Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
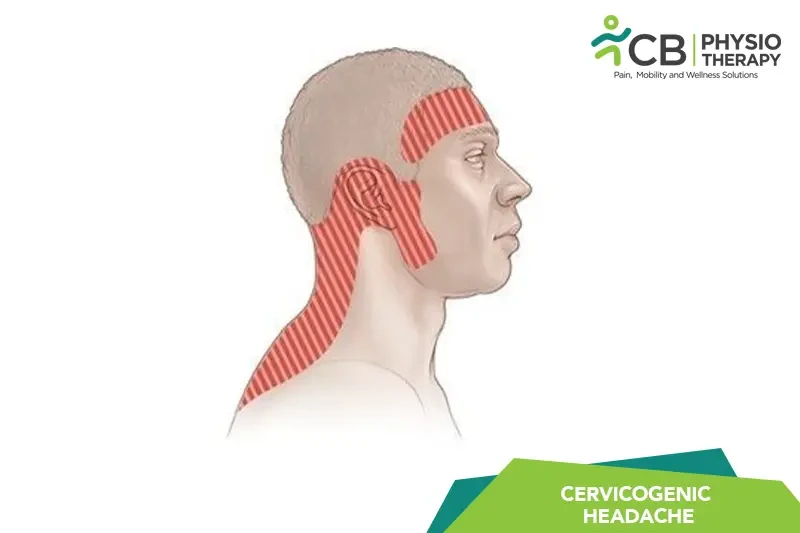
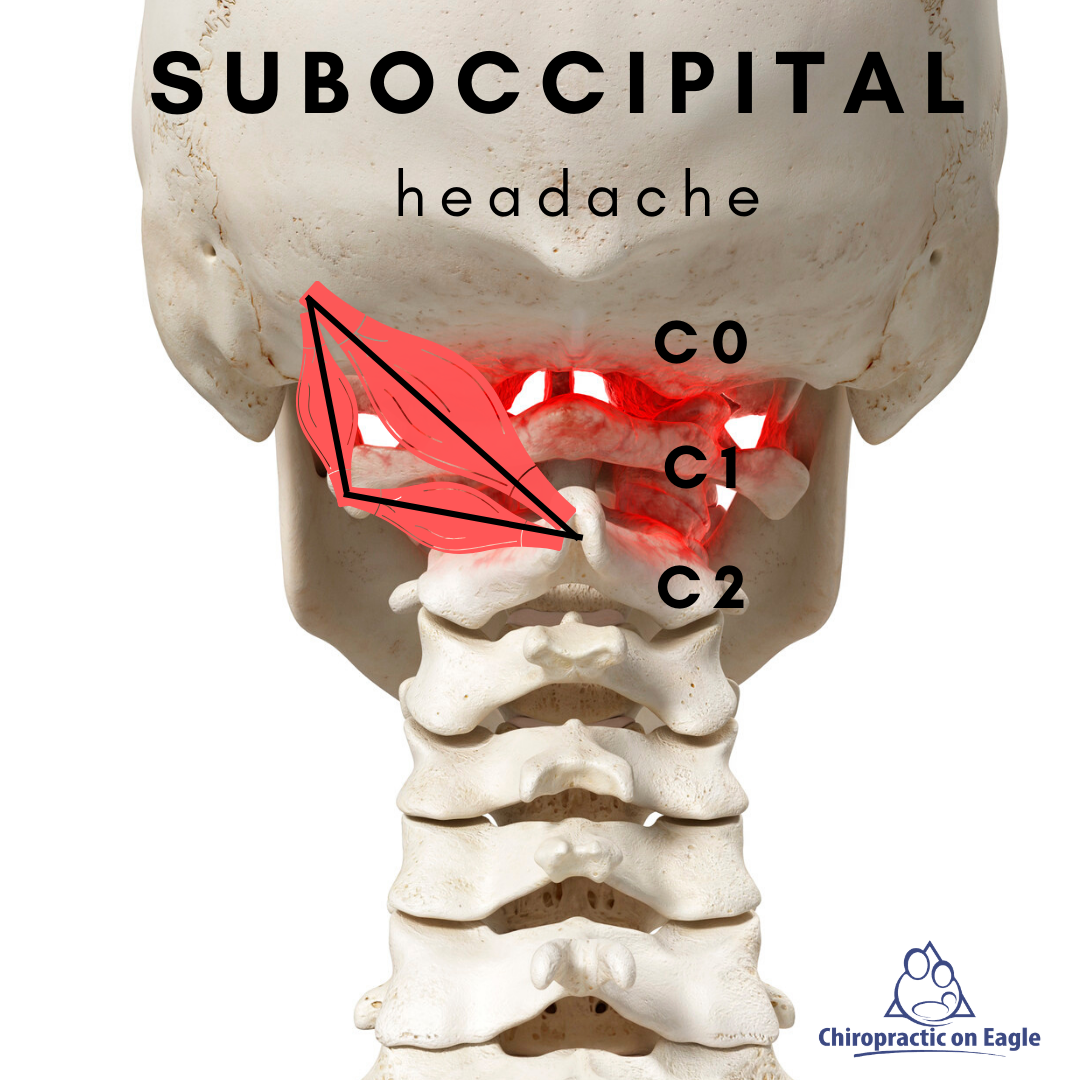
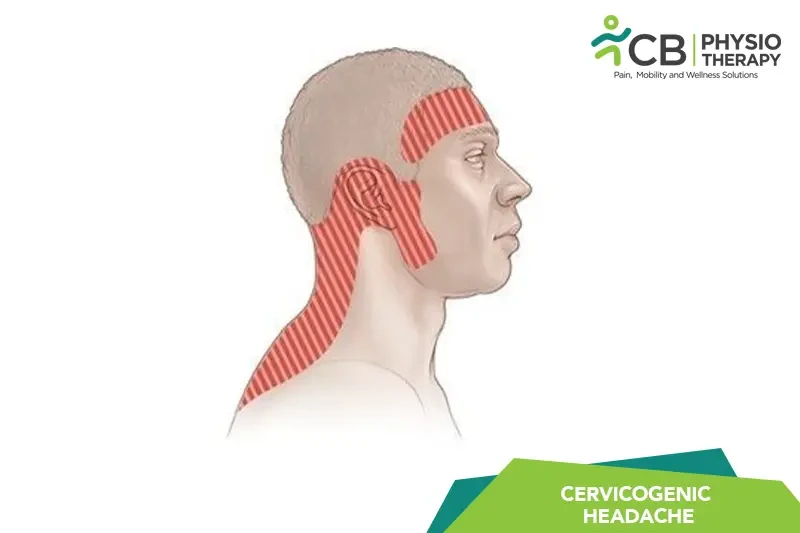
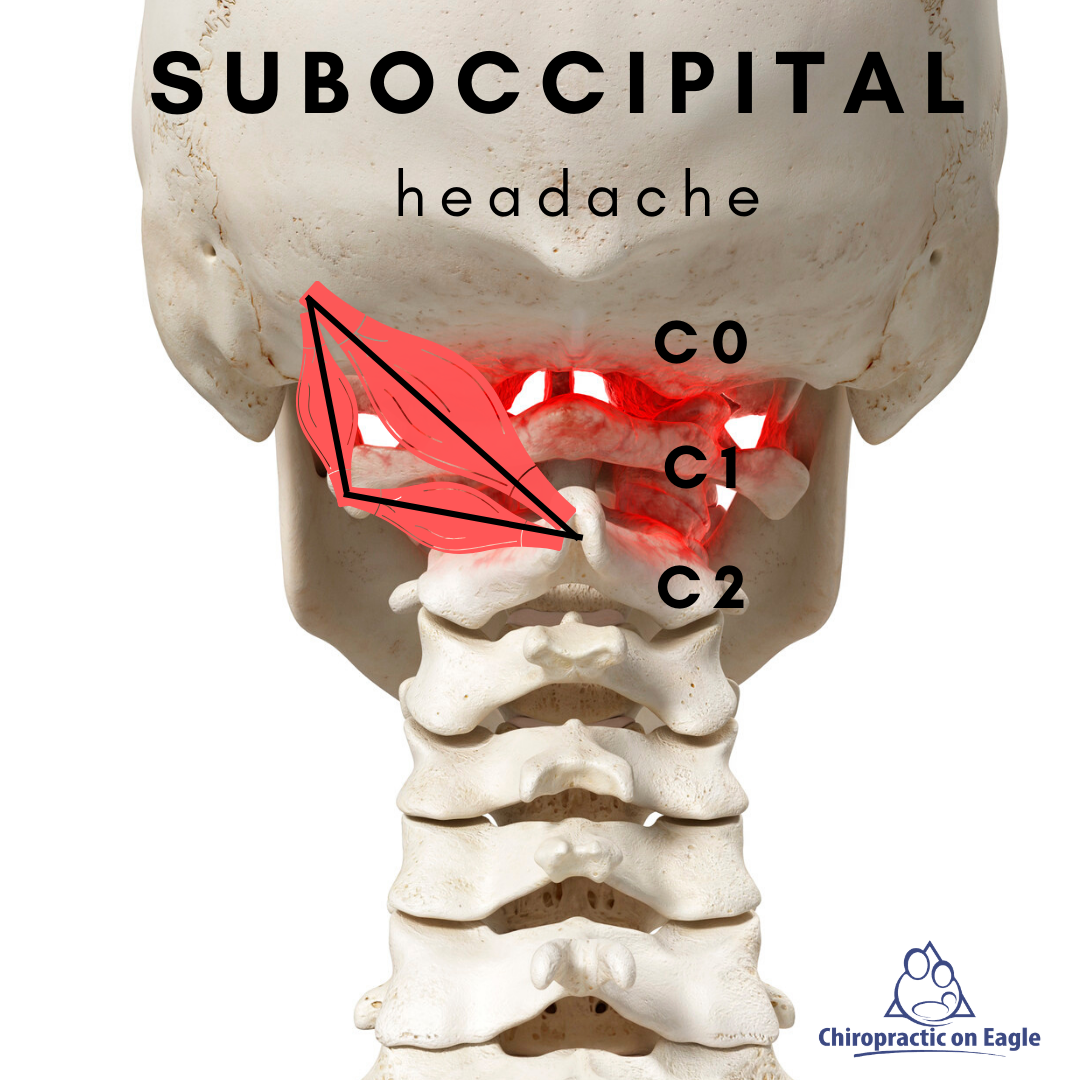
Antiseizure medications like gabapentin (Neurontin) and pregabalin (Lyrica) may provide relief. Your doctor also may prescribe duloxetine (Cymbalta), a type of antidepressant called a selective Secondary headaches are caused by an identifiable process. Cervicogenic headache, posttraumatic headache, and medication overuse headache are the most common secondary headaches. Red flag Core Tip: Cervicogenic headache (CEH) was recognized as a unique category of headache.The treatments of CEH remain controversial among different disciplines. The Chinese Association for the Study of Pain asked a multidisciplinary expert group identified the clinically relevant topics in CEH. Cervicogenic headache (CeH) is a secondary headache disorder, which presents with unilateral pain, predominantly on the occipital and upper cervical regions, and is worsened by neck movement, sustained awkward head position, or external pressure over the symptomatic side. A cervicogenic headache presents as unilateral pain that starts in the neck and is referred from bony structures or soft tissues of the neck.[1] It is a common chronic and recurrent headache that usually starts after neck movement. It usually accompanied by reduced range of motion of the neck. It could be confused with a migraine, tension headache, or other primary headache syndromes Antiepileptic drugs, such as gabapentin (Neurontin) or pregabalin (Lyrica), have low evidence and are not strongly recommended for cervicogenic headache treatment, but they may still be considered. Nonsteroidal anti-inflammatories ( NSAIDs ) have low evidence for cervicogenic headache treatment. Gabapentin (GBP), originally an antiepileptic drug, is more commonly used in the treatment of pain, including headache disorders. Off-label GBP is used in headache disorders with some success, some failure, and much debate. Some physical therapy exercises that address cervicogenic headaches are cervical spine manipulation and strengthening exercises like deep neck flexors, upper quarter muscle stretches, thoracic spine thrust manipulation, and C1-C2 self-sustained natural apophyseal glides. Here's how they work: Wade Cooper is the Medical Director of the University of Michigan Headache and Neuropathic Pain Clinic.He is an assistant professor with the departments of Neurology and Anesthesiology at the University of Michigan School of Medicine. He also serves as the fellowship director for the Headache Medicine Fellowship Program. His areas Cervicogenic headaches can interfere with how you go about your day, but you don’t have to deal with the pain forever. There are treatment options available for many different causes. Your provider will help you find one or a combination specific to your situation. We also debate the role of a new antiepileptic drug, gabapentin, in the management of headache and neck pain. It is now considered to be an emergent treatment for pain syndrome. We delineate its pharmacological, laboratory and clinical profiles, with a review of the world literature. Cervicogenic headache, posttraumatic headache, and medication overuse headache are Gabapentin (Neurontin) is minimally effective at high doses, and adverse effects are common. Medications alone are often ineffective or provide only modest benefit for cervicogenic headache. 25 Medications commonly used include antidepressants, antiepileptic drugs, analgesics, and muscle relaxants, 25 but none of these medications has been studied in controlled clinical trials. Gabapentin is a drug that’s approved to help prevent seizures in people with epilepsy and treat nerve pain from shingles. It’s also sometimes used off-label for migraine prevention. Cervicogenic headaches can be painful and debilitating. However, there are treatments available. Cervicogenic headaches typically arise when the nerves of the upper cervical spine are irritated. The pain from these headaches usually starts in the neck and spreads to one side of the head. It may also cause pain behind one or both eyes. We would like to show you a description here but the site won’t allow us. A systematic review of radiofrequency ablation and pulsed radiofrequency ablation demonstrated “very limited benefit” in the management of cervicogenic headache. 32 A 2016 review focusing solely on cervical zygapophyseal joint pain (as opposed to cervicogenic headache) found some degree of evidence for radiofrequency ablation and nerve What is a cervicogenic headache? This is a headache related to neck problems that often begins at the top of the neck and moves into the head. What are the signs and symptoms? What should I look out for? What can I do to help prevent the headaches? • Try not to sleep on your stomach. Although there are no published clinical trials for pregabalin in episodic migraine, pregabalin may be beneficial in cervicogenic headache. Both gabapentin and pregabalin have shown increased restorative sleep patterns, 39., 40. which also may play a role in chronic pain syndromes such as cervicogenic headache. Cervicogenic headache constitutes 15 to 20% of all chronic and/or recurrent headaches and is categorized as a secondary headache, meaning the condition results from an underlying disease. CGH specifically stems from a neuromusculoskeletal dysfunction of the cervical spine, particularly the upper three cervical segments.¹˒²˒³
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |