Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
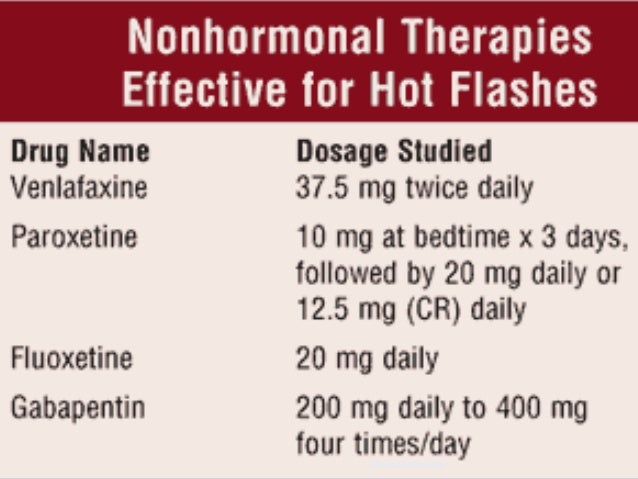 |
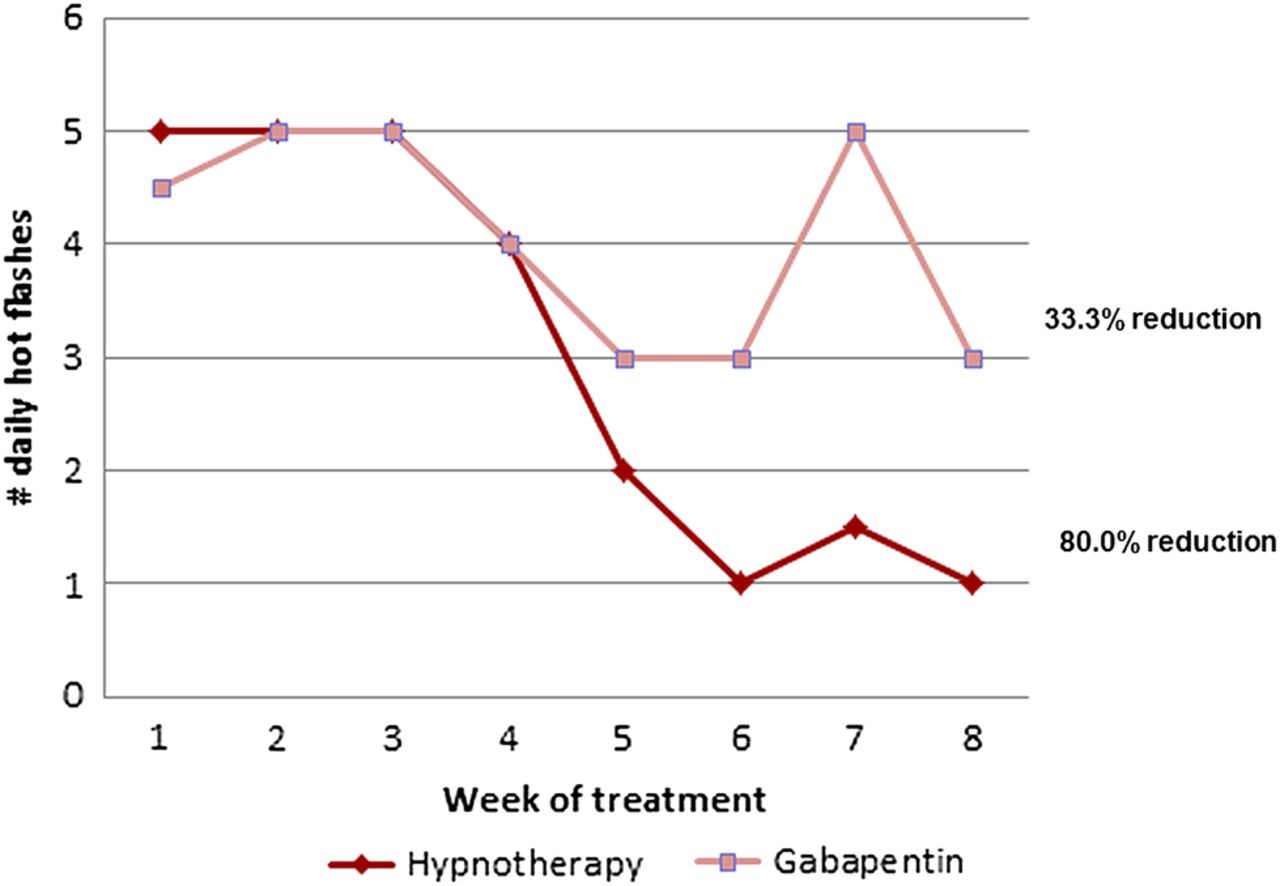
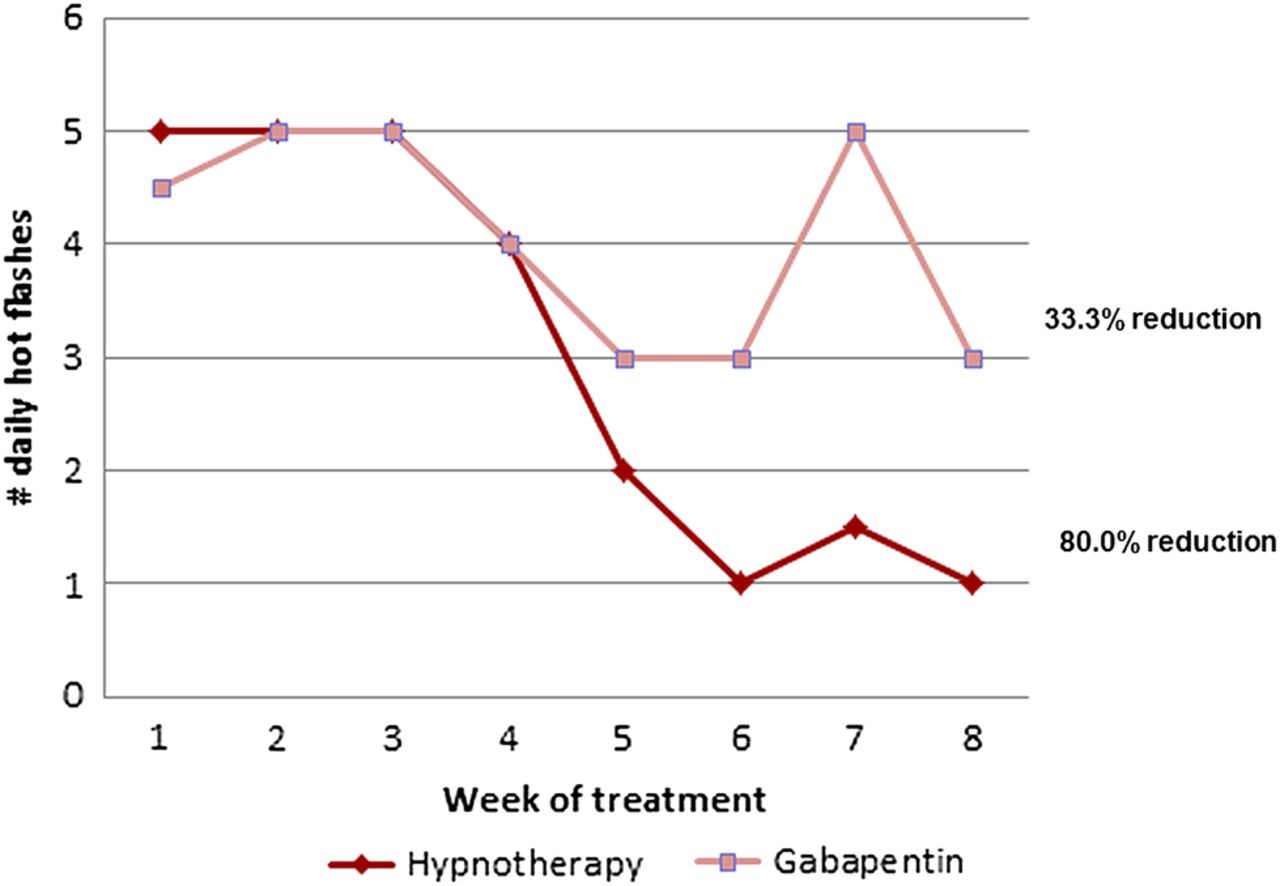
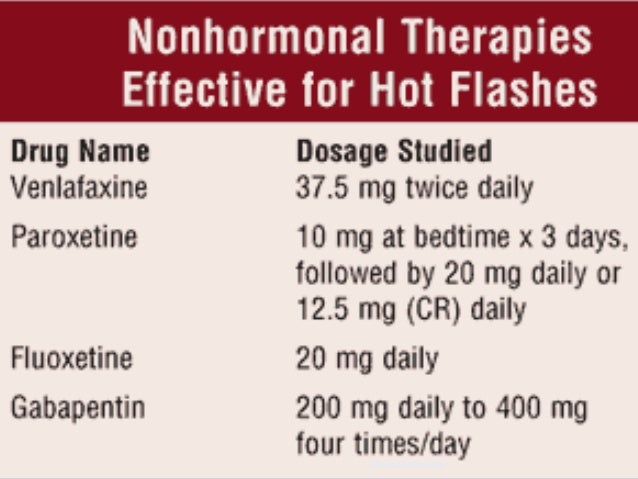
Purpose: Nonhormonal pharmacologic interventions are recommended for the treatment of hot flashes in breast cancer survivors. Antidepressants and gabapentin have been shown to be both effective and well tolerated; however, it is not clear which is preferred. Hot flashes occur frequently in menopausal women and in women with breast cancer, diminishing their quality of life. A report from the Women's Health Initiative published in 2002 raised concerns about the long-term safety of estrogen therapy. As a result, nonhormonal alternatives have emerged as pre Gabapentin is a GABA analogue used in the treatment of epilepsy, neurogenic pain, restless-leg syndrome, essential tremor, bipolar disorder, and migraine prophylaxis; it was first reported for its effects on hot flashes in five women and one man. 19 A randomised double-blind, placebo-controlled trial has shown that gabapentin is effective in Gabapentin appears to be effective for the treatment of hot flushes with a favorable effect on quality of sleep. Vitamin E has only marginal effect on vasomotor symptoms. VMS are reported in more than 80% of women receiving tamoxifen or AIs, with hot flashes being the most bothersome symptom. 1 Normally, standard of care for VMS is menopausal hormone therapy (MHT) with estrogen-based therapy. 3 However, personal history of estrogen-sensitive cancers is an absolute contraindication for patients on endocrine 420 women with breast cancer who were having two or more hot flashes per day were randomly assigned placebo, gabapentin 300 mg/day, or gabapentin 900 mg/day by mouth in three divided doses for 8 weeks. Gabapentin was further validated as a treatment for hot flashes in breast cancer survivors, including women already taking an antidepressant. 23–25 In a definitive study of 420 women who were randomised to receive gabapentin 300 mg/day, gabapentin 900 mg/day or placebo, the 900 mg/day dose of gabapentin was the most effective, decreasing the A 900-mg daily dose of gabapentin was associated with significant decreases in hot flash severity and frequency, but a 300-mg daily dose of the drug was not, results from a randomized, double-blind, placebo-controlled trial have found. Keywords: Breast cancer, Hot flashes, Vasomotor symptoms, Treatment, Non-hormonal, Randomized, controlled trials. Introduction. Hot flashes are highly prevalent and persistent among breast cancer survivors . Hot flashes are symptoms of estrogen deprivation that are exacerbated by anti-estrogen therapy used for breast cancer treatment [2, 3]. The most effective nonestrogenic agents for treating hot flashes, studied to date, are progesterone analogs. Low doses of megestrol acetate (20-40 mg orally/d) or medroxyprogesterone acetate (400-500 mg intramuscularly as a single dose, that can be repeated months later if effects wear off) decrease hot flashes to a similar degree to what is seen with estrogen. 20,22,31,32 Clinically, these This evidence-based review synthesizes and updates the findings of the highest quality evidence-based studies of interventions to manage hot flashes resulting from cancer therapies in patients with breast or prostate cancer since the initial Putting Evidence Into Practice review of hot flashes in 2011. A 2005 study by Pandya et al. randomized 420 women with breast cancer and experiencing at least 2 hot flashes in 24 hours to one of three groups: gabapentin 300 mg daily, gabapentin 900 mg daily, or placebo 23. After 8 weeks, the 300 mg dose group showed a modest 20% reduction in hot flashes, but the 900 mg dose group showed a reduction of Hot flashes, also called hot flushes, occur in approximately two-thirds of postmenopausal women with a history of breast cancer and are associated with night sweats in 44% of these women. [2, 3] The severity of hot flashes in patients with breast cancer has been associated with sleep difficulty, higher pain severity, and poor psychological funct Purpose: Hot flashes are a common and debilitating symptom among survivors of breast cancer. This study aimed at evaluating the effects of electroacupuncture (EA) versus gabapentin (GP) for hot flashes among survivors of breast cancer, with a specific focus on the placebo and nocebo effects. Hot flashes can be a prominent problem in women with breast cancer. 1–3 In lieu of concerns regarding the use of hormonal therapies in these women, nonhormonal means of alleviating hot flashes are desirable. The study led by Kishan J. Pandya, MD, found that gabapentin is effective in the control of hot flashes at a dose of 900 mg/day, but not the lower dose of 300 mg/day. “This drug should be considered for treatment of hot flashes in women with breast cancer,” he said. We undertook a randomised, double-blind, placebo-controlled, multi-institutional trial to assess the efficacy of gabapentin in controlling hot flashes in women with breast cancer. alence of hot flashes in women treated for breast cancer range from 51% to 81% (Fisher et al., 2013). In addition, almost 80% of men with prostate cancer treated with androgen deprivation therapies (ADTs) (i.e., drugs or orchiectomy) are reported to experi-ence hot flashes, which can persist for years (Qan’ir et al., 2019). Hot flashes (HFs) occur in about 75% of women at midlife, interfering with many spheres of life and overall quality of life (QoL) (1,2).Breast cancer survivors are at higher risk for long-term and more severe HFs as a consequence of chemotherapy-induced menopause, ovarian function suppression, and the use of tamoxifen or aromatase inhibitors (). Based on the pharmacology of gabapentin, a relationship between exposure and anxiety was hypothesized and specified a priori in the design of a double-blinded, placebo-controlled trial of gabapentin for the treatment of hot flashes in breast cancer patients: Gabapentin for the Control of Hot Flashes in Women with Breast Cancer (ClinicalTrials
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |