Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 | |
 | |
 |  |
 |  |
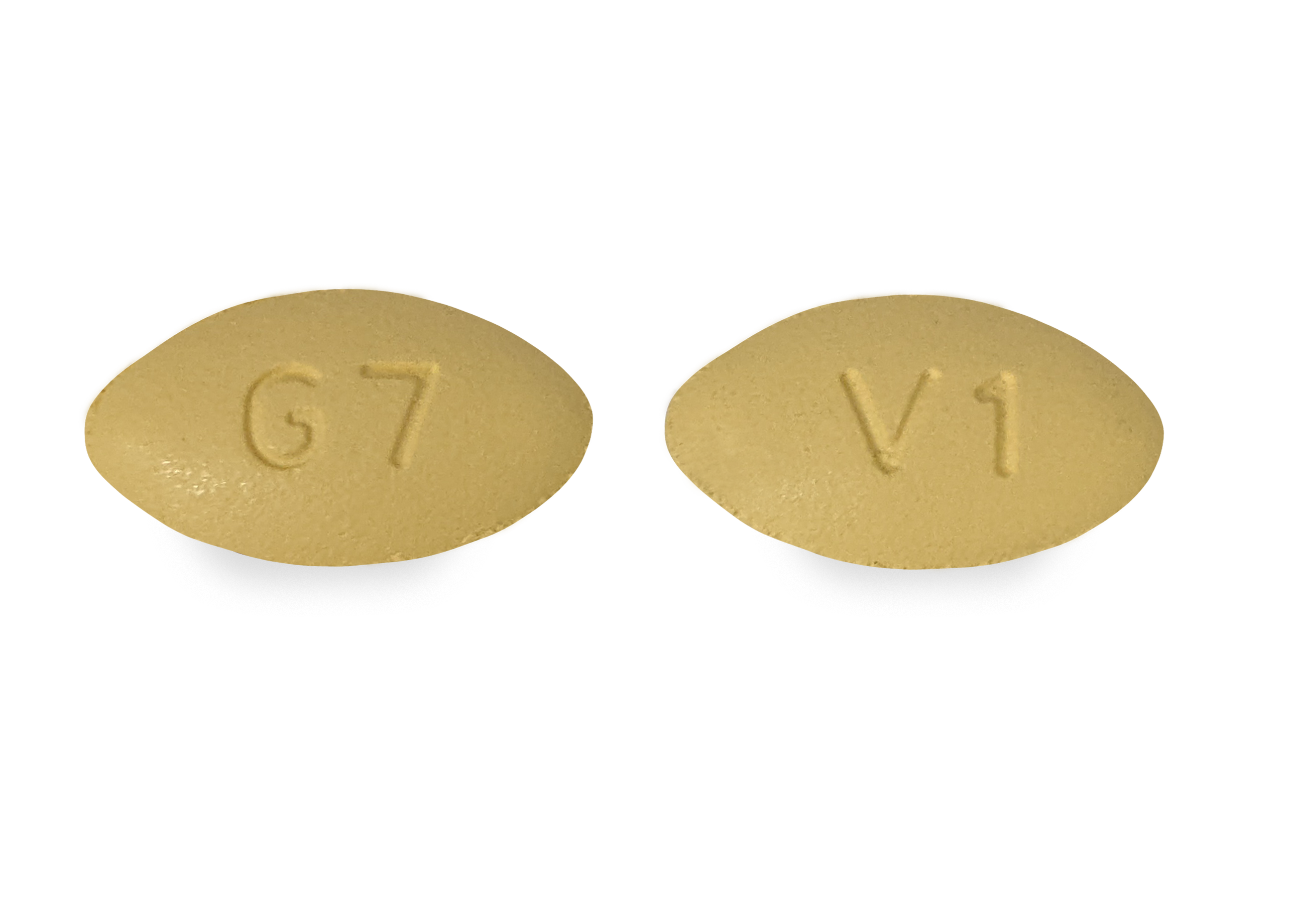 |  |
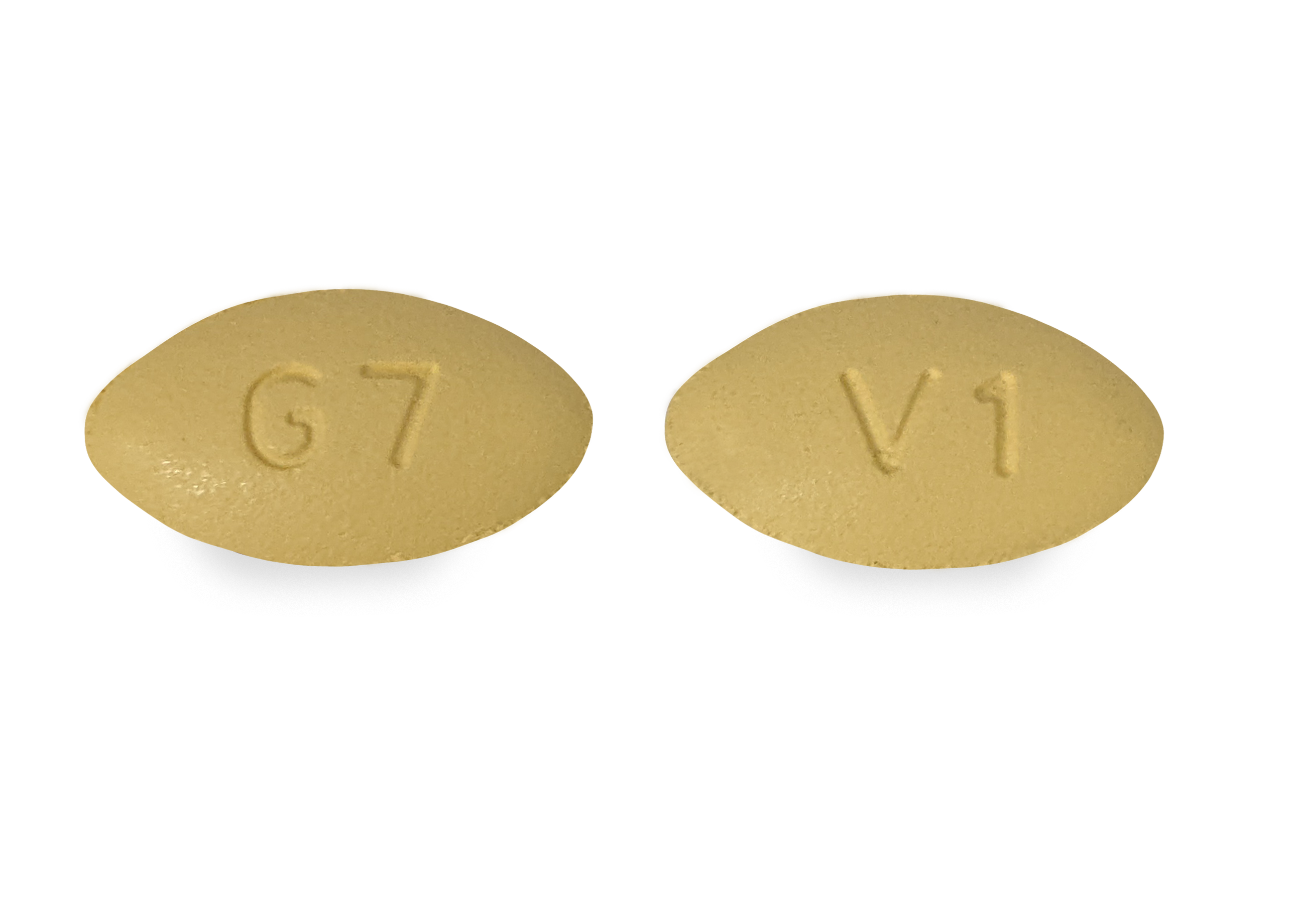
Treatment with clonazepam, gabapentin, or memantine could be considered in patients with visual symptoms from persistent seesaw nystagmus (see Table 2 for recommended dosing). Seesaw Nystagmus | alternative Seesaw Nystagmus. Periodic Alternating Nystagmus. Patients with acquired periodic alternating nystagmus often complain of oscillopsia. Pathophysiology. Due to various reasons, it is difficult to study herpes zoster pathophysiology compared to its relative, herpes simplex virus. Damage to the corneal stroma in VZV-SK has long been thought to result from inflammatory processes, rather than direct viral cytolytic activity. Improvement of SWJ has been reported with diazepam, clonazepam, phenobarbital, and valproate. Studies show MSO may benefit from gabapentin or memantine. Opsoclonus and ocular flutter may be reduced with propranolol, clonazepam, gabapentin, topiramate, levetiracetam, or ethosuximide. Surgery Amitriptyline can alleviate neck pain, insomnia, and excessive drooling, and gabapentin is useful in reducing dystonic pain. Prognosis. The prognosis for patients with PSP is poor, with the average time from onset of symptoms to death ranging from 5-9 years. The standard pharmacological treatments for ONM are membrane stabilizing agents, including carbamazepine, gabapentin, phenytoin, and lacosamide . Carbamazepine, the treatment of choice, may decrease the ephaptic transmission by interacting with different receptors and channels on the neuronal membrane and reducing the frequency of prolonged “Used off label, gabapentin can be highly effective in decreasing oscillopsia and nystagmus amplitude,” said Dr. Rucker. Optical or mechanical. In some patients, the use of prisms can stimulate convergence mechanisms, which can quiet the nystagmus pattern. The most common medications used to modify behavior include systemic neuromodulating agents like gabapentin and carbamazepine. [2] [19] Other medications that have been trialed include amitriptyline, pimozide, diazepam, tiagabine, and oxcarbazepine with varying degrees of success. Treatments of SOM include topical β-blockers, carbamazepine, oxcarbazepine, phenytoin, gabapentin, baclofen, and incisional surgery in severe cases . However, no treatment for SOM has been consistently effective, but some patients may respond to one of the treatments mentioned above [2] . Drugs can be directly toxic to the cells of the retina or the retinal pigment epithelium (RPE). The most common manifestation of injury to the retina and RPE is a pigmentary maculopathy. The gabapentinoids gabapentin and pregabalin are among the most commonly prescribed drugs in North America. Now, researchers have found an association between gabapentin and the incidence of acute angle-closure glaucoma (AAG). 1 A similar association was not found for pregabalin. Purpose: To investigate the response to gabapentin treatment in patients with dry eye (DE) accompanied by features of neuropathic ocular pain (NOP), and to analyze the differences between clinical manifestations of the groups according to treatment response. Oral gabapentin is a first-line treatment for chronic systemic neuropathic pain. Although it has been used for ocular discomfort after refractive surgery and in severe, painful dry eye syndrome (DES), it can depress the central nervous system. A prospective, randomized, controlled study evaluated three groups: one was given a placebo, one was given pregabalin 75mg orally, and was given gabapentin 300mg orally. This study did not find any significant difference in pain control . Another study evaluated post-PRK pain control with gabapentin 300mg orally versus oxycodone and acetaminophen. Epidemiology and Risk factors. Glaucoma is a form of optic neuropathy. It is usually associated with intra-ocular pressure (IOP) abnormalities, thinning of the retinal nerve fiber layer (RNFL), characteristic visual field loss, and may be categorized as open or closed angle based on the status of the iridocorneal angle. Gabapentin (GBT) is a structural analog of gamma-amino butyric acid that has been used by systemic administration to provide pain relief in glaucomatous patients. We have already shown in a rabbit model system that its topic administration as eye drops has anti-inflammatory properties. Anticonvulsants (carbamazepine, oxcarbazepine, gabapentin) and selective serotonin reuptake inhibitors also have demonstrated efficacy in the treatment of symptoms. Interventional Therapy Nerve blocks can alleviate pain temporarily; some patients have experienced pain relief lasting up to a few months post-injection [2] . The macular edema improved after discontinuing the use of the drug. If vision loss after the use of gabapentin occurs, it is prudent to identify macular edema. Gabapentin should be considered one of the potential causes of macular edema. Footnotes Disease Entity. Fungal endophthalmitis is a rare, purulent fungal infection involving the intraocular fluids (vitreous and aqueous).. Etiology and Risk Factors. The etiology depends on the mode of transmission of the fungus: The systemic pain intensity correlates with depression and PTSD correlate with the dry eye like symptoms. These patients are treated with tri-cyclic antidepressants (e.g., amytriptyline, nortriptyline), anti-convulsants (e.g. carbamazepine), NSAIDS, dronabinol, tramadol, gabapentin/pregabalin are also used with variable success. Variable success has been seen with topical beta blockers, carbamazepine, phenytoin, baclofen, gabapentin, clonazepam, mirtazapine, memantine, and surgery . Botulinum toxin injections have variable success rates and could potentially only provide temporary relief due to difficulty in isolating the superior oblique muscle from the other
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 | |
 | |
 |  |
 |  |
 |  |