Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
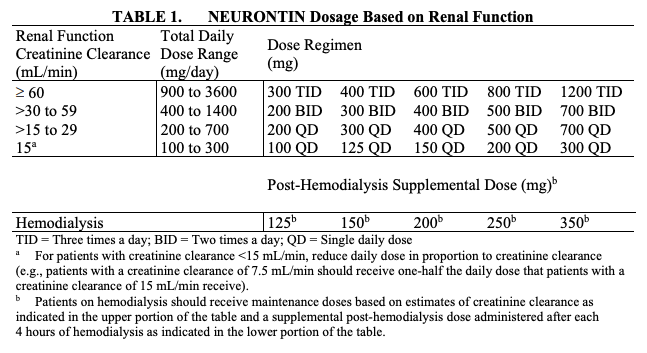
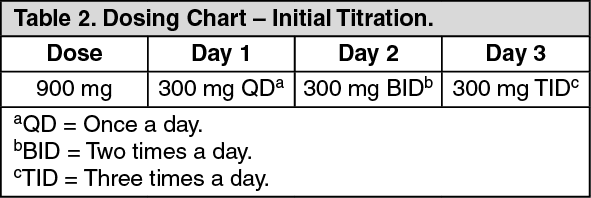
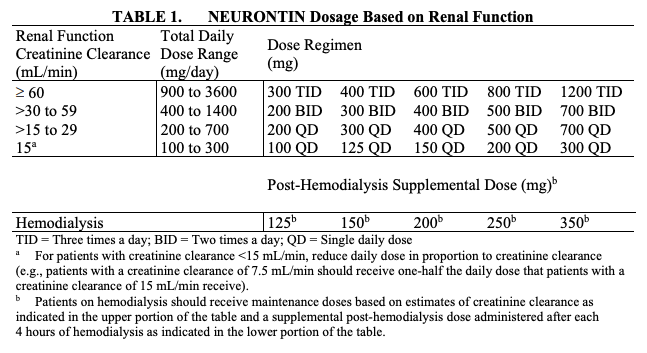
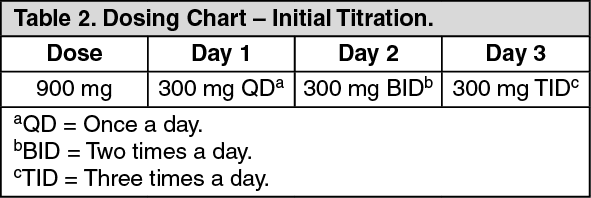
Reduction in pain by 50% is a commonly used endpoint in clinical pregabalin dose and titrating up the gabapentin dose. Example withdrawal schedule for a dose Dose reduction should be gradual, for example stepping down every 10 days but no faster than once a week, unless advised and supervised by a health care professional. Please see table overleaf for your individual gabapentinoid reduction plan. • Where possible, ensure any reduction is discussed and agreed with the patient. • Agree the speed of dose reduction with the patient. • Typically, one change per week is recommended. Some patients will need space to acclimatise to the new dose so the dose changes may be every one to two weeks. Emotional Stress: Mood swings or panic attacks may occur without a taper schedule to soften the transition. Gabapentin Taper Schedule. Gabapentin taper schedule isn’t one-size-fits-all. Some individuals can lower their dose in a matter of weeks, while others may need months for a more comfortable transition. Review patients prescribed gabapentinoids as appropriate with a view to dose reduction/treatment cessation where appropriate; Continue to review prescribing practice to ensure adherence to the NHSGGC Chronic Non-Malignant Neuropathic Pain Guidelines Prescribe gabapentinoids with caution in the elderly NHSGGC Prescribing Indicator Sevelamer — absorption of gabapentin may be reduced if taken concurrently with sevelamer. Gabapentin should be taken at least 1 hour before, or 3 hours after, sevelamer if the reduction in gabapentin levels is clinically significant. Morphine — interaction of gabapentin with morphine sulphate increases risk of respiratory depression. Tapering or slowly reducing your dose is recommended to stop taking gabapentin. Tapering off will help you avoid side effects. The timeline to reduce gabapentin depends on the individual and Dose reductions can be made weekly (except in the instance of transdermal fentanyl), two weekly or monthly, and should be guided by what the person can manage. Frequency of dose reduction can change during the tapering process. PK !T ¼Ù© [Content_Types].xml ¢ ( Ä–ËnÂ0 E÷•ú ‘· 1°¨ªŠÀ¢ e‹Tú &ž€Ûø!{xý}' ¢ ‚ Q7‘’™{ï M"g0Zë mSÃi³L¥Pé 7çm !Ðfu W -”Ùó å0 = OÊëƒTÖ 79„ë ”¾Íñ€H‚6vÎ +˜~´Fñ˼ $³ Å6¶QY7B€‘-1ì æ $øÞõ Jã³öÐJ~i|æüý ž¿ü3çÏ(r"¦9´A°³n„@:t¡¼^þ&lmNERçØ[ è ÷ { ~ ê ìÀ£:ý¥U‰d}ñ|P Í dM6ßþÒ ÿÿ PK In older adults and in the presence of psychiatric illness, gabapentin discontinuation should follow a slow tapering schedule, as for benzodiazepines (e.g., biweekly reduction of 10–25% of dose), and patients should be monitored carefully for emerging withdrawal symptoms. Specific tapering recommendations for gabapentin vary. If using gabapentin for epilepsy, some studies recommend to decrease your dose slowly (over months) to avoid recurrent seizures. Data indicates that seizures most often occur in the first six months after beginning to taper. The dose should be reduced gradually each week as this will minimise withdrawal effects. It will also allow you to check if there is any change in your pain. The amount and time will depend on your current dose and how long you have been taking the medication. Often the dose can be reduced in reverse order to how it was increased. £543,385 was spent on pregabalin and gabapentin.[epact2 2021] There is published evidence that both gabapentin and pregabalin are subject to abuse and misuse. Both medicines have known psychiatric side effects including euphoria. Individuals misusing gabapentin and The hyperbolic relationship between antidepressant dose and occupancy of their primary target receptor, the serotonin transporter, 49 suggests that the gradual reduction in the biological effect likely necessary to mitigate withdrawal symptoms requires a hyperbolic dose-reduction regimen. 12 This requires performing multiple dose reductions GMMMG Gabapentinoids - Prescribing for pain - Resource pack v. 1.1 6 • If a decision is made to prescribe gabapentinoids for unlicensed indications, the Depending on your overall health and reason for taking gabapentin, your doctor may recommend that you slowly decrease or taper the dose over time. This can help avoid withdrawal symptoms and allow your doctor to observe you and ensure you remain healthy and stable as the drug leaves your system. Tapering schedules are personalized, often reducing the dose no more frequently than once a week. Initial dose reduction should be conservative, with close monitoring of patient response. Effective coping strategies for withdrawal include relaxation techniques, counseling and medical support. A trial reduction of gabapentinoid should be considered every 6-12 months, when prescribed for chronic pain. The dose should be reduced gradually to minimise withdrawal effects and check if there is any change in your pain. Please follow your reduction plan. You may need a prescription for different strengths of medication. Initial dose: Day 1: 300 mg orally once Day 2: 300 mg orally 2 times day Day 3: 300 mg orally 3 times a day. Titrate dose as needed for pain relief; Maintenance dose: 900 to 1800 mg/day orally in 3 divided doses Maximum dose: 1800 mg per day Extended-release: Gralise (gabapentin) 24-hour extended-release tablets: Initial dose: Response to dose reduction will vary considerably between patients, depending on their starting dose and duration of use, but in general a dose reduction step should usually not exceed: 50 – 100 mg pregabalin in one week; 300 mg gabapentin in one week
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |