Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
03222-3.fp.png) |  |
 |  |
 |  |
 |
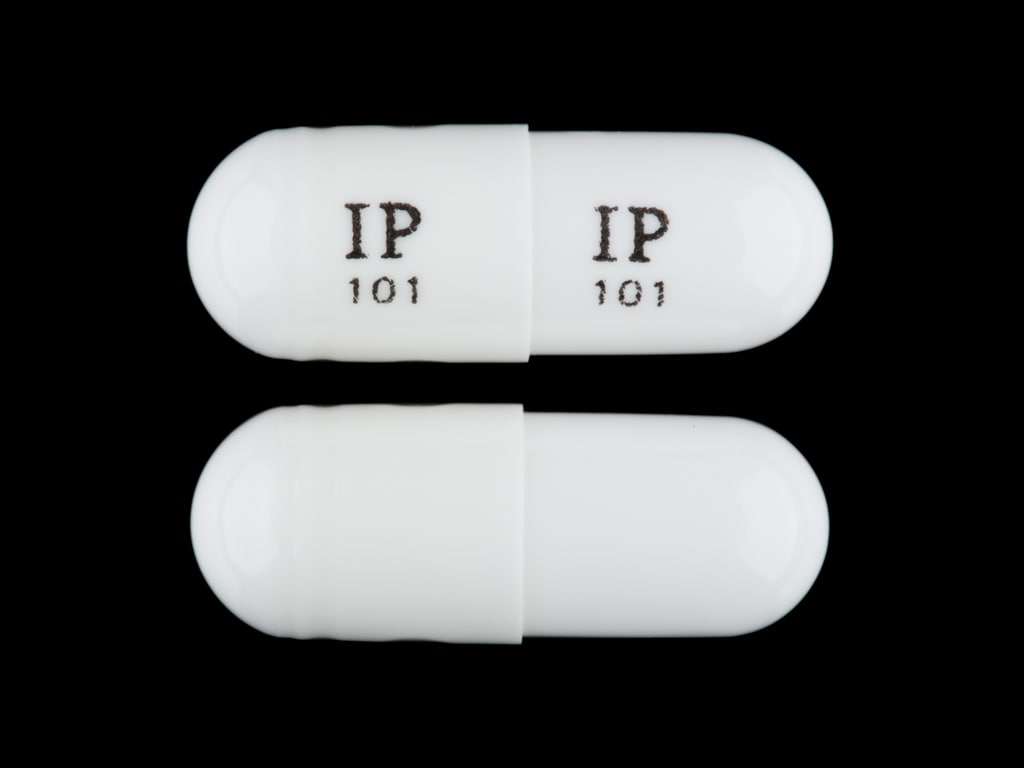
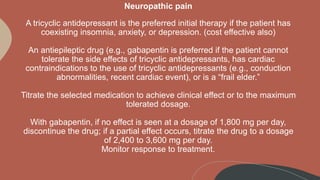
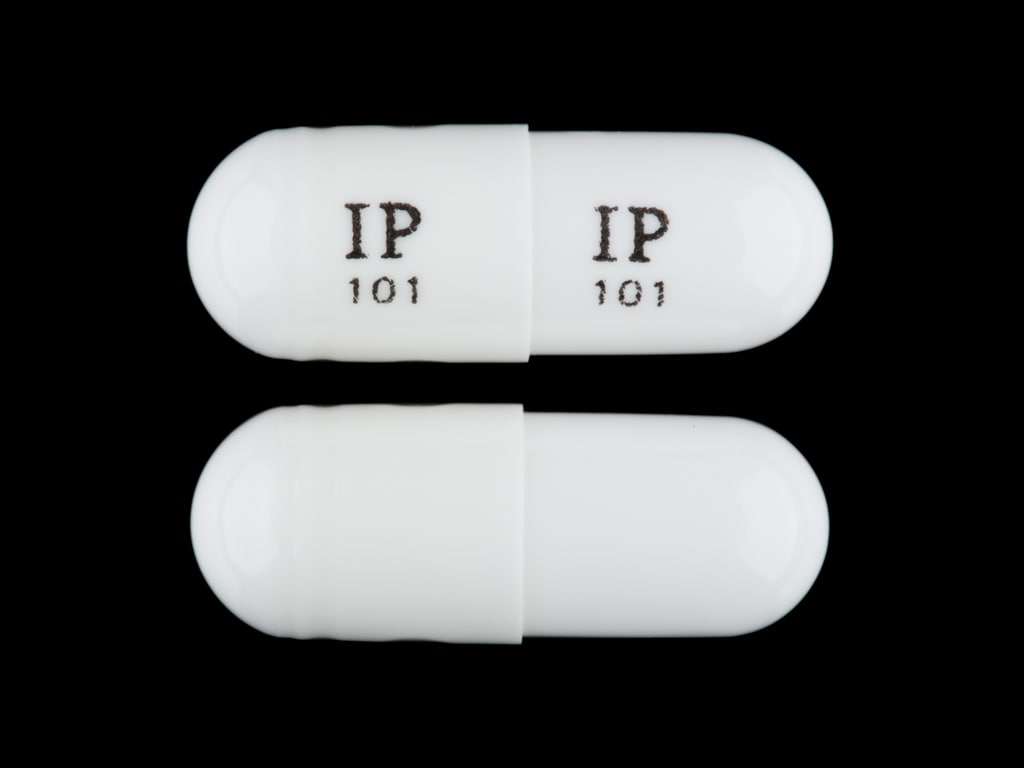
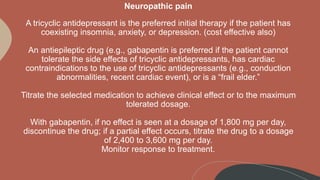
The question of whether gabapentin is “hard on the heart” is complex and warrants careful examination. While primarily known for its use in treating nerve pain, seizures, and restless legs syndrome, gabapentin’s impact on the cardiovascular system is increasingly being recognized. Gabapentinoids can cause concentration-dependent peripheral edema of early onset. The primary mechanism of non-cardiogenic peripheral edema is vasodilatory edema secondary to altered myogenic tone, independent of Ca<sub>v</sub>1.2 blockade under the experimental conditions tested. Moreover, the use of gabapentin and pregabalin have increased in the USA from 1.2% of adults in 2002 to 3.9% in 2015, with the largest increases in older adults, those with diabetes and those with at least 5 comorbidities. In this focused review, we discuss the cardiovascular safety of gabapentin and pregabalin. Heart Failure The incidence of heart murmurs in apparently healthy cats is only 16% to 44%. 6-8 The prevalence of cardiomyopathy detected by echocardiography in a large population of shelter cats was 15.3%, and the most prevalent primary heart disease in these cats was hypertrophic cardiomyopathy. 8 For cats with heart disease, arrhythmias may have more The goal was to determine whether the prescription of gabapentin and pregabalin in patients with fibromyalgia increases the risk of adverse cardiovascular events, including peripheral vascular disease, strokes, myocardial infarcts, heart failure, deep venous thrombosis, and pulmonary embolism. between short-term (3 month) gabapentin use and heart failure, myocardial infarction, peripheral vascular disease, deep venous thrombosis, and pulmonary embolism. Short-term (3 month) pregabalin use was associated with deep Background Gabapentin and pregabalin are commonly prescribed medications to treat pain in patients with diabetic neuropathy. Gabapentin and pregabalin can cause fluid retention, which is hypothesized to be associated with cardiovascular diseases. However, whether long-term use of gabapentin and pregabalin is associated with adverse cardiovascular diseases remains unknown. This study aims to Gabapentin was discontinued and the patient was started on diltiazem 30 mg per oral four times a day and apixaban 5 mg per oral twice daily. which led to a decrease in the patient’s heart rate to ~60 beats per minute. In patients with diabetic neuropathy who were prescribed gabapentin and pregabalin, there is an increased risk for heart failure, myocardial infarction, peripheral vascular disease, stroke, deep venous thrombosis, and pulmonary embolism with long-term use. Our findings suggest that increased risk fo This study evaluated whether perioperative administration of gabapentin in cardiac surgery patients could reduce postoperative opioid consumption, postoperative sleep or perceived quality of recovery. This randomised controlled trial assigned 60 patients undergoing cardiac surgery to receive 1200 mg Although the most frequent side effects of gabapentin are associated with the central nervous system, gabapentin can also affect the cardiovascular system. Case reports and observational studies have showed that gabapentin can be associated with increased risk of atrial fibrillation. Oral and intravenous gabapentin can markedly attenuate blood pressure (BP) in hypertensive rats. The nucleus tractus solitarii (NTS) is the primary integrative center for cardiovascular control and other autonomic functions in the central nervous system. Gabapentin is a commonly used medication used as an anti-convulsant or analgesic. The well-known side-effects of gabapentin are dizziness, drowsiness and fatigue. In rare cases, it can lead to development of new onset congestive heart failure (CHF) or decompensation of pre-existing CHF. Gabapentin attenuates cardiac remodeling by inhibiting inflammation via peroxisome proliferator-activated receptor-γ activation and preventing calcium overload. Gabapentin (GBP), a GABA analogue, is primarily used as an anticonvulsant for the treatment of partial seizures and neuropathic pain. Whereas a majority of the side effects are associated with the nervous system, emerging evidence suggests there is a high risk of heart diseases in patients taking GBP. In patients with diabetic neuropathy who were prescribed gabapentin and pregabalin, there is an increased risk for heart failure, myocardial infarction, peripheral vascular disease, stroke, deep venous thrombosis, and pulmonary embolism with long-term use. Gabapentinoids can cause concentration-dependent peripheral edema of early onset. Reduced myogenic tone is the main mechanism of these non-cardiogenic edemas. In case of peripheral edema or heart failure, a drug etiology should be considered. Then, peripheral edema developed associated with the recommended dose of gabapentin, which was used in place of pregabalin. Despite the lack of any published evidence, the New York Heart Association issued a warning about using caution when prescribing pregabalin to type III-IV heart failure patients. A recently published report describes the case of a patient who developed non-ischemic cardiomyopathy following initiation of gabapentin therapy for pain management.. The patient, a 44-year-old African American female, with no prior cardiac history, presented to the emergency department (ED) complaining of shortness of breath and cough. There is research to suggest that cardiovascular effects occur after taking gabapentin. In this article, we’re going to take a look at what gabapentin is, how it could affect your heart, the other side effects of gabapentin use, and how you can keep your heart rate healthy. Keep reading now to learn more. What Is Gabapentin?
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
03222-3.fp.png) |  |
 |  |
 |  |
 |