatory concern; for drugs that increase the QTc interval by less than 20 ms the data are inconclusive with regard to arrhythmic risk In general, manufacturers advise that the use of two or more drugs that are associated with QT prolongation should be avoided. Increasing age, female sex, cardiac disease and some metabolic disorders (notably hypokalaemia) predispose to QT prolongation. Prescribers should also use caution when prescribing concurrent drugs that reduce serum A QT-concentration relationship was reported with moxifloxacin. Gabapentin exposures were dose-proportional with gabapentin enacarbil doses of 1200 and 6000 mg. The most commonly reported adverse events with gabapentin enacarbil 6000 mg were dizziness and somnolence (60.0% and 54.0%, respectively). Both pharmacokinetic and pharmacodynamic drug interactions can significantly increase the risk of QT prolongation. Pharmacists may help reduce the risk of serious ventricular arrhythmias by screening for potential interactions. As the QT interval varies with a change in heart rate, various formulae can adjust for this, producing a 'corrected QT' (QTc) value. Normal QTc intervals are typically <450 ms for men and <460 ms for women. For every 10 ms increase, there is a ~5% increase in the risk of arrhythmic events. o Reference ranges for prolonged QTc interval (men QTc >440 msec, women QTc >470 msec) & age-related differences (children/older adults) o Patient and drug-specific risk factors for Torsade de Pointes to enable completion of following risk assessment when initiating new medication: Does the Among the mood stabilizers, lithium has a moderate risk of QTc prolongation while the antiepileptics used for this purpose such as carbamazepine, oxcarbazepine, topiramate, valproate, pregabalin, gabapentin, and lamotrigine are reported to be safe with a low risk of QTc prolongation. In the field of pain medicine all the major drug classes (i.e. NSAIDs, opioids, anticonvulsive and antidepressant drugs, cannabinoids, muscle relaxants) contain agents that increase the risk of QT prolongation. The risk of QT interval prolongation was evaluated in a thorough QTc trial in 247 healthy individuals following treatment with LCM at 400 or 800 mg/day. Exposure to LCM did not appear to cause QT prolongation, nor does it seem to have important effects on QRS duration {UCB, Inc., data on file}.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |