Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
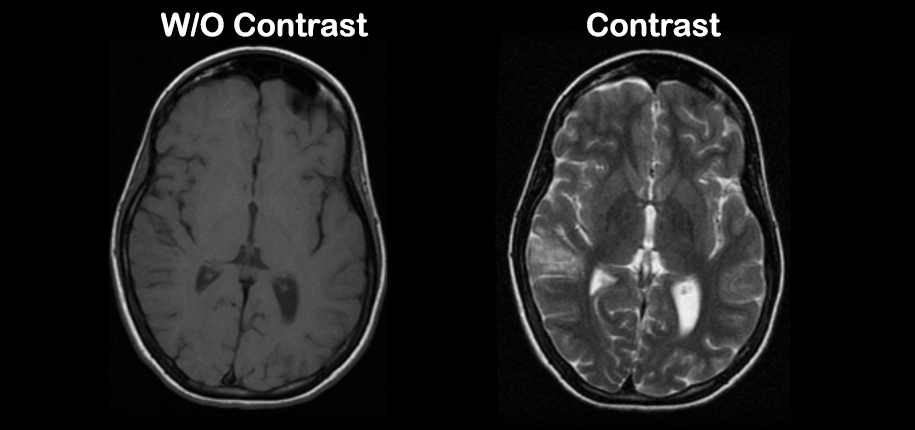
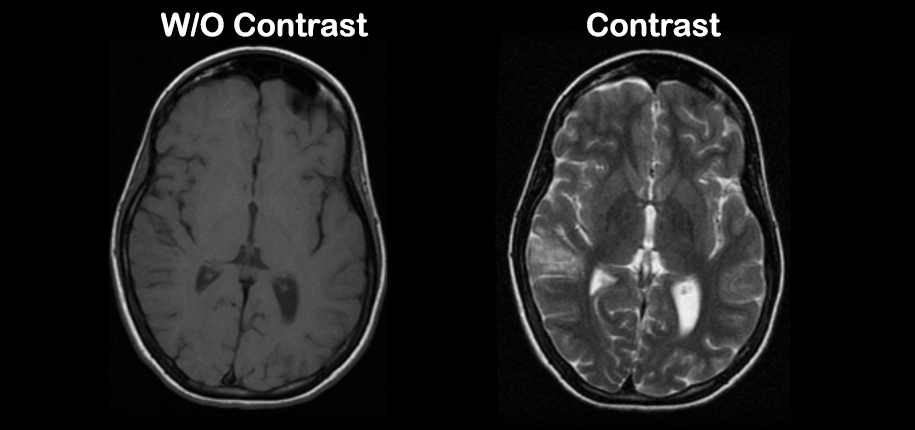
Happy Monday all - I had a MRI on 12/26 with Gandolinium contrast -within 12 hours I developed the most excruciating pain in y left thigh which settled in my lower left calf - went t my PCP but he was useless - on January 16 I received my first Moderna vaccine and I developed some symptoms that - I know that now - are Erythromelalgia (not confirmed) again went to PCP and a Podiatrist (not on-specific considerations in the prevention and management of Contrast Induced Nephropathy (CIN). It is designed to be read in conjunction with and to complement information released in 2016 by the Royal Australian and New Zealand College of Radiologists (RANZCR)1 and in 2017 by the Agency for Clinical Innovatio. A gadolinium-based contrast agent (GBCA) is a clear contrast fluid that we inject into a vein during MRI scans to better detect medical problems. For over 30 years, GBCAs have been used in over 450 million patients worldwide to improve their MRI scans. The brand of GBCA most commonly used at Penn Medicine is Dotarem or Eovist. Unenhanced axial T1-weighted MR images (MRI) of the posterior fossa at the level of the dentate nucleus of our patient (first and second line) and same views taking advantage of contrast enhancement by ImageJ (third and fouth line): (a, A, I MRI) before any gadolinium administration (dentate nucleus-to-pons signal intensity ratio = 1.0259), (b In patients with post-radiological neurological deficits, contrast-induced neurotoxicity (CIN) should be among the top differentials. In this case report, we present the case of a 61-year-old female who experienced classical signs and symptoms of neurotoxicity after a cerebral angiogram. I've been taking Gabapentin for a week, 900mg total daily. I am having an MRI on my lumbar spine in a few days. Will Gabapentin interfere or "mask" anything that might otherwise show on the MRI? FDA is requiring a new class warning and other safety measures for all gadolinium-based contrast agents (GBCAs) for magnetic resonance imaging (MRI) concerning gadolinium remaining in patients Magnetic resonance imaging confirmed the presence of myositis confined to the left thigh and the patient's symptoms and laboratory abnormalities resolved following Gabapentin cessation. Magnetic resonance imaging confirmed the presence of myositis confined to the left thigh and the patient's symptoms and laboratory abnormalities resolved following Gabapentin cessation. Unenhanced axial T1-weighted MR images (MRI) of the posterior fossa at the level of the dentate nucleus of our patient (first and second line) and same views taking advantage of contrast enhancement by ImageJ (third and fouth line): (a, A, I MRI) before any gadolinium administration (dentate nucleus-to-pons signal intensity ratio = 1.0259), (b We have two overall objectives in this systematic review: firstly, what is the effect of holding RAS blockers, NSAIDs, diuretics or metformin before the administration of contrast media on the risk of CI-AKI and related renal complication in patients who undergo contrast procedures? to inject the contrast in exactly the right place. A fluoroscope is an X-ray machine that shows live pictures. It will also help your radiologist see the dye as it moves through your joint. -ray dye, lidocaine, and MRI contrast. This mixture helps the radiologist see the contrast during both the arthrogram and the MRI. The lidocaine will help ease MRI revealed diffuse multi-compartmental hyperintense T2 signal (muscle edema) and heterogeneous contrast enhancement within the left medial thigh. Given the absence of trauma and a negative ultrasound and CTA, these MRI findings were strongly favoured to be secondary to an inflammatory process. Introduction. Medicine is an art of balancing risks and benefits. When it was discovered that gadolinium in gadolinium-based contrast media was not excreted fully from the body (), even in patients with normal renal function (), it threw the risk-benefit assessment of patients being considered for contrast material–enhanced magnetic resonance (MR) imaging into turmoil. Overall, the described interference for iodinate contrast media include inappropriate gel barrier formation in blood tubes, the appearance of abnormal peaks in capillary zone electrophoresis of serum proteins, and a positive bias in assessment of cardiac troponin I with one immunoassay. Because of the favorable side effect profile, we settled for a symptomatic therapy with gabapentin. In contrast to pregabalin, its dosage can be increased more rapidly. Gabapentin has an inhibitory effect on voltage-gated calcium channels and is used as an antiepileptic drug as well as in the treatment of neuropathic pain. Intravenous administration of a gadolinium-based contrast agent (GBCA) is indicated in over one-third of MRI examinations to obtain the necessary information. While GBCA is well tolerated in most patients, it is associated with a small risk for nephrogenic systemic fibrosis (NSF) or acute adverse reaction. In patients with cardiovascular disease, kidney disease, and/or diabetes, renin-angiotensin system blockers, non-steroidal anti-inflammatory drugs, diuretics, and metformin can increase the risk of CI-AKI when undergoing contrast imaging. Since its introduction more than 35 years ago, gadolinium-enhanced MRI has fundamentally changed medical practice. Although extraordinarily safe, gadolinium-based contrast agents (GBCAs) may have side effects. Four distinct safety considerations include acute allergiclike reactions, nephrogenic systemic fibrosis (NSF), gadolinium deposition, and symptoms associated with gadolinium exposure Gadopentetate injection is a magnetic resonance imaging (MRI) contrast agent that is used to help create a clear picture of the body during an MRI scan. MRI scans are a special kind of diagnostic procedure that use magnets and computers to create images or “pictures” of certain areas inside the body. Unlike x-rays, they do not involve
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |