Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
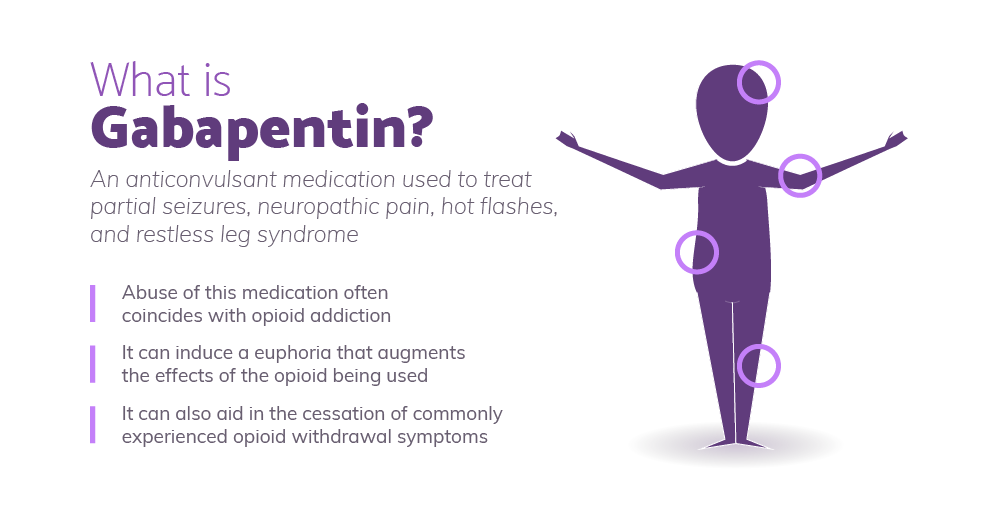
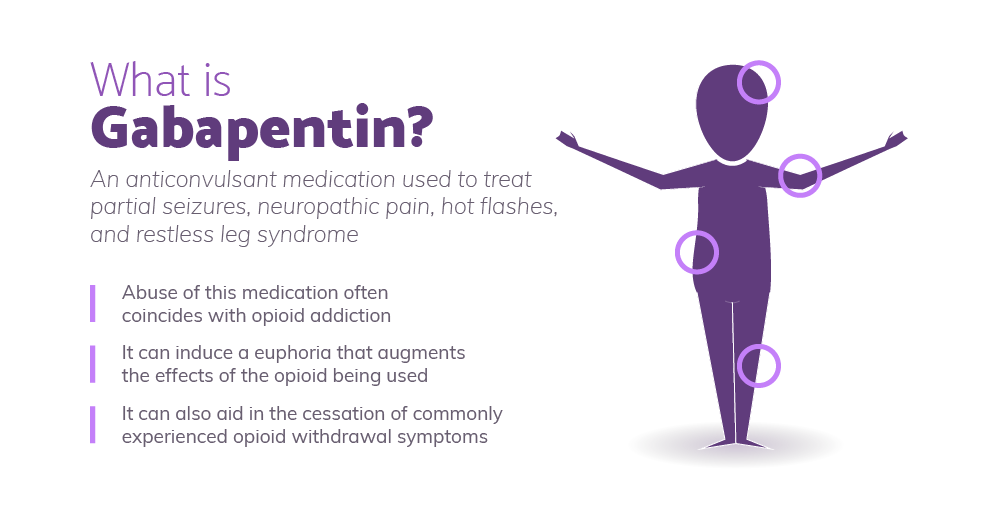
Orthostatic hypotension is a frequent cause of falls and syncope, impairing quality of life. It is an independent risk factor of mortality and a common cause of hospitalizations, which exponentially increases in the geriatric population. We present a management plan based on a systematic literature review and understanding of the underlying pathophysiology and relevant clinical pharmacology Summary: Orthostatic hypotension is reported as a side effect among people who take Gabapentin (gabapentin), especially for people who are male, 60+ old, have been taking the drug for < 1 month also take Aspirin, and have High blood pressure. Neurogenic orthostatic hypotension (OH) is a disabling disorder caused by impairment of the normal autonomic compensatory mechanisms that maintain upright blood pressure. Nonpharmacologic treatment is always the first step in the management of this We treated four patients affected by orthostatic tremor (OT) with gabapentin in increasing doses (300 to 2,400 mg/d). OT was evaluated with patients' self-monitoring scales, tremor rating scales, electromyography(EMG) showing the 14- to 18-Hz frequencies, and EMG frequency analysis. Gabapentin may improve tremor, stability, and QOL in patients with OT, and symptomatic response correlated with a reduction in tremor amplitude and postural sway. The findings confirm previous reports of symptomatic benefit with gabapentin and provide justification for larger controlled clinical trials. Chronic orthostatic hypotension (OH) is a common, often underdiagnosed, disorder, defined by an excessive fall in blood pressure (BP) with standing. OH can be associated with postural lightheadedness, dizziness, fatigue, coat hanger pain, and, in extreme situations, syncope, falls, and injuries. Orthostatic hypotension is defined as a decrease in blood pressure of 20 mm Hg or more systolic or 10 mm Hg or more diastolic within three minutes of standing from the supine position or on Drug-induced orthostatic hypotension is an important clinical problem. When symptomatic, it is poorly tolerated by the patient, and can be a cause for discontinuing treatment. It may have more serious consequences if it leads to syncope, falls and injury, or to sustained loss of perfusion of vital o In this narrative review we present an overview of drugs acting on the cardiovascular and central nervous system that may potentially impair the orthostatic blood pressure response and we provide practical suggestions that may be helpful to guide medical therapy optimization in patients with OH. Drug-induced orthostatic hypotension: A systematic review and hypotension. Orthostatic hypotension is a chronic, debilitating illness that is difficult to treat. The therapeutic goal is to improve postural symptoms, standing time, and function rather than to achieve upright normotension, which can lead to supine hypertension. Drug therapy alone is never adequate. Figure. Spectrum of orthostatic hypotension (OH). Clinical development of OH requires the presence of autonomic impairment (due to aging, diabetes, and primary autonomic neuropathies) often in combination with aggravating factors that overwhelm or impair compensatory autonomic responses (volume depletion, infections, deconditioning, and medications). OH did not significantly impact length of hospitalization, progression free and overall survival. Multivariable analysis revealed four risk factors (i.e. ≥0.5% weight loss/day, white race, gabapentin, antihypertensives) and two protective factors (i.e. antihistamine, proton pump inhibitor) associated with the development of peri-transplant OH. Orthostatic hypotension (OH) is common, affecting up to 30% of the general population over 65 and up to 70% of people living in nursing homes. It is defined by a drop in the systolic blood pressure (BP) of 20 mmgh or/and diastolic BP of 10 within 3 min of standing. Neurogenic orthostatic hypotension is a type of OH caused by autonomic failure and multiple system atrophy. It is relatively We report seven patients with orthostatic tremor (OT) who were successfully treated with the anticonvulsant gabapentin. Five of the patients had been previously tried on clonazepam, the most commonly used drug for OT, four without any benefit. Orthostasis Condition: Orthostasis or orthostatic hypotension (OH) is a decrease in blood pressure that happens soon after standing or sitting up. When a person stands up, gravity causes blood to pool in the legs. This reduces blood pressure since less blood is circulating back to the heart to pump. If orthostasis and other symptoms continue despite changes in the Norvasc and gabapentin, the next two drugs that should be looked at are tamsulosin, Sinemet, and ropinerole. Unlike gabapentin, they also reported a dose response, with a greater response being seen in those taking 600 mg daily than in those taking 300 mg . Pregabalin has also been shown to decrease health care and non–health care costs compared with gabapentin in the treatment of peripheral neuropathic pain . Drug-induced orthostatic hypotension (OH) is common, and its resulting cerebral hypoperfusion is linked to adverse outcomes including falls, strokes, cognitive impairment, and increased mortality. The extent to which specific medications are associated with OH remains unclear. Orthostatic hypotension (OH) is a common side effect of drugs. It causes a reduction in blood pressure (BP) on standing, which results in reduced cerebral blood flow that is linked to falls, strokes, cognitive impairment, and increased mortality. Over 250 medications are associated with OH.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |