Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 | 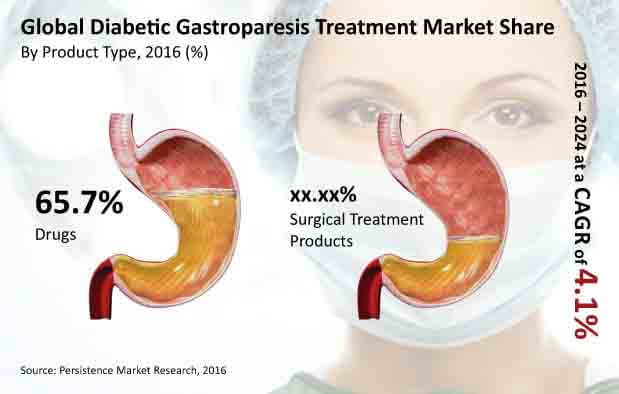 |
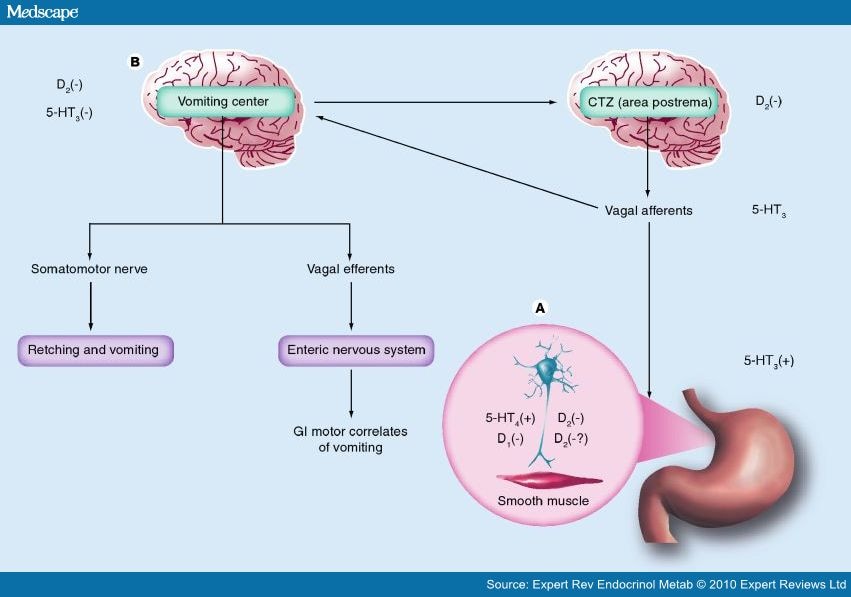
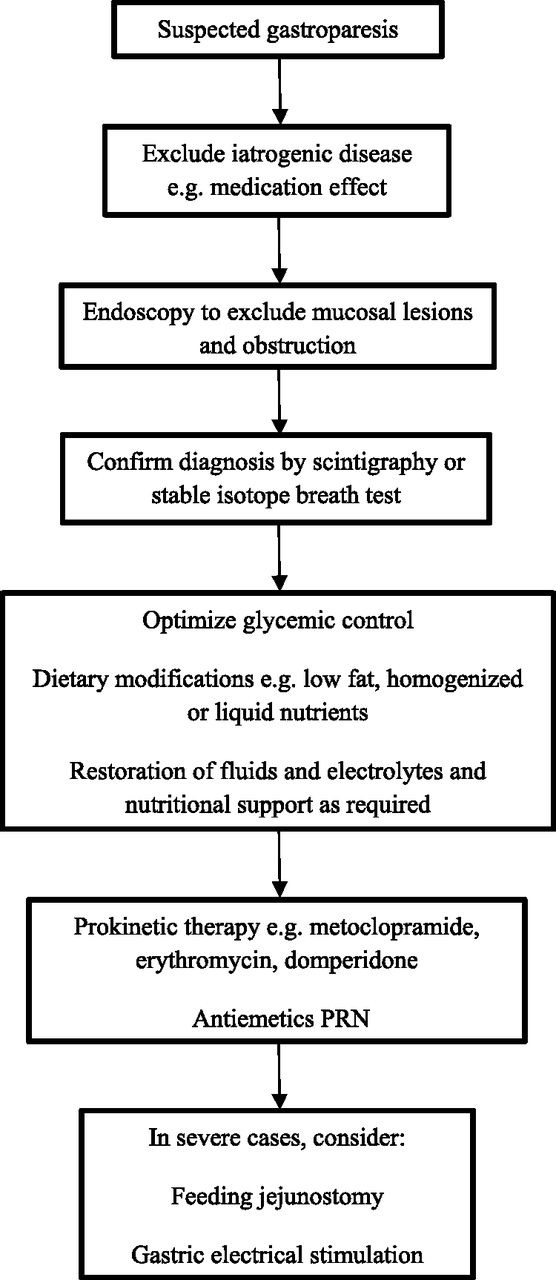
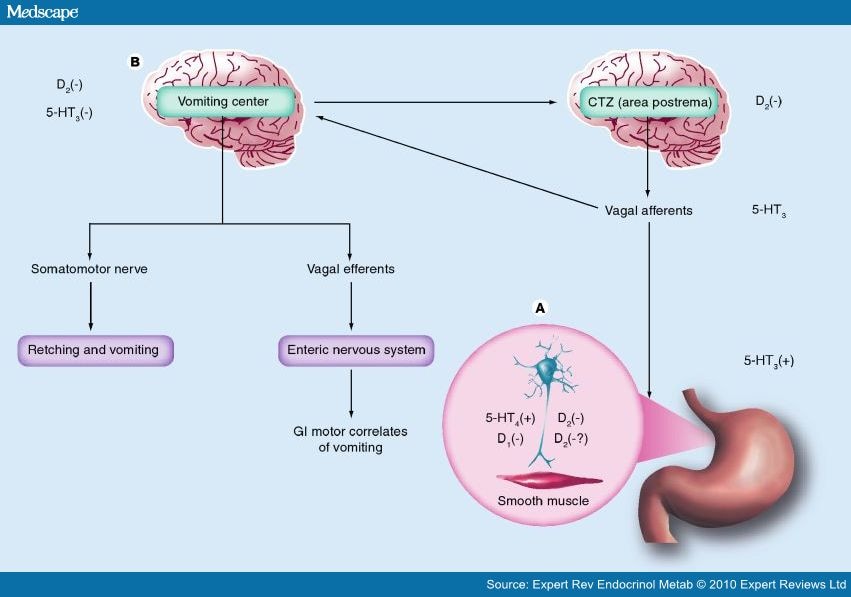
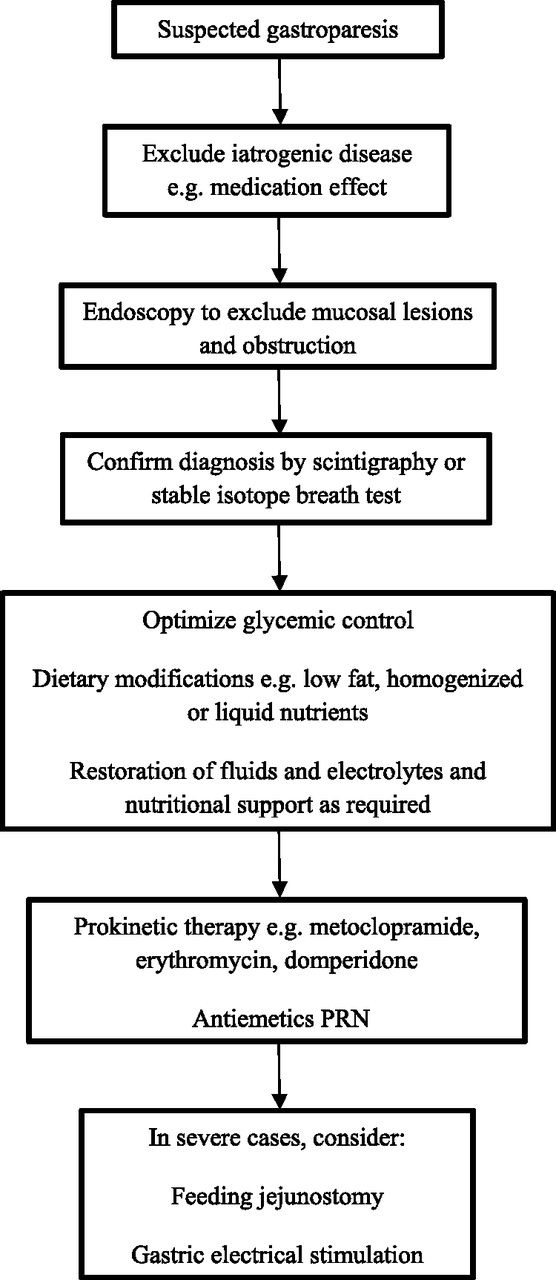
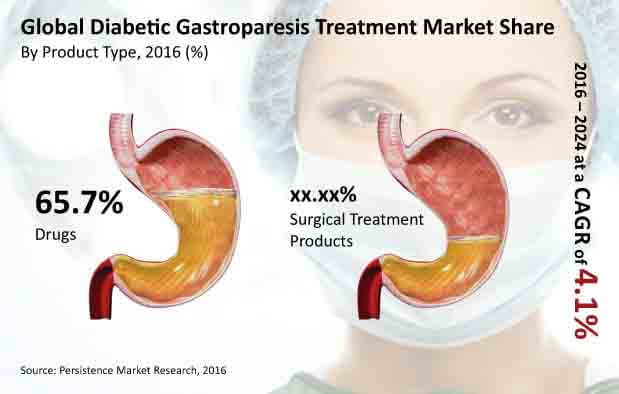
Refractory symptoms of shorter duration are more likely to respond than prolonged intractable symptoms. 53 Whether patients with refractory diabetic gastroparesis respond better than those with idiopathic gastroparesis remains controversial. 54, 57, 59 Temporary electrical stimulation may predict response to GES and should be offered if Gastroparesis can be a serious problem where the GI tract literally “slows down”. This issue is common in patients with diabetes. Bloating, abdomnial pain, nausea, vomiting, and a feeling of fullness are all possible symptoms of gastroparesis. There are also medications that can worsen gastroparesis. The case: KD is a 62 year old female who [] Although idiopathic gastroparesis is the most common form of gastroparesis, diabetes is the most common disease associated with the condition. Upper gastrointestinal symptoms are reported in 11% to 18% of patients with diabetes, most of which are associated with delayed gastric emptying. Gastroparesis, or chronic delayed gastric emptying without mechanical obstruction, affects about 40% of patients with type 1 diabetes and up to 30% of patients with type 2 diabetes. Diabetic gastroparesis (DGP) typically causes nausea, vomiting, early satiety, bloating, and postprandial fullness. Management of diabetic neuropathy should begin at the initial diagnosis of diabetes. The primary care physician needs to be alert for the development of neuropathy—or even its presence at the time of initial diabetes diagnosis—because failure to diagnose diabetic polyneuropathy can lead to serious consequences, including disability and amputation. This case report discusses 2 cases of medication-induced gastroparesis which were initially diagnosed as diabetic gastroparesis, and thorough history taking revealed the cause to be medication induced. Gastroparesis can be caused either by diseases of the stomach's muscles or the nerves that control the muscles, though often no specific cause is identified. The most common disease-causing gastroparesis is diabetes mellitus, which damages the nerves controlling the stomach muscles. miting, early satiety, postprandial fullness, bloating, and upper abdominal pain. Management of gastroparesis should include assessment and correction of nutritional state, relief of symptoms, improvement of gastric emptying and, in diabetics, glycemic control. Patient nutritional state should be managed by oral dietary modifications. If oral intake is not adequate, then enteral nutrition via Gastroparesis is characterized by delayed gastric emptying in the absence of mechanical obstruction. This complication is associated with uncontrolled diabetes, contributing to approximately one-third of all gastroparesis cases (1 – 3). Gastroparesis is more prevalent in patients with type 1 diabetes than in those with type 2 diabetes (4). I'm on gabapentin (ostensibly) for my gastroparesis and have been for a number of years. I started at 25 mg three times a day, and gradually bumped up. My current dose is 800 mg once a day. The sleepiness was awful for the first week or so, and then again after each dose bump. Gabapentin binds to the α-2 δ subunit of voltage-gated calcium channels preventing release of nociceptive neurotransmitters including substance P, norepinephrine, and glutamate. It is used as an effective analgesic for patients with neuropathic pain and chronic pain syndromes. Gabapentin is approved for diabetic peripheral neuropathy [73], [74]. Anticholinergics are one of the most common medication classes that “slow down” the GI tract which could obviously be a problem in this case. Looking into alternatives (depending upon the indication and benefit of amitriptyline) like SSRI’s (if depression), SNRI’s, or possibly increasing the gabapentin would all be potential options. erspectives on the risk factors, diagnosis, and management of gastroparesis in adults (including dietary, pharmacological, device, and interventions directed at the pylorus), and they represent the official practice recommendations of the American College of Gastroenterology. The scientific evidence for these guidelines was assessed using the Grading of Recommendations, Assessment, Development Idiopathic gastroparesis is the most common form, whereas diabetes accounts for approximately one-third of all cases of gastroparesis. 2 Other causes of nausea, vomiting, and postprandial distress symptoms (eg, early satiety, postprandial fullness, and epigastric pain) are excluded by standard endoscopy, routine laboratory studies, and computed Management of gastroparesis should include assessment and correction of nutritional state, relief of symptoms, improvement of gastric emptying and, in diabetics, glycemic control. Patient nutritional state should be managed by oral dietary modifications. Delayed gastric emptying on objective testing defines gastroparesis, but symptoms overlap with functional dyspepsia and do not correlate well with gastric emptying delay. This review outlines a strategy for defining, diagnosing, and managing refractory gastroparesis. improvement in symptoms and resolution of gastroparesis. Further research needs to be done to assess the frequency of misdiagnosing diabetic patients with gastroparesis due to medications, specifically glucagon-like peptide-1 receptor agonists which are increasingly being used in diabetics. Keywords gastroenterology, gastroparesis The pathophysiology behind gastroparesis is varied and depends on disease etiology. Vagal and/or autonomic neuropathy play an important role in the development of diabetic gastroparesis, and it is estimated to occur in up to 20% to 40% of patients with diabetes. Gastroparesis can cause problems with blood sugar levels and nutrition. Diabetes is among the most common causes of gastroparesis. Glucagon-like peptide-1 receptor analogues are medications that control diabetes (especially postprandial hyperglycemia). GLP-1 agonists delay gastric emptying. Diabetic gastroparesis is reported as a side effect among people who take Gabapentin (gabapentin), especially for people who are female, 60+ old, also take Lantus, and have Gastroesophageal reflux disease.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |