Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
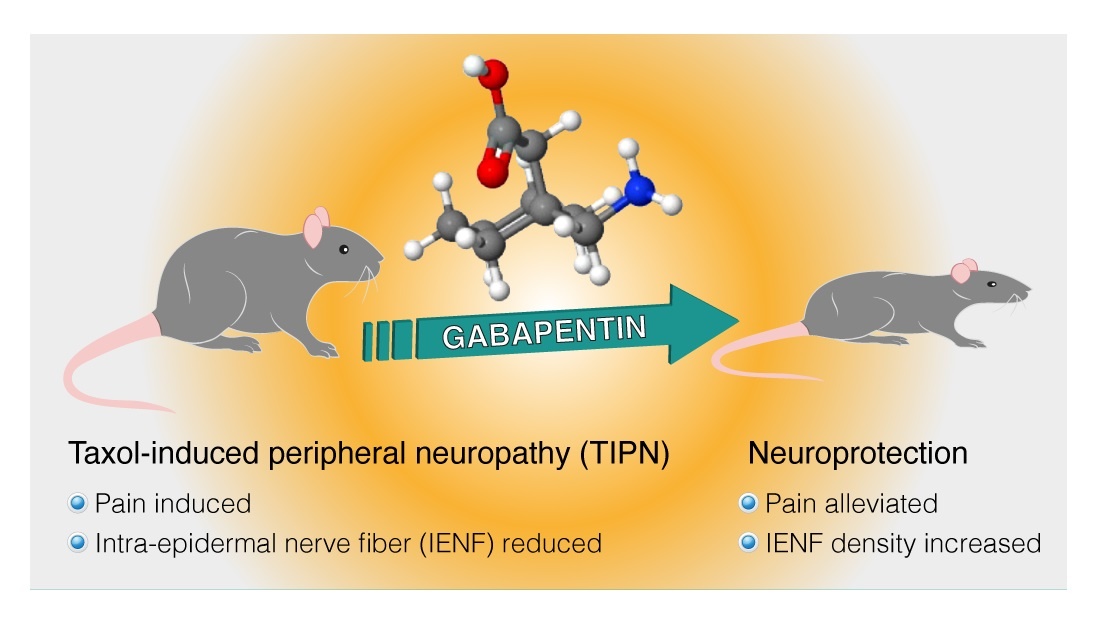
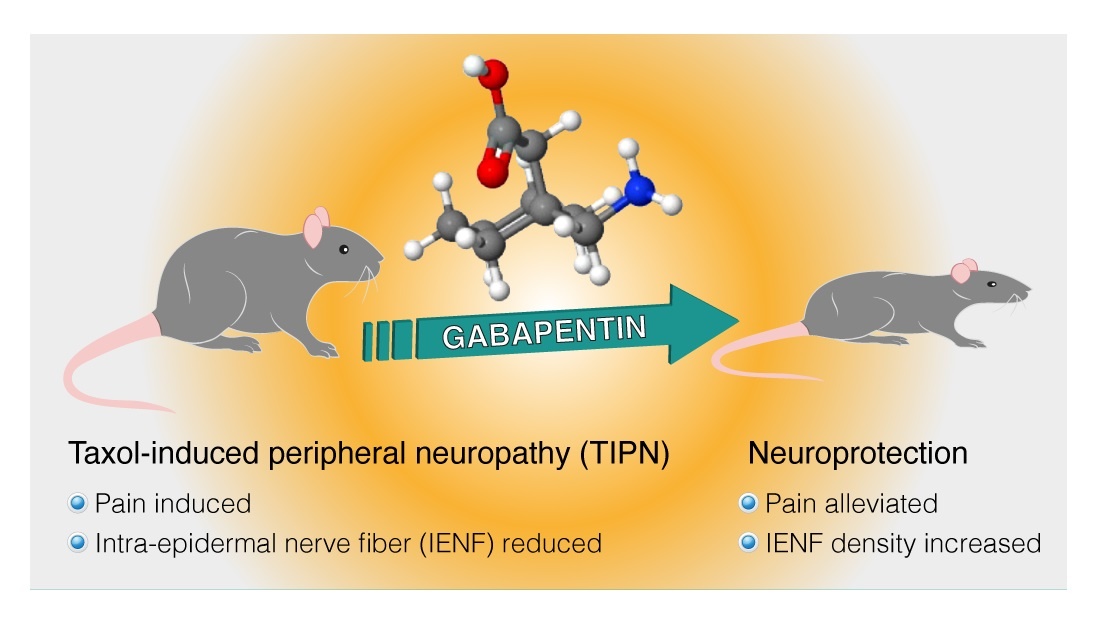
Compared with the control group, gabapentin therapy led to a statistically significant better response in patients of each baseline neurotoxicity group. Conclusions: Gabapentin monotherapy seems to be well tolerated and useful for the management of chemotherapy-induced neuropathic pain. Chemotherapy-induced neuropathy is a serious clinical problem caused by a substantial number of cytotoxic drugs, including taxanes, platinums, vinca alkaloids, epothilones, eribulin, and bortezomib; these drugs cause different pathologic insults to neurons. Chemotherapy-induced peripheral neuropathy (CIPN) affects between 40% and 70% of individuals undergoing chemotherapy and may significantly affect quality of life by worsening symptomatic clusters, such as psychological distress, fatigue-related pain, and abdominal discomfort.¹˒² On the basis of these data, a multicenter, double-blind, placebo-controlled, crossover, randomized trial was conducted to evaluate the effect of gabapentin on symptoms of chemotherapy-induced peripheral neuropathy (CIPN). On the basis of these data, a multicenter, double-blind, placebo-controlled, crossover, randomized trial was conducted to evaluate the effect of gabapentin on symptoms of chemotherapy-induced peripheral neuropathy (CIPN). This topic review will cover approaches to prevention and treatment of CIPN focusing mainly on platinum drugs, taxanes, vinca alkaloids, and bortezomib. An ongoing phase III study is evaluating the efficacy of oral gabapentin in preventing paclitaxel-induced neuropathy.33 Some experts recommend integrated care approaches, such as acupuncture, exercise and scrambler therapy, for treatment and prevention. Neuropathy is a dose limiting side effect of taxanes which may impact the quality of life and treatment outcomes. This randomized placebo-controlled double-blinded clinical trial was carried out to assess the efficacy of gabapentin in preventing chemotherapy induced neuropathy. Women with breast can After completion of chemotherapy treatments, paclitaxel neuropathy, on average, improves over the ensuing several months. In contrast, oxaliplatin-induced neuropathy, on average, worsens for 2-3 months after cessation of therapy (labeled as coasting phenomenon); after approximately 3 months, neuropathy tends to improve.3 Neuropathy in the When peripheral neuropathy occurs due to chemotherapy treatment, it is termed Chemotherapy-induced peripheral neuropathy (CIPN) [1], [2], [5]. CIPN is a frequent adverse effect of anticancer agents most commonly presenting with sensory symptoms more than motor symptoms in a symmetrical “glove and stocking” distribution [3], [4], [5], [6]. In a recent study using a mouse model of paclitaxel-induced peripheral neuropathy, a fenofibrate-enriched diet did show promise in that it had some ability to prevent the development of mechanical hypersensitivity, prevented cold hypersensitivity, and prevented a reduction in sensory nerve action potential in mice treated with four Chemotherapy-induced peripheral neuropathy (CIPN) is a common dose-limiting side effect experienced by patients receiving treatment for cancer. Approximately 30–40% of patients treated with neurotoxic chemotherapy will develop CIPN and there is When peripheral neuropathy occurs due to chemotherapy treatment, it is referred to as chemotherapy-induced peripheral neuropathy (CIPN). Typically, symptoms are sensory rather than motor and include reduced feeling and heightened sensitivity to pressure, pain, temperature, and touch. Efficacy of gabapentin in the management of chemotherapy-induced peripheral neuropathy: a phase 3 randomized, double-blind, placebo-controlled, crossover trial (N00C3). Cancer 110 (9), 2110–2118. 10.1002/cncr.23008 [ DOI ] [ PubMed ] [ Google Scholar ] Chemotherapy-induced peripheral neuropathy (CIPN) is one of the most disabling and demoralizing problems that arise for cancer survivors. When investigating symptoms of numbness, tingling, or pain in the extremities, it is critical to determine whether the problem is neuropathic, somatic, or mixed. In the 6 months following the initiation of chemotherapy, gabapentin was used by (i.e., dispensed to or administered to) 7.1% of patients in the neurotoxic chemotherapy group and 1.7% of patients in the non-neurotoxic chemotherapy group (relative risk: 4.2 (95% CI: 4.0-4.3) for neurotoxic vs. non-neurotoxic chemotherapy). Agents such as glutathione, mangafodipir and duloxetine are expected to be effective for CIPN intervention, while Ca/Mg infusion and venlafaxine, tricyclic antidepressants, and gabapentin dis-play limited efficacy for preventing and alleviating CIPN. Taxol-induced neuropathy was expressed by 80% and 73% reduction in the paw density of IENFs and CGPR, and gabapentin treatment corrected by 83% and 46% this reduction, respectively. Paclitaxel and carboplatin treated patients may benefit from gabapentin therapy in chemotherapy-induced peripheral neuropathy. Chemotherapy substantially deteriorates the neurologic condition of the patients and the quality of life. The combination of “chemotherapy-induced peripheral neuropathy” and each of the following keywords were used to search for CIPN treatment: “calcium and magnesium”, “goshajinkigan”, “duloxetine”, “vitamin B12”, “pregabalin”, “gabapentin”, and “pancreatic cancer”.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |