Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 | 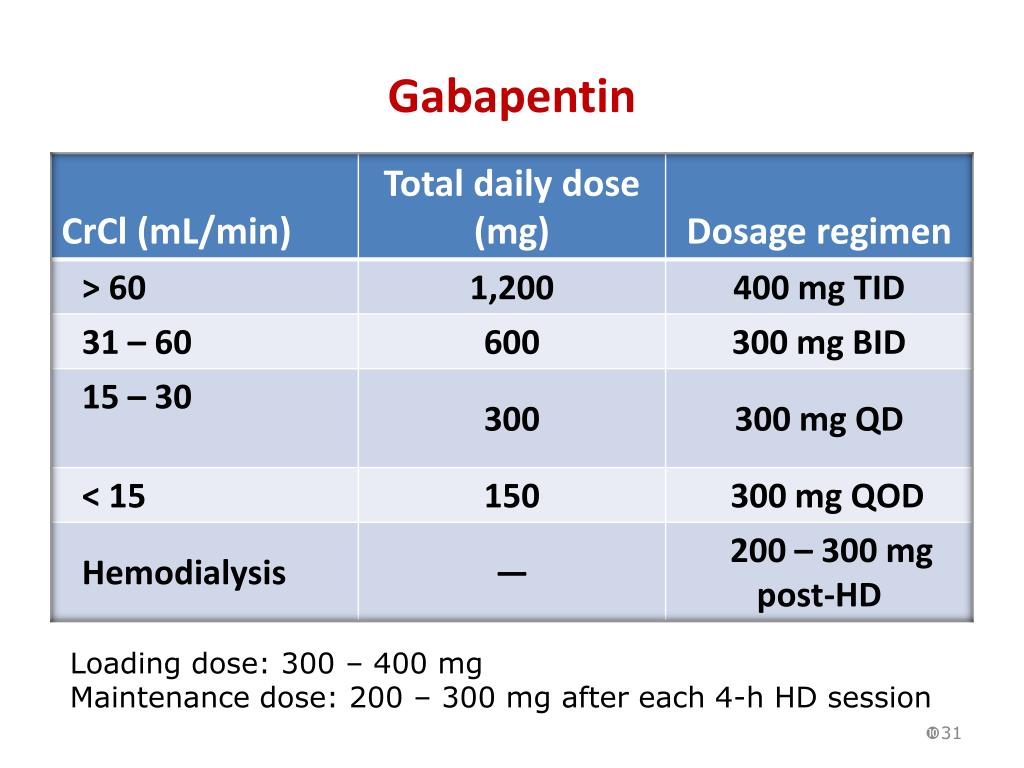 |
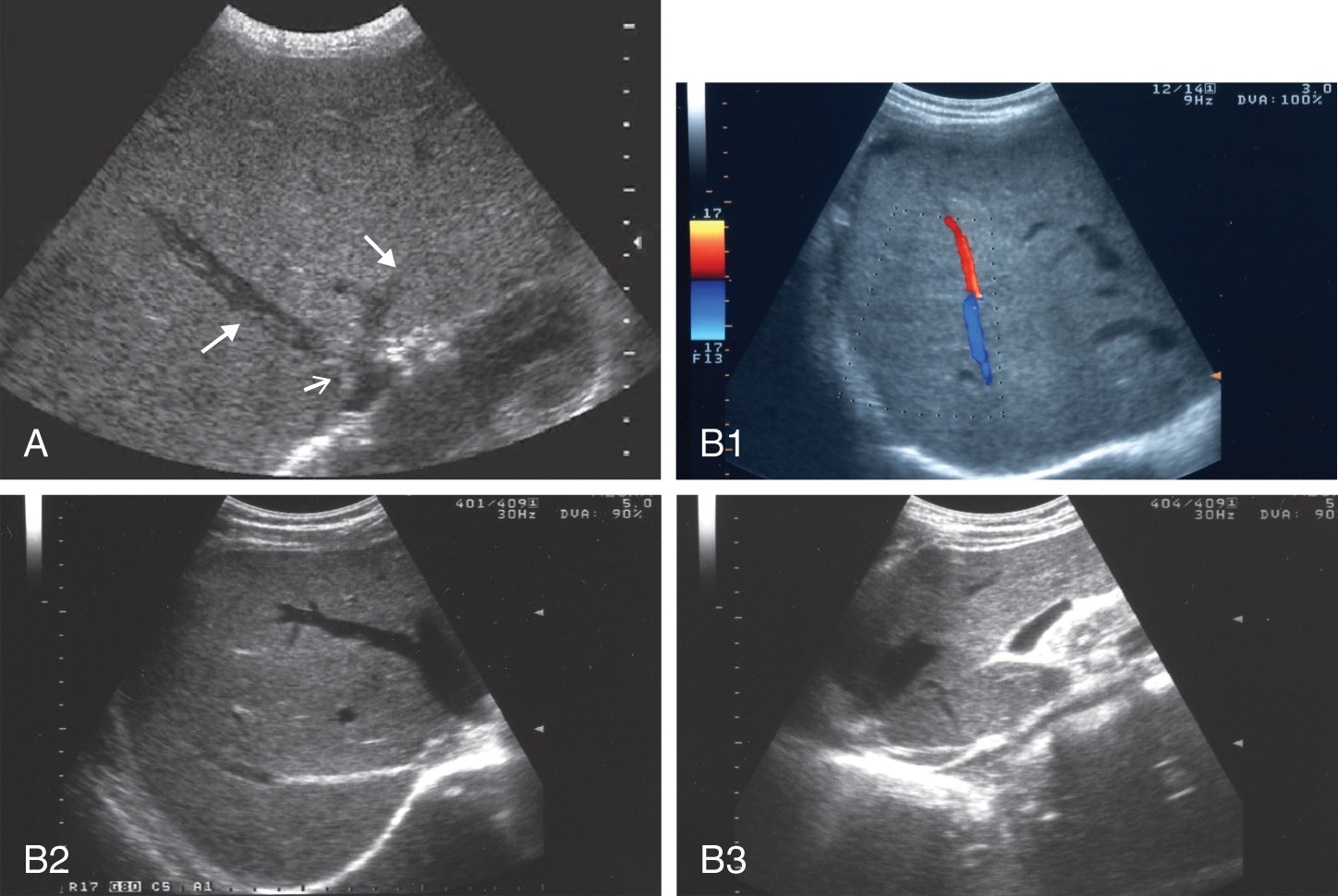
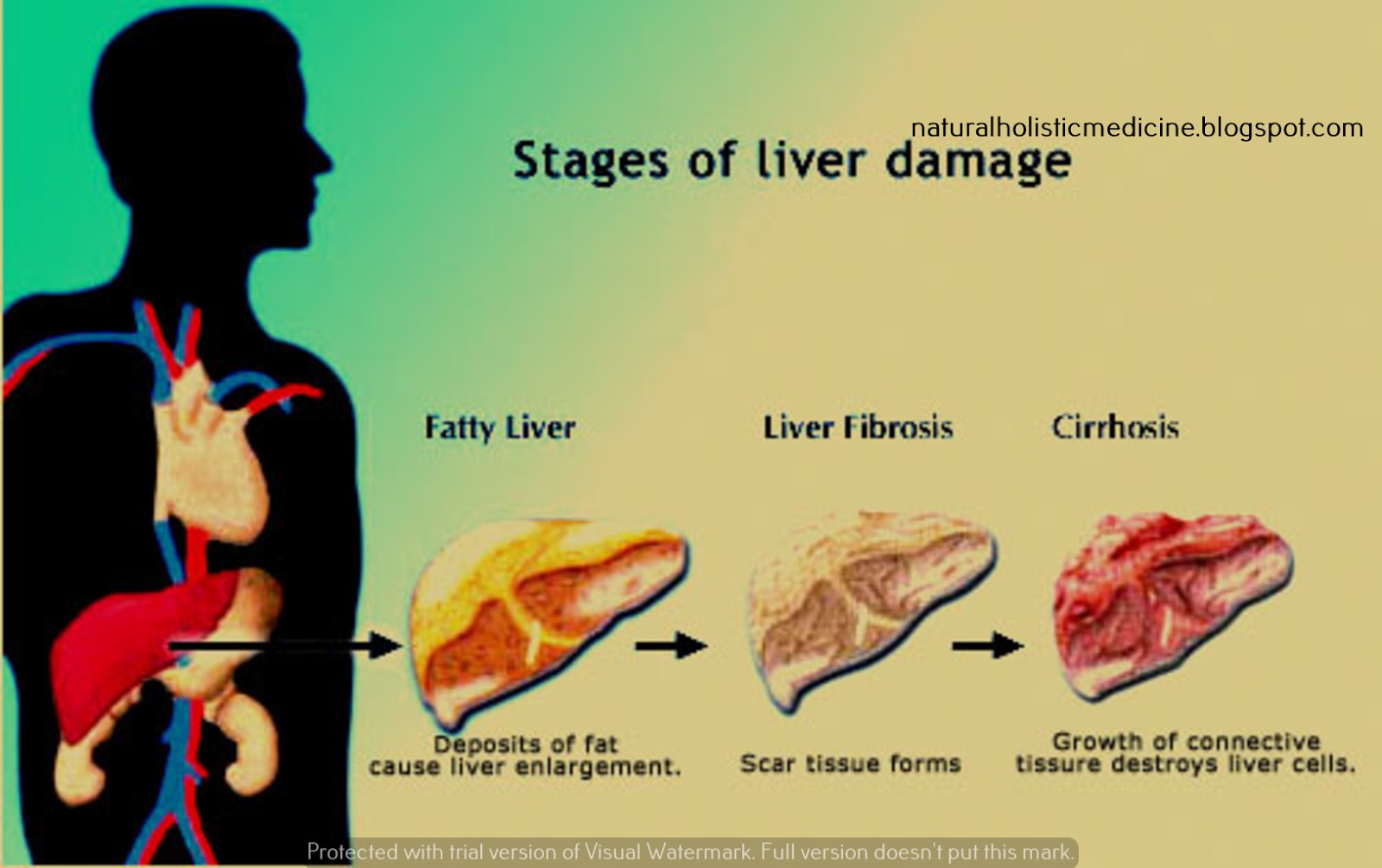
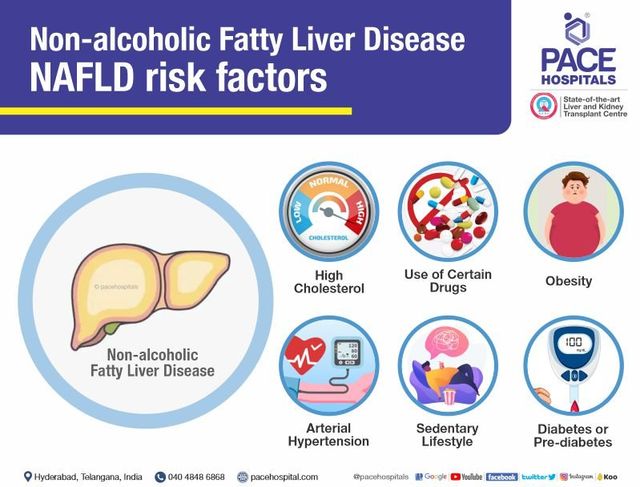
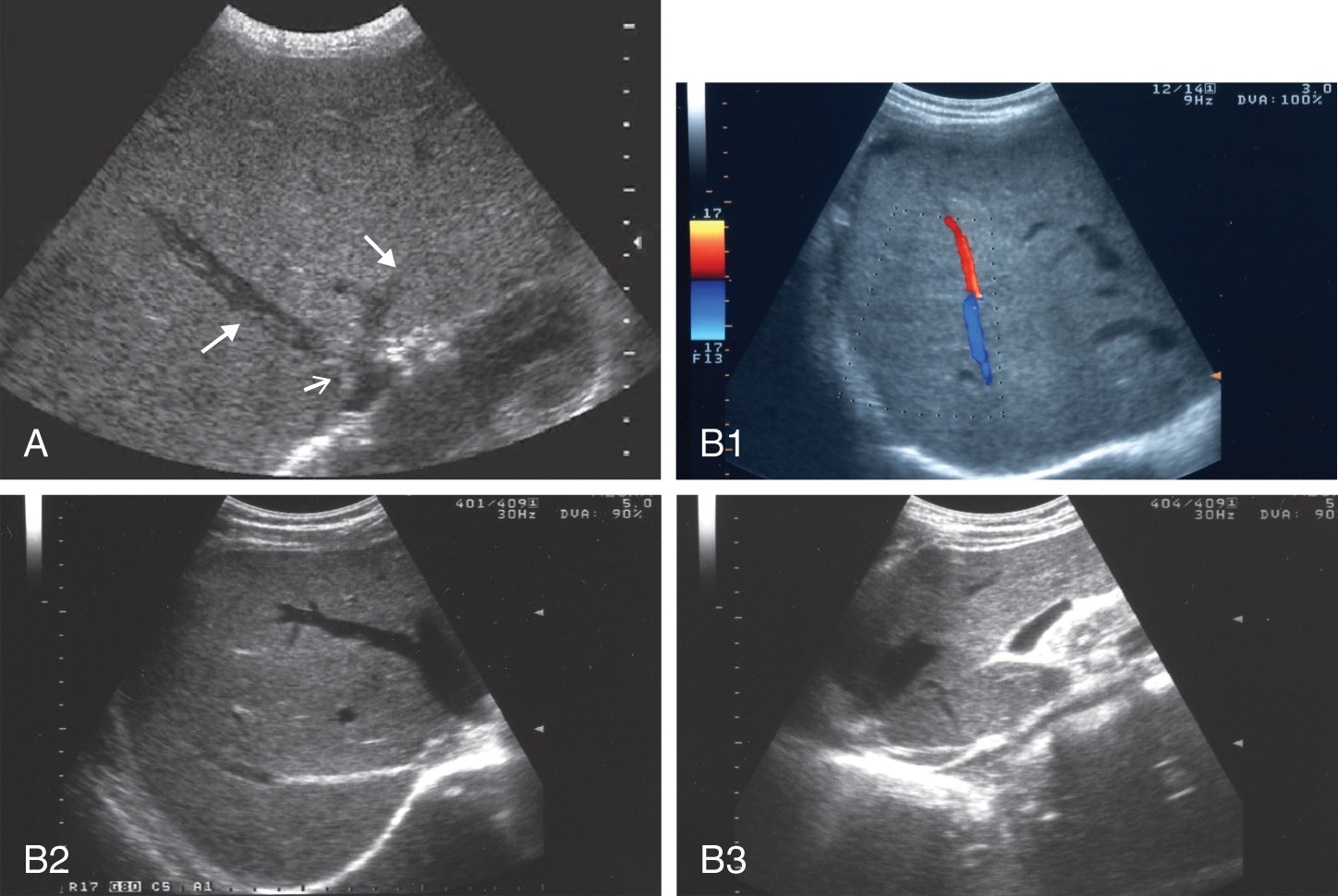
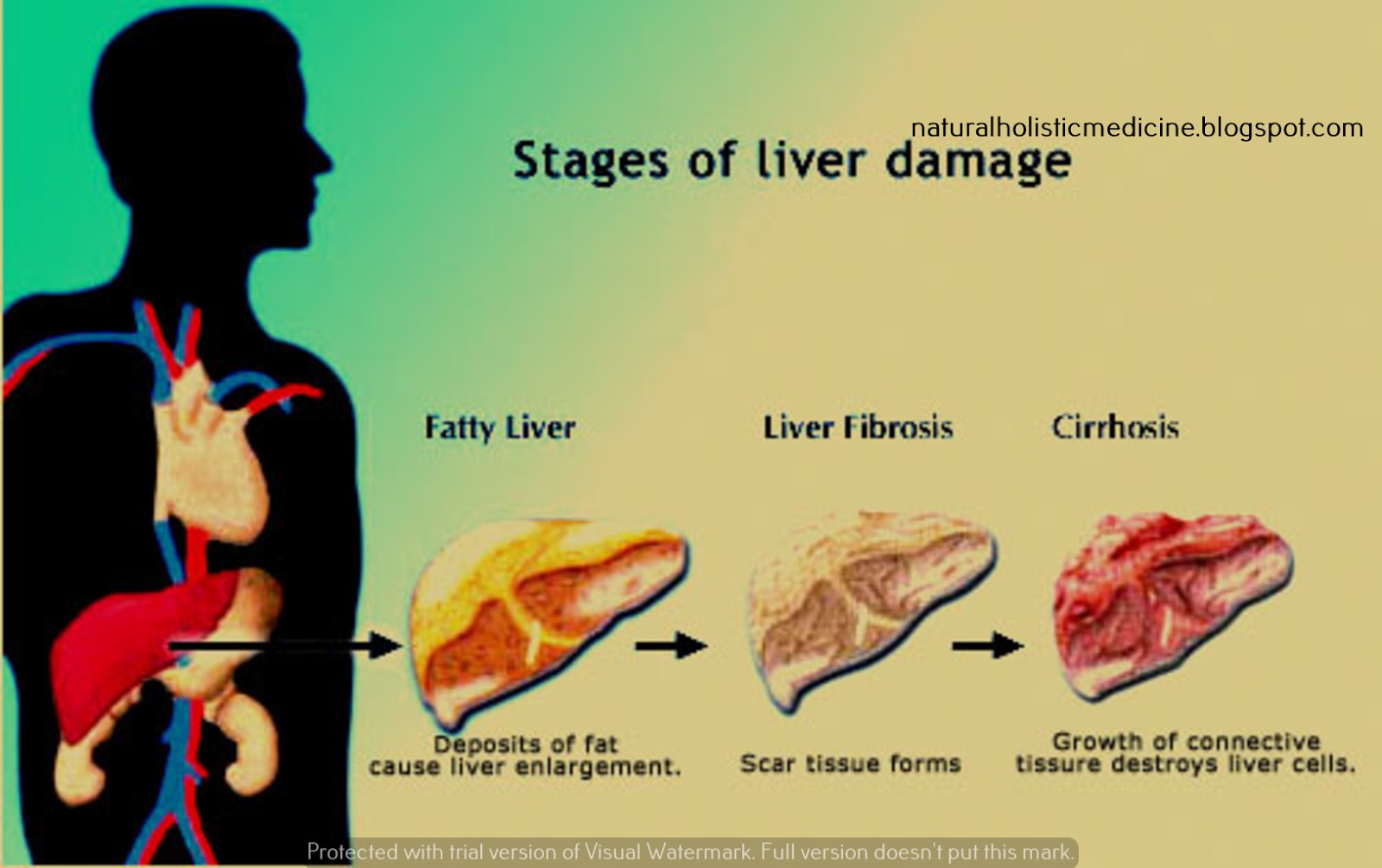
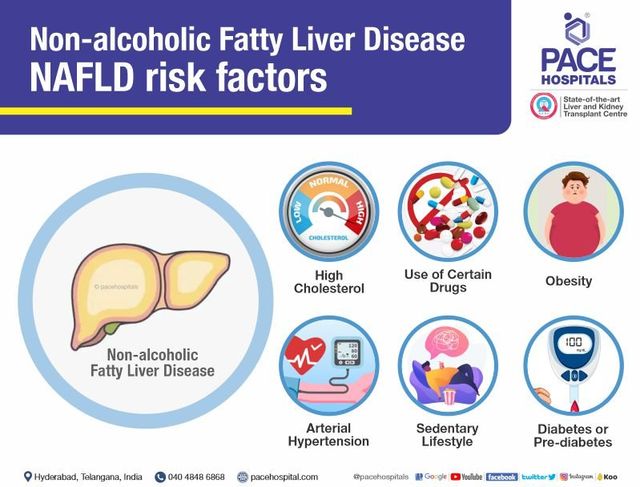
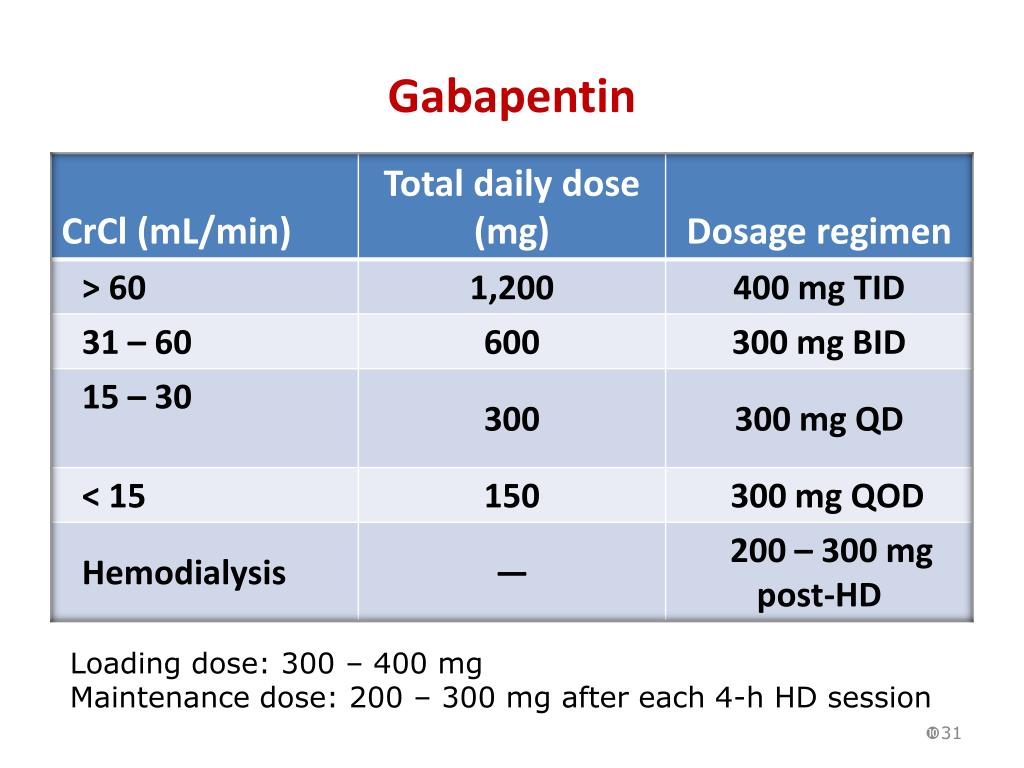
In patients who have severe or chronic pain and require narcotics (eg, with sickle-cell anemia, which causes chronic liver disease and is associated with chronic pain), management is quite complicated and often best done with the partnership of a pain management specialist. Pain management in patients with cirrhosis is a difficult clinical challenge for health care professionals, and few prospective studies have offered an evidence-based approach. In patients with end-stage liver disease, adverse events from analgesics are frequent, potentially fatal, and often avoidable. Severe complications from analgesia in these patients include hepatic encephalopathy This class, which includes gabapentin and pregabalin, is not metabolized by the liver. Therefore, risks in patients with advanced liver disease are not greatly increased. However, there are case reports of pregabalin‐induced hepatoxicity. 4 Gabapentin and pregabalin are renally excreted, so dosages need to be adjusted for renal failure. With a cautious approach including slow dose up-titration and careful monitoring, effective analgesia can be achieved in most cirrhotic patients without significant side effects or decompensation of their liver disease. Paracetamol is safe in patients with chronic liver disease but reduced doses of 2-3 grams daily is recommended for long-term use. Liver injury may occur from paracetamol overdose 16 and in rare cases from repeated therapeutic doses in patients with glutathione deficiency risk factors such as malnutrition, chronic illness, or chronic alcohol ingestion. 17 Although the half-life of paracetamol may be prolonged in patients with chronic liver disease, CYP450 content is not Several studies demonstrated that chronic treatment with gabapentin may alter liver and renal homeostasis (Grunze et al., 1998; Daoud et al., 2004; Lasso-de-la-Vega et al., 2001); however, the One case involved a 60-year-old male taking 2400 milligrams of gabapentin for chronic pain, who developed DILI with a mixed hepatocellular and cholestatic pattern . The removal of gabapentin and the administration of steroids resulted in the normalization of liver test abnormalities. In this clinical scenario, bromides, levetiracetam, gabapentin, and vigabatrin constitute safe choices. For the treatment of status epilepticus, levetiracetam and lacosamide, available in intravenous preparations, are good second-line therapies after benzodiazepines fail to control seizures. •Liver disease can enhance the risk of adverse reactions of medications •No test can determine drug dosing in patients with hepatic impairment •Most drugs can be used safely •Drug prescribing should be carefully done in patients with severe liver disease (cirrhosis), especially dose with jaundice, ascites or encephalopathy A recent case report from Sweden determined that pregabalin was a probable cause of acute liver failure in a 61-year-old healthy man with no previous liver disease. 47 Although this may have been an idiosyncratic event because no further case reports have been published in the literature, clinicians must be mindful of the increased risk of drug Class: Non-opioid Recommendations in liver disease: Oral route, use with caution & avoid intravenous route. Comments: Can opt for a sub-maximal dose 500mg -1g TDS-QDS especially if at higher risk for paracetamol toxicity & consider dose reduction if on for >7 days* Pain management is often a challenge for healthcare professionals, but it remains a very important component of providing quality patient care and is a common factor in patient satisfaction. 5 A high prevalence of pain has been found among patients with chronic liver disease, reported between 32% and 77%. 6-8 Pain and opioid-based pain regimens No cases of acute liver failure or chronic liver injury due to gabapentin have been described. There is no information about cross reactivity with other compounds having similar structure (pregabalin). We would like to show you a description here but the site won’t allow us. Gabapentin (Neurontin) usually isn’t bad for your liver or kidneys. In most cases, it has little effect on these organs. In rare instances, gabapentin can cause DRESS (drug reaction with eosinophilia and systemic symptoms) syndrome. INTRODUCTION. Chronic pain in cirrhosis is common, poorly characterized, and uniquely morbid. Reported by 40%–79% of patients with cirrhosis, 1,2 it is a key driver of poor functional status and quality of life. 3–6 Patients with cirrhosis and chronic pain also have significantly greater health care use. 7 Pain management in cirrhosis can be complex because of challenges in diagnosis and We are reporting a case of drug induced liver injury (DILI) secondary to gabapentin therapy with risk factors for underlying non-alcoholic fatty liver disease (NAFLD). In considering acetaminophen treatment in patients with chronic liver disease, the main variables to be concerned about are: what affect liver disease has on CYP2E1 levels, the patient’s probable glutathione stores, and the half life of acetaminophen itself. Get the latest pain assessments and treatment approaches. The aim of this double-blind, randomized, placebo-controlled trial was to study the effect of gabapentin on the perception of pruritus and its behavioral manifestation, scratching, in cholestasis. The participants were 16 women with chronic liver disease and chronic pruritus. There are potential harms associated with many of the common classes of analgesics (e.g. acetaminophen, NSAIDs, opioids) in this population as many of these agents are largely metabolized by the liver. 2. Liver disease is not a single disease entity, but rather ranges from acute liver injury, to chronic liver disease (e.g. nonalcoholic fatty
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |