Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
/GettyImages-758308071-b4e2f5958ec34d1f927787d0250d0eed.jpg) | |
 |  |
:max_bytes(150000):strip_icc()/GettyImages-1277767392-6d7f3a50a8b74459ae2db1a3b17041ab.jpg) |  |
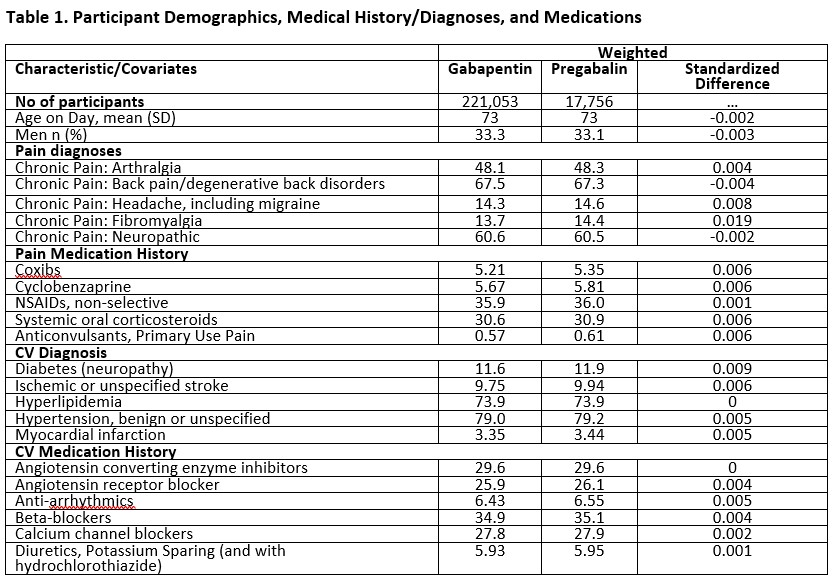
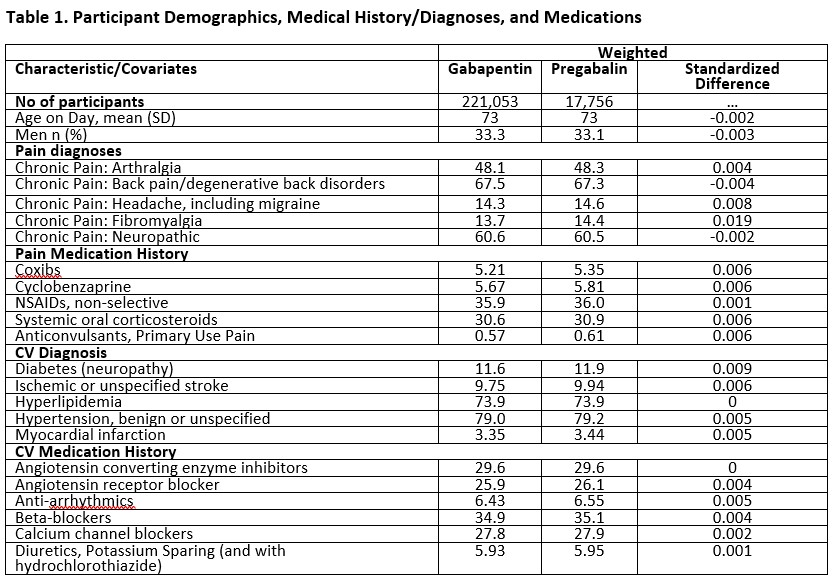
In patients with diabetic neuropathy who were prescribed gabapentin and pregabalin, there is an increased risk for heart failure, myocardial infarction, peripheral vascular disease, stroke, deep venous thrombosis, and pulmonary embolism with long-term use. There were significant associations between short-term (3 month) gabapentin use and heart failure, myocardial infarction, peripheral vascular disease, deep venous thrombosis, and pulmonary embolism. Short-term (3 month) pregabalin use was associated with deep venous thrombosis, peripheral vascular disease. Conclusion Heart failure tends to occur early, within days after the onset of treatment with gabapentin or pregabalin. The characteristics, dose dependence, genetic predisposition, pathophysiology and the type of HF remain to be clarified. Several studies involving gabapentin and its congener pregabalin have demonstrated that these agents may rarely cause acute congestive Heart Failure (HF) in patients with and without compensated HF [1,4]. To the best of our knowledge, this is the first reported young patient with new-onset Afib development associated with gabapentin therapy. Age, high body mass index (> 30 kg/m 2), height, alcohol consumption (> 1 drink/day), caffeine consumption (> 3 cups/day), hypertension, left ventricular hypertrophy, diabetes mellitus, obstructive sleep apnea, myocardial infarction, heart failure, smoking Secondary analyses stratified for baseline history of heart failure yielded similar findings. Conclusion: In a large cohort of older patients with a seizure disorder, pregabalin was not associated with an increased risk of heart failure relative to gabapentin. The goal was to determine whether the prescription of gabapentin and pregabalin in patients with fibromyalgia increases the risk of adverse cardiovascular events, including peripheral vascular disease, strokes, myocardial infarcts, heart failure, deep venous thrombosis, and pulmonary embolism. While the mechanism by which gabapentinoids may affect the heart is unclear, the authors concluded that “At this time, we recommend that gabapentin and pregabalin be prescribed with caution in the setting of heart failure.” For more information visit wiley.com. Gabapentin is a commonly used medication used as an anti-convulsant or analgesic. The well-known side-effects of gabapentin are dizziness, drowsiness and fatigue. In rare cases, it can lead to development of new onset congestive heart failure (CHF) or decompensation of pre-existing CHF. Several studies involving gabapentin and its congener pre-gabalin have demonstrated that these agents may rarely cause acute congestive Heart Failure (HF) in patients with and with-out compensated HF [1,4]. Heart failure tends to occur early, within days after the onset of treatment with gabapentin or pregabalin. The characteristics, dose dependence, genetic predisposition, pathophysiology and the type of HF remain to be clarified. Drugs may cause or exacerbate HF by causing direct myocardial toxicity; by negative inotropic, lusitropic, or chronotropic effects; by exacerbating hypertension; by delivering a high sodium load; or by drug-drug interactions that limit the beneficial effects of HF medications. Despite the lack of any published evidence, the New York Heart Association issued a warning about using caution when prescribing pregabalin to type III-IV heart failure patients. Though the effect mechanisms of pregabalin and gabapentin are not well known, the calcium channel relationship may lead to these side effects. Two patients were switched from pregabalin to gabapentin, with one recurrence of heart failure symptoms on gabapentin. Clinicians should consider pregabalin a potential contributor to worsening heart failure symptoms regardless of the time between pregabalin initiation and heart failure symptom onset and even in patients without a history of There were significant associations between short-term (3 month) gabapentin use and heart failure, myocardial infarction, peripheral vascular disease, deep venous thrombosis, and pulmonary embolism. Short-term (3 month) pregabalin use was associated with deep venous thrombosis, peripheral vascular disease. Introduction: Gabapentinoids are ligands of the α2-δ subunit of voltage-gated calcium channels (Cav) that have been associated with a risk of peripheral edema and acute heart failure in connection with a potentially dual mechanism, vascular and cardiac. Abstract. Gabapentin (GBP), a GABA analogue, is primarily used as an anticonvulsant for the treatment of partial seizures and neuropathic pain. Whereas a majority of the side effects are associated with the nervous system, emerging evidence suggests there is a high risk of heart diseases in patients taking GBP. Results: We observed 33 patients with worsening heart failure among users of pregabalin [incidence rate (IR) 105.7 per 1000 person-years] versus 43 patients among users of gabapentin (IR 133.8 per 1000 person-years), corresponding to an HR of 0.79 [95% confidence interval (CI) 0.50-1.23]. All cases of peripheral edema or heart failure involving gabapentin or pregabalin reported to the French Pharmacovigilance Centers between January 1, 1994 and April 30, 2020 were included to describe their onset patterns (e.g., time to onset). We hypothesize that there is an increased risk of heart failure or edema in individuals receiving pregabalin compared to placebo or gabapentin. To investigate this further, we will conduct a systematic review of pregabalin across all available studies.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
/GettyImages-758308071-b4e2f5958ec34d1f927787d0250d0eed.jpg) | |
 |  |
:max_bytes(150000):strip_icc()/GettyImages-1277767392-6d7f3a50a8b74459ae2db1a3b17041ab.jpg) |  |