Gallery
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |
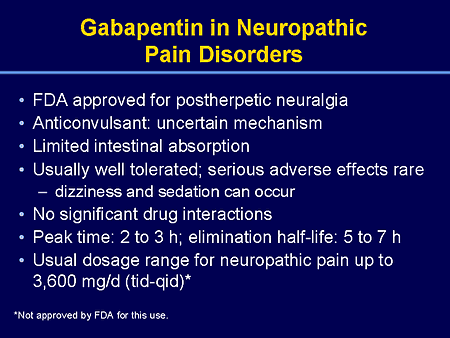
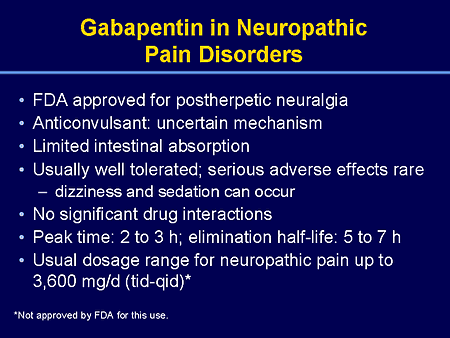
The Canadian Pain Society has advised selective cannabinoids as third-line agents for NeP. 7,8 It recommends close monitoring with long-term treatment and quotes history of psychosis as a contraindication. 7,8 NeuPSIG has recommended against use of cannabinoids because of weak evidence. 7 Gabapentin reduces neuropathic pain by < 1 point on a 0-10 point scale and benefits about 15% of carefully selected patients (NNT=6-8). A similar proportion of people suffer harm (NNH=8). A test of benefit/harm can be made after 1-2 days at a low dose (100-900 mg/day). Benefit is unlikely to increase with higher doses or longer treatment. A total of 14 RCTs with 3545 patients were included in this study, including 926 in the pregabalin treatment group, 1256 in the gabapentin treatment group, and 1363 in the placebo control group. Pregabalin was better than gabapentin in alleviating pain and improving the global perception of change in pain and sleep (P < 0.05). For people with neuropathic pain. Gabapentin at a dose of 1800 to 3600 mg daily (1200 to 3600 mg gabapentin encarbil) can provide good levels of pain relief to some people with postherpetic neuralgia and peripheral diabetic neuropathy. Evidence for other types of neuropathic pain is very limited. Gabapentin is a drug that has been widely used in the treatment of chronic pain states. Despite its widespread usage, it is only recently that light has been shed on the mechanism of action of this agent. In the current review, the authors document the pharmacological, biochemical and molecular info Gabapentin is FDA approved for pain management of a limited number of neuropathic pain conditions; Gabapentin is widely used off-label for various chronic pain conditions and for the treatment of acute pain, making it now one of the most commonly described analgesic drugs Gabapentin (GBP) is a Health Canada approved antiepileptic drug. 5 In the UK, GBP is licensed for the treatment of peripheral and central neuropathic pain in adults and in the US it is marketed for post-herpetic neuralgia (PHN). 3 The mechanism of action for GBP relates to its ability to bind with high-affinity to the alpha-2-delta subunit of vo Gabapentin and pregabalin are often considered first line treatment options for various neuropathic pain conditions. The purpose of this retrospective cohort study was to compare clinically meaningful pain reduction and other relevant outcomes among patients prescribed either gabapentin or pregabali The National Institute of Clinical Excellence (NICE) guidelines on the management of neuropathic pain recommend gabapentin, pregabalin, amitriptyline or duloxetine as the initial choice of treatment for neuropathic pain with the exception of trigeminal neuralgia. 1 The guideline development group found that gabapentin was the most cost Background: Few direct head-to-head comparisons have been conducted between drugs for the treatment of diabetic peripheral neuropathic pain (DPNP). Approved or recommended drugs in this indication include duloxetine (DLX), pregabalin (PGB), gabapentin (GBP) and amitriptyline (AMT). Introduction and hypothesis: Chronic pelvic pain (CPP) affects 2.1-24% of women, causing physical and psychological damage to women around the world. Based on the efficacy of gabapentin in the treatment of chronic pain, we conducted this study to evaluate the efficacy and safety of gabapentin in reducing pain in women with CPP. Gabapentin is used to control seizures, to treat nerve pain that can happen after having had shingles, and to treat a condition called restless legs syndrome. In addition to these FDA-approved uses, doctors sometimes prescribe gabapentin off-label. Gabapentin is a novel drug used for the treatment of postoperative pain with antihyperalgesic properties and a unique mechanism of action, which differentiates it from other commonly used drugs. Various studies have shown that perioperative use of gabapentin reduces postoperative pain. Authors' conclusions: Gabapentin at doses of 1800 mg to 3600 mg daily (1200 mg to 3600 mg gabapentin encarbil) can provide good levels of pain relief to some people with postherpetic neuralgia and peripheral diabetic neuropathy. Evidence for other types of neuropathic pain is very limited. Several studies have evaluated the efficacy of gabapentin and pregabalin in the treatment of neuropathic pain, yielding contradictory results. On one hand, it has been observed that gabapentin is more effective, especially at higher doses, compared to pregabalin (8, 9). This paper reviews the pharmacology and clinical effectiveness of gabapentin in the treatment of neuropathic pain. Gabapentin has antihyperalgesic and antiallodynic properties but does not have significant actions as an anti-nociceptive agent. Its mechanisms of action appear to be a complex synergy Gabapentin is approved to treat seizures and postherpetic neuralgia, a type of nerve pain from shingles. It is thought to work by changing how nerves send messages to your brain. It is also used off-label to treat other neuropathic pain conditions. Objectives: Gabapentin was initially developed as an antiepileptic drug but was later discovered to be an effective treatment of neuropathic pain. Gabapentin has been successfully used for the treatment of multiple neuropathic pain syndromes such as diabetic neuropathy and postherpetic neuralgia. Gabapentin is used to treat postherpetic neuralgia, a type nerve pain that can occur due to an outbreak of shingles, and restless legs syndrome (RLS), an uncomfortable urge to move your legs around, often at night. Objective: To assess the efficacy and safety of gabapentin in patients with fibromyalgia. Methods: A 12-week, randomized, double-blind study was designed to compare gabapentin (1,200-2,400 mg/day) (n=75 patients) with placebo (n=75 patients) for efficacy and safety in treating pain associated with fibromyalgia.
Articles and news, personal stories, interviews with experts.
Photos from events, contest for the best costume, videos from master classes.
 |  |
 |  |
 |  |
 |  |
 |  |
 |  |